Hong Kong Med J 2025;31:Epub 21 May 2025
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Roles of unmet supportive care needs, supportive
cancer care service disruptions, and COVID-19–related perceptions in psychological distress among recently diagnosed breast cancer survivors in Hong Kong
Nelson CY Yeung, PhD1; Stephanie TY Lau, BSSc1; Winnie WS Mak, PhD2; Cecilia Cheng, PhD3; Emily YY Chan, PhD1; Judy YM Siu, PhD4; Polly SY Cheung, PhD5
1 The Jockey Club School of Public Health and Primary Care, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR, China
2 Department of Psychology, The Chinese University of Hong Kong, Hong Kong SAR, China
3 Department of Psychology, The University of Hong Kong, Hong Kong SAR, China
4 Department of Applied Social Sciences, Faculty of Health and Social Sciences, The Hong Kong Polytechnic University, Hong Kong SAR, China
5 Hong Kong Breast Cancer Foundation, Hong Kong SAR, China
Corresponding author: Prof Nelson CY Yeung (nelsonyeung@cuhk.edu.hk)
Abstract
Introduction: Receiving a cancer diagnosis and
living with breast cancer can be particularly stressful
during pandemic situations. This study examined
how cancer care service disruptions, unmet
supportive care needs (SCNs), and coronavirus
disease 2019 (COVID-19)–related perceptions were
associated with psychological distress among Hong
Kong breast cancer survivors (BCS) during the
COVID-19 pandemic.
Methods: A total of 209 female BCS diagnosed since
January 2020 (ie, the start of the COVID-19 pandemic
in Hong Kong) were recruited from the Hong Kong
Breast Cancer Registry to complete a cross-sectional
survey measuring the aforementioned variables.
Results: Multivariable logistic regression analysis
indicated that unmet physical/daily living needs (odds
ratio [OR]=1.03; P=0.002), unmet psychological
needs (OR=1.06; P<0.001), and perceived severity
of COVID-19–related health consequences in BCS
(OR=1.67; P=0.02) were significantly associated
with moderate-to-severe psychological distress.
However, cancer treatment/supportive care service
disruptions, fear of COVID-19, and unmet SCNs
in patient care/health system information/sexual
domains were not significant contributors (P=0.77-0.89).
Conclusion: Half of the BCS in Hong Kong
experienced substantial psychological distress during
the pandemic. Survivors with higher levels of unmet SCNs in physical/daily living and psychological
domains, as well as those with greater perceived
severity of COVID-19–related health consequences,
were more likely to experience moderate-to-severe
psychological distress. These findings suggest that
efforts to address specific unmet SCNs and risk
perceptions are important for reducing psychological
distress among BCS during pandemic situations.
New knowledge added by this study
- At least 50% of breast cancer survivors (BCS) in Hong Kong experienced a moderate-to-severe level of psychological distress during the coronavirus disease 2019 (COVID-19) pandemic.
- Unmet needs in physical/daily living and psychological domains were associated with moderate-to-severe psychological distress among local BCS.
- Perceived COVID-19 severity, but not fear of COVID-19, was associated with moderate-to-severe psychological distress among local BCS.
- To address the physical and psychological needs of BCS, healthcare providers should consider how telemedicine services can provide remote support for symptom management and psychological counselling.
- The provision of up-to-date educational materials can help alleviate distress and risk perceptions related to COVID-19.
Introduction
The coronavirus disease 2019 (COVID-19)
pandemic has had a broad public health impact on
global populations. Pandemic-control measures
(eg, social distancing regulations and changes in
hospital services) have affected both the general
population and individuals with chronic diseases
(including cancer survivors).1 A recent meta-analysis
found that 53.9% of cancer patients (n=27
590) experienced high levels of distress during the
COVID-19 pandemic2; breast cancer survivors
(BCS) reported highest prevalence of post-traumatic
stress symptoms (52.3%) among all groups of cancer
patients.2 In Hong Kong, 40% of cancer survivors
reported feeling anxious and depressed during
COVID-19.3 However, factors associated with
psychological distress among local BCS during the
pandemic have been understudied.
After completion of active treatment, BCS
require a range of supportive cancer care services for
rehabilitation. To prioritise resources for managing
COVID-19, some oncology services were postponed
in Hong Kong.4 Among a heterogeneous sample
of cancer survivors in Hong Kong,3 <10% reported
that the COVID-19 pandemic had affected their
hospital treatments or follow-ups. Despite this
low prevalence, the potential negative impacts of such disruptions on cancer survivors’ well-being
should not be ignored. A systematic review found
that delays or changes in treatment plans were
associated with high levels of psychological distress,
above and beyond the contributions of other socio-demographic
factors.5 Similarly, BCS in the United
Kingdom who experienced disrupted oncology
services reported worse emotional well-being.6 In
China, a 3-week treatment delay was significantly
associated with increased psychological symptoms
among BCS.7 Based on these findings, we speculated
that cancer treatment and supportive care service
disruptions would be associated with greater
psychological distress among BCS in Hong Kong.
Given that cancer survivors are more
aware of the risks of infection compared with the
general population,8 their emotional reactions and
perceptions towards COVID-19 also contribute
to their well-being. Due to the rapidly changing
pandemic situations caused by different variants
of the COVID-19 virus, cancer survivors tend to
experience fear of contracting COVID-19 and
express concerns about the severity of its negative
health impacts on cancer prognosis.9 10 Based
on a review of 51 studies (19.5% conducted in
Asia), COVID-19–related fear and worries were
associated with psychological distress among cancer
survivors.11 However, a recent study in Hong Kong
showed that 49.7% of cancer survivors did not feel
worried about contracting COVID-19,3 and they did
not consider themselves to experience more negative
consequences of contracting COVID-19 compared
with the general population.12 Whether COVID-19–related fear and risk perceptions are associated with
psychological distress among BCS in Hong Kong has
yet to be explored.
The COVID-19 pandemic has led to unmet
supportive care needs (SCNs) among BCS. According
to Fitch’s Supportive Care Needs Framework,13 a
medical diagnosis affects people’s abilities to meet
their own needs across life domains; unmet needs
may result in worse adjustment outcomes. It is
common for cancer survivors to report physical,
psychological, social, and health system–related
unmet needs during COVID-19.14 A longitudinal
survey of Asian and Asian American cancer survivors
revealed a significant increase in psychological and
healthcare access needs during COVID-19.15 In
Hong Kong, higher levels of unmet SCNs were
identified in the health system/information,
psychological, and patient care/support domains
among cancer survivors during COVID-19.3 In
Australia, unmet SCNs were associated with greater
psychological distress among haematological
and gynaecological cancer survivors.16 However,
research examining the associations between unmet
SCNs and BCS’ psychological distress has been
sparse.
This study examined factors associated with
psychological distress among Hong Kong BCS during
COVID-19. We hypothesised that different domains
of unmet SCNs, disruptions in cancer treatment
and supportive cancer care services, increased fear
of COVID-19, and a stronger belief that COVID-19
would cause more severe health consequences for
BCS (compared with the general population) were
associated with greater psychological distress.
Methods
Prospective participants were recruited from
the Hong Kong Breast Cancer Registry, the most
representative monitoring system for BCS in Hong
Kong.17 Based on the cancer registry data, those
fulfilling the inclusion criteria were invited to
participate in a cross-sectional survey. Breast cancer
survivors eligible for the study were required to be:
≥18 years old, diagnosed with stages 0 to III cancer
since January 2020, in active treatment, able to read
Chinese and communicate in Cantonese, and able to
provide informed consent.
Among 946 BCS contacted, 409 were
unreachable, 23 were ineligible, and 227 were
uninterested in the study. With verbal consent
given over the phone, those who were eligible and
interested in the study (n=287) received a mail
package enclosing a cover letter explaining the study
details, a consent form, a questionnaire packet, a
stamped return envelope, and a thank-you card. After
they had provided consent, participants completed
the survey at home. Participants were compensated
with supermarket vouchers (worth HK$100) for
their time upon returning the completed survey. The
study was conducted between June and December
2022. Overall, 209 completed surveys were returned
(from 287 sent), yielding a completion rate of 72.8%.
Measurement
Psychological distress
The one-item National Comprehensive Cancer
Network Distress Thermometer was used to
assess participants’ psychological distress over
the past week.18 On an 11-point Likert scale, the
thermometer ranged from 0 (no distress) to 10
(extreme distress).19 A higher score indicated a
higher level of psychological distress. A cut-off point
of ≥4 indicated moderate-to-severe distress.20 The
Chinese version of the Distress Thermometer has
demonstrated reliability and validity among Chinese
cancer patients.21
Cancer treatment and supportive cancer care
service disruptions during coronavirus disease
2019
Participants’ experiences of any postponement or
cancellation of various types of cancer treatments (eg, surgery and adjuvant therapies) and supportive
cancer care services (eg, psychological counselling
and peer support groups) during COVID-19 were
measured (no=0, yes=1).
Supportive care needs
The Chinese version of the 34-item Short-Form
Supportive Care Needs Questionnaire was used to
measure five domains of SCNs (namely, physical/daily living, psychological needs, patient care and
support, sexuality, and health system/information
needs) over the past month. On a five-point scale (no
need–not applicable, no need–satisfied, low need,
moderate need, high need), items were scored using
standardised guidelines.22 Higher scores indicated
higher levels of unmet SCNs. The scale has shown
reliability and validity among Hong Kong cancer
survivors.3 22
Fear of coronavirus disease 2019
The Chinese version of the seven-item Fear
of COVID-19 Scale was adapted to measure
participants’ fear of COVID-19.23 On a five-point
scale (1=strongly disagree, 5=strongly agree),
a higher mean score indicated greater fear of
COVID-19 (eg, “My heart races or palpitates when I
think about getting COVID-19”; Cronbach’s α=0.88).
The scale has demonstrated reliability and validity in
a Chinese general population.23
Perceived severity of consequences of coronavirus
disease 2019 on breast cancer survivors
A single item was developed to measure participants’
perception of the severity of COVID-19 health
consequences for BCS (ie, “COVID-19 can cause
more severe health consequences in BCS than in the
general population”). Responses were recorded on
a five-point scale (1=strongly disagree, 5=strongly
agree); higher scores indicated greater perceived
severity.
Clinical and socio-demographic characteristics
Participants self-reported the following
characteristics: (1) socio-demographic information;
(2) treatment-related variables (surgery undergone,
treatments being received or completed, and time
since last treatment); and (3) breast cancer–related
variables (eg, stage at diagnosis and time since
diagnosis).
Planned analyses
Descriptive statistics and bivariate correlations
among the variables were computed. Multivariable
logistic regressions were used to examine
associations between independent variables
and moderate-to-severe levels of psychological distress (binary-coded), based on the suggested
Distress Thermometer cut-off of ≥4. Simple logistic
regression analysis was used to assess how individual
variables (including socio-demographic/cancer-related
variables, cancer treatment/supportive
cancer care service disruptions, unmet SCNs, fear
of COVID-19, and COVID-19 risk perception)
were associated with psychological distress. Odds
ratios (ORs) were obtained by separately fitting each
variable against psychological distress.24 Significant
variables in the simple analyses were then entered
into a multivariable logistic regression model using
the enter method. These analyses were performed
using SPSS (Windows version 26.0; IBM Corp,
Armonk [NY], US). P values <0.05 were considered
statistically significant.
Sample size calculation
Based on prior studies regarding BCS’ psychological
distress,24 25 we assumed a similar prevalence of
30% for moderate-to-severe levels of psychological
distress in our target population. With α=0.05 (two-tailed)
and a statistical power of 80%, a sample
size of 203 would be sufficient to detect an OR of
1.56 for the key independent variables (G*Power
version 3.1.2).26 The current sample size (n=209)
was sufficient to detect the expected effect sizes with
adequate statistical power.
Results
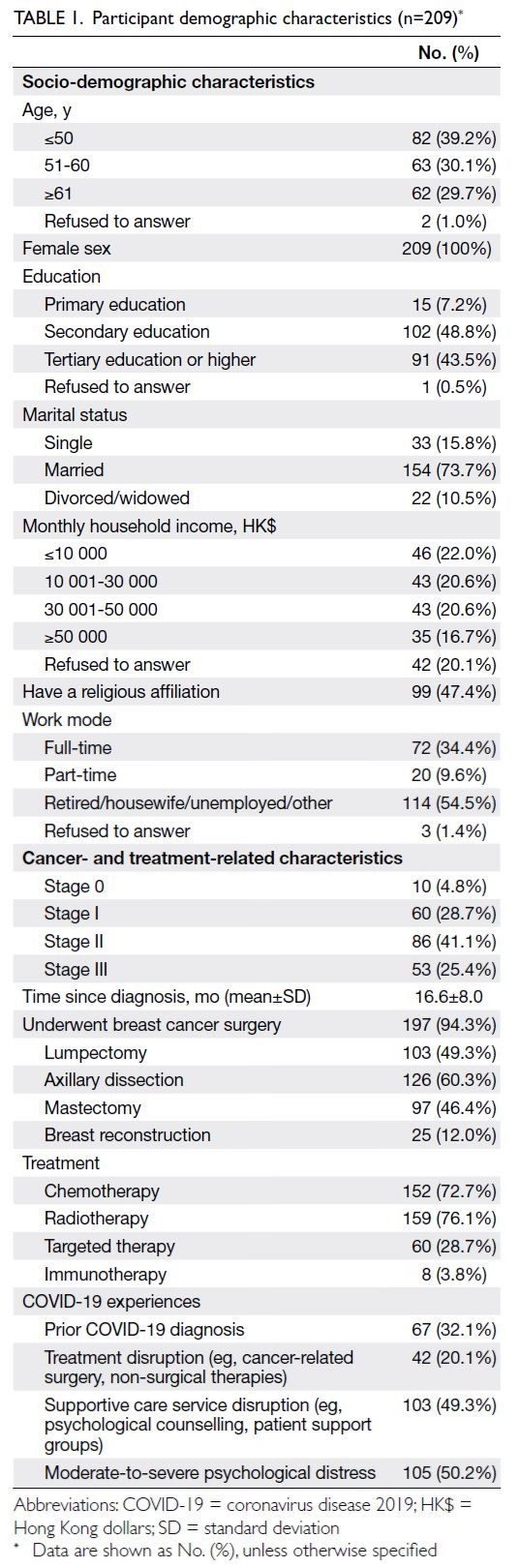
Participant characteristics
Among the 209 participants, 69.3% were aged ≤60
years. Regarding cancer-related characteristics,
4.8%, 28.7%, 41.1%, and 25.4% were diagnosed
with Stage 0, Stage I, Stage II, and Stage III breast
cancer, respectively. Most participants (94.3%) had
undergone breast cancer surgery. Most had also
received chemotherapy (72.7%) and radiotherapy
(76.1%). The average time since diagnosis was 16.6
months (standard deviation=8.00). During COVID-19, 32.1% of participants had a prior diagnosis of
COVID-19; 20.1% experienced cancer treatment
disruptions (eg, surgery/adjuvant therapies); and
49.3% experienced supportive cancer care service
disruptions (eg, psychological counselling, patient
support groups). Based on a Distress Thermometer
score ≥4, 50.2% of participants reported a moderate-to-severe level of psychological distress (Table 1).
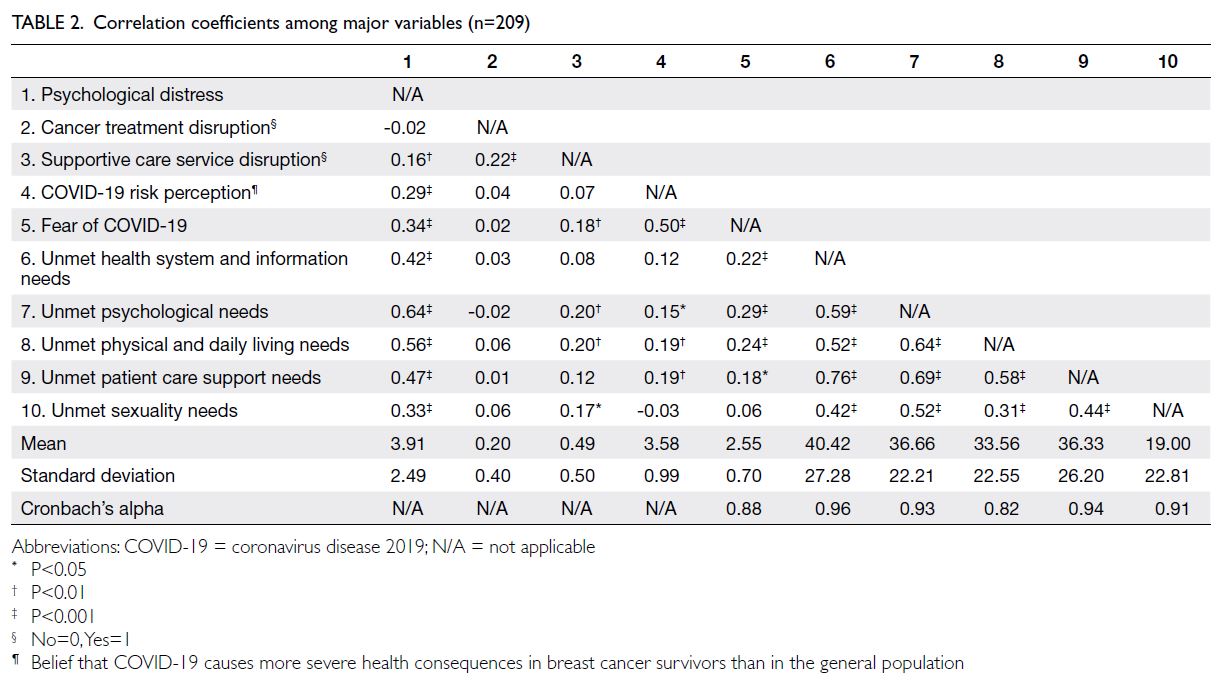
Correlations between major variables and
psychological distress
Based on the correlation analysis results (Table 2), participants who had experienced supportive
cancer care service disruption, perceived greater
fear of COVID-19, and held a stronger belief that
COVID-19 causes more severe health consequences
in BCS tended to report increased psychological distress (sample correlation coefficients=0.16-0.34;
all P<0.01). All five domains of unmet SCNs were
associated with increased psychological distress
(sample correlation coefficients=0.33-0.64; all P<0.001).
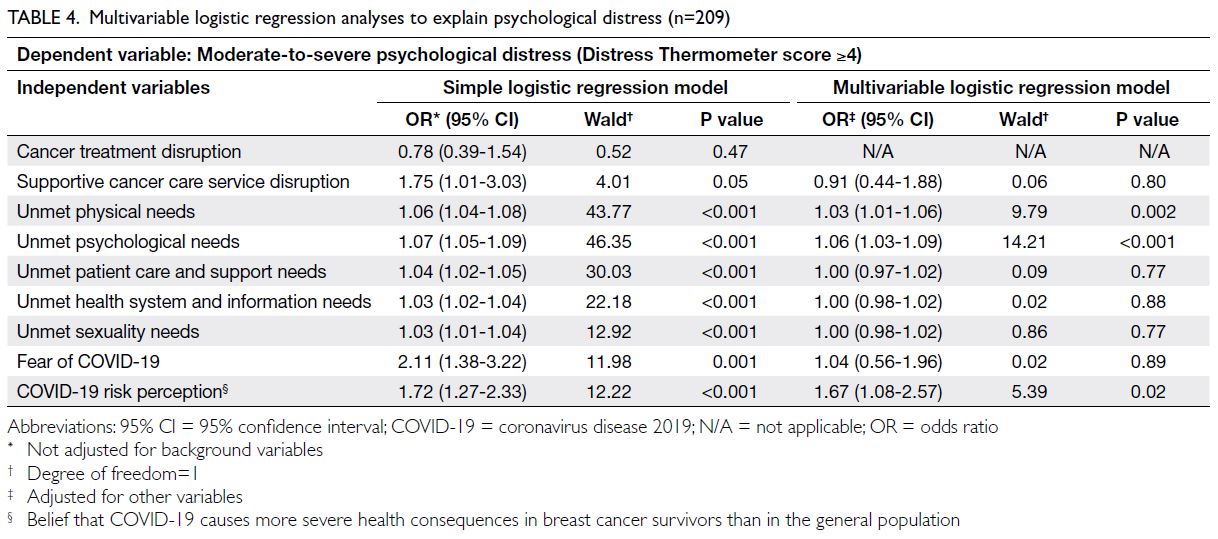
Logistic regression analyses
In the simple logistic regression analyses (Table 3), no background variables showed significant
associations with psychological distress; accordingly,
adjustments for those variables were not included
in the final multivariable regression model. On the
other hand, all domains of unmet SCNs (ORs=1.03-1.07; all P<0.001), cancer supportive care service
disruption (OR=1.75; P=0.05), fear of COVID-19
(OR=2.11; P=0.001), and the perception that
COVID-19 causes more severe health consequences
in BCS (OR=1.72; P<0.001) were associated with
moderate-to-severe psychological distress (Table 4). The multivariable logistic regression results
indicated that only unmet physical needs (OR=1.03;
P=0.002), unmet psychological needs (OR=1.06;
P<0.001), and perceived severity of COVID-19–related health consequences in BCS (OR=1.67;
P=0.02) were associated with moderate-to-severe
psychological distress (Table 4).
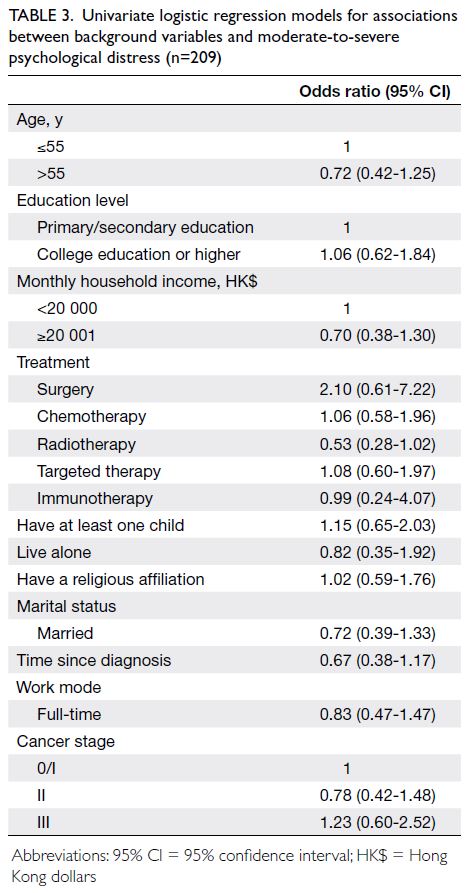
Table 3. Univariate logistic regression models for associations between background variables and moderate-to-severe psychological distress (n=209)
Discussion
At least 50% of BCS in Hong Kong experienced
a moderate-to-severe level of distress during COVID-19. This prevalence was comparable to
that of gynaecological cancer survivors in Turkey,27
but lower than that of sarcoma patients in Italy.28
Discrepancies in prevalence might be attributed to
varied pandemic situations across regions, including
differences in survey periods, cancer types, and
specific pandemic-control measures. Future
research could investigate how these factors jointly
contribute to BCS’ psychological distress. Among the
studied variables, multivariable logistic regression
analysis revealed that higher levels of unmet SCNs
in physical and psychological domains, along with
a stronger belief that COVID-19 could cause more
severe health consequences in BCS, were associated
with greater psychological distress among BCS in
Hong Kong.
Supportive care service disruption was
associated with breast cancer survivors’
psychological distress
We found that 20.1% and 49.3% of BCS experienced
cancer treatment and supportive cancer care
service disruptions, respectively, during COVID-19.
Only the disruption of supportive cancer care
services (but not cancer treatments) demonstrated
a significant univariate association with moderate-to-severe psychological distress. Previously, cancer
care service disruptions during COVID-19 were
associated with worse psychological outcomes
among BCS in the United Kingdom,6 Canada,29 and Ireland.30 Given that disruptions of supportive
cancer care services (but not cancer treatments)
were positively associated with unmet SCNs, the
absence of timely supportive care might make coping
with and living with cancer particularly difficult
during COVID-19.11 However, supportive cancer
care service disruption was no longer significant
in multivariable logistic regression analyses when
other independent variables were considered. This
finding implies that more proximal factors related to
BCS’ daily lives and challenges (eg, different domains
of unmet SCNs) had relatively greater prominence
in explaining psychological distress among BCS in
Hong Kong during COVID-19.
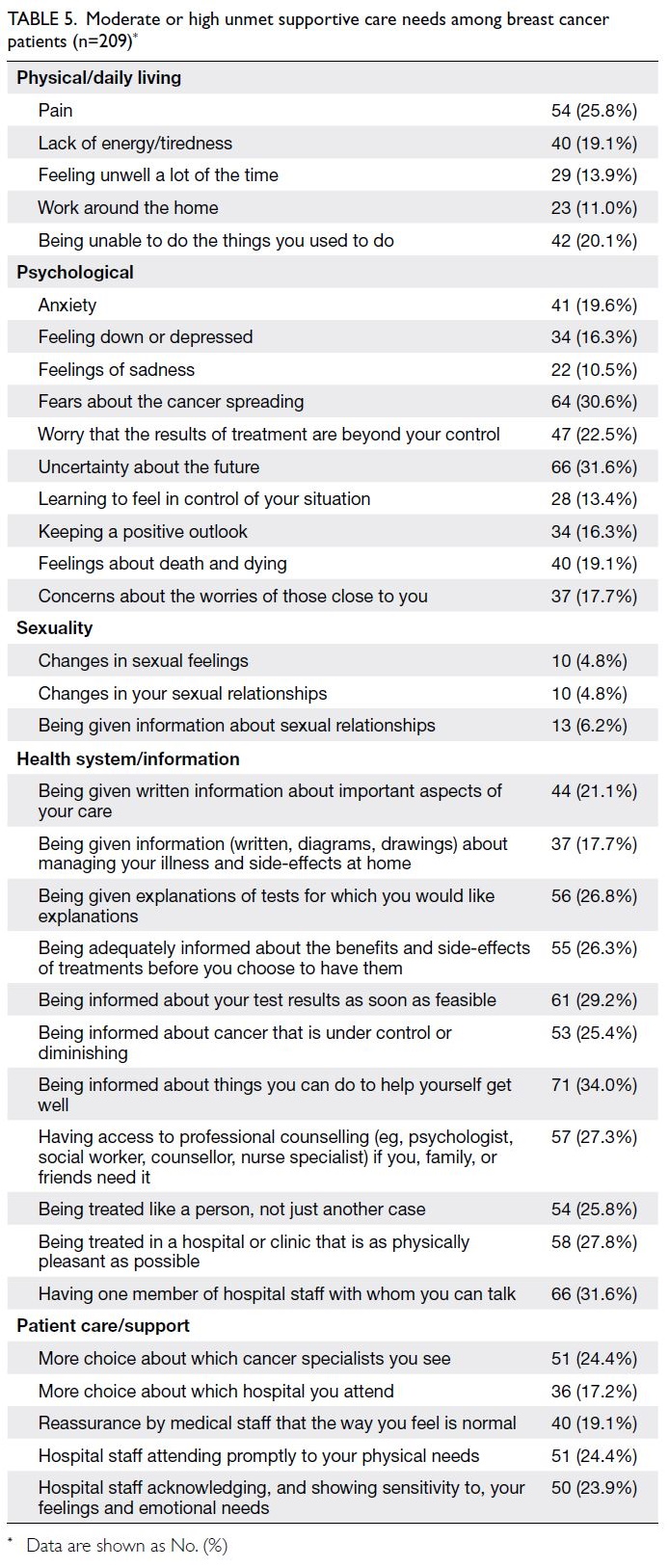
Unmet supportive care needs in relation
to breast cancer survivors’ psychological distress
Breast cancer survivors in Hong Kong reported
moderate levels of unmet SCNs across different
domains, with the highest score in the health system/information domain and the lowest score in the
sexuality domain (Table 5). These levels of unmet
SCNs were comparable to those reported by other
local cancer survivors in 2021.3 Our findings
showed that all five domains of unmet SCNs were
associated with moderate-to-severe psychological
distress, but only unmet SCNs in the psychological
and physical/daily living domains constituted
significant contributors in the final multivariable
logistic regression model (Table 4). These findings
were similar to a study conducted among survivors
of mixed cancer types (56.7% diagnosed within the
previous year) in Turkey.31 According to that study,31
conducted during COVID-19, all domains of unmet SCNs were correlated with depression/anxiety, but
only unmet SCNs in the psychological and physical/daily living domains independently contributed to
depression/anxiety in the multivariable analysis. In
contrast, among cancer survivors in Jordan (77%
diagnosed ≥6 years prior), all domains of unmet SCNs
during COVID-19 were independently associated
with quality of life.32 Given that our participants
were recently diagnosed BCS (with an average
time since diagnosis of 16.6 months; all diagnosed
after the COVID-19 pandemic began), they were
still in the process of coping with the reality of the
cancer diagnosis, the discomfort and side-effects
of treatment, uncertainties about the future, and
potential cancer recurrences. Considering the time
since diagnosis, the relative contributions of SCNs in
the psychological and physical/daily living domains
to psychological distress were particularly strong
among recently diagnosed BCS during COVID-19.
Coronavirus disease 2019–related risk
perception was associated with psychological distress
Fear of COVID-19 was associated with greater
psychological distress only in the simple analysis,
but not in the multivariable regression model.
Previously, fear of COVID-19 was associated
with greater psychological distress among cancer
survivors in the US33 and the general population in
Hong Kong34 during earlier phases of the COVID-19
pandemic in 2020 to 2021. Due to Hong Kong’s
unique experiences in successfully managing
prior pandemics (eg, the severe acute respiratory
syndrome and the H1N1 pandemics),35 pandemic
fatigue (ie, a state of emotional and physical
exhaustion resulting from prolonged anti-pandemic
measures) was observed during the fourth and fifth
waves of the pandemic in Hong Kong (2021-2022).36
Such fatigue was reflected in the lower levels of fear
of COVID-19 (ie, affective and physiological states
of anxiety and fear towards COVID-19) among our
sample surveyed in 2022, compared with the general
population surveyed in early 2021,34 using the same
measurement. This finding might explain why the
contribution of fear of COVID-19 to psychological
distress among local BCS was weaker than expected.
Conversely, we found that the perceived
severity of the health consequences of COVID-19
for BCS was a stronger contributor to psychological
distress than fear of COVID-19. Cancer and its
treatments (eg, chemotherapy) can weaken patients’
immune systems, and it is common for BCS to
believe that being immunocompromised might lead
to more severe health consequences if they contract
COVID-19.1 Risk perception has been associated
with coping behaviours. For example, a recent
study found that risk perception about COVID-19
was a stronger contributor to information-seeking behaviour among the general population in Hong
Kong than among their counterparts in China and
Taiwan.37 We expected that this phenomenon would
also be apparent among Hong Kong BCS. However,
health information about COVID-19 may not
always be tailored for cancer survivors or effectively
communicated through local mass media,1 which
could be associated with psychological distress
among BCS. To alleviate such COVID-19–related
risk perceptions, we recommend that health
organisations tailor health information and provide
counselling for cancer survivors through alternative
platforms (eg, social media and online forums).
Limitations
This study had several limitations. First, given
its cross-sectional design, it could not establish
causal relationships among the variables. Cancer
survivors’ risk perceptions about COVID-19 and
unmet SCNs are likely to change throughout the
course of their cancer journey. Future studies could
utilise longitudinal designs to better understand
the temporal relationships among variables and
psychological distress. Second, although the
Hong Kong Breast Cancer Registry is the most
comprehensive registry for BCS in Hong Kong, it
does not cover the entire BCS population due to its
voluntary enrolment system. The generalisability of
the findings to BCS in other countries with different
healthcare systems and pandemic situations should
be interpreted with caution. Third, other important
independent variables might contribute to BCS’
psychological distress. Studies have revealed that
additional daily COVID-19 stressors (eg, increased
responsibilities at home and difficulties obtaining
daily necessities) and coping strategies (eg,
catastrophising) may play key roles in explaining
psychological distress among cancer survivors.12 29
The inclusion of such variables could further improve
the explanatory power of the regression model.
Fourth, to reduce participant burden, we measured
risk perceptions related to COVID-19 using a self-developed
item. Specifically developed items are
commonly used as predictors of psychological
outcomes to capture nuances in the local COVID-19 context.38 However, researchers are encouraged
to confirm our findings using fully validated
instruments for the measurement of COVID-19 risk
perceptions.
Implications
This study highlights the importance of addressing
BCS’ unmet SCNs in the physical/daily living
and psychological domains, as well as their
risk perceptions of COVID-19, in relation to
psychological distress during the pandemic. To
address physical/daily living needs, survivors might need to engage in self-monitoring of health (eg,
reporting symptoms and metrics to healthcare
providers through patient portals). Psychological
well-being should be regularly monitored, and
communication between providers and survivors
should be maintained through virtual means. In
addition to information about cancer symptom
management, survivors should be provided with
accessible mental health services that can support
them in coping with the emotional impacts of their
diagnosis and treatment.39 Regarding COVID-19
risk perception, it may be beneficial to offer accurate
and up-to-date educational materials explaining
BCS’ risks associated with COVID-19 and how
they can protect themselves. Research suggests
that telehealth can empower survivors and provide
strategies for coping during unprecedented times.
A recent study in Iran indicated that a tele-nursing
intervention—including supportive telephone
calls with explanations about cancer, treatment
side-effects, symptom management, and self-care—reduced unmet SCNs among Iranian cancer
survivors undergoing chemotherapy.40 Researchers
should explore the applicability of such service
models in Hong Kong and other regions.
Conclusion
Half of BCS in Hong Kong experienced a moderate-to-severe level of psychological distress during
COVID-19. Efforts to address unmet SCNs in the
physical/daily living and psychological domains,
manage risk perceptions regarding health
consequences of COVID-19, and provide supportive
cancer care services through alternative modes
might help alleviate psychological distress among
BCS in future pandemic situations.
Author contributions
Concept or design: All authors.
Acquisition of data: NCY Yeung, STY Lau.
Analysis or interpretation of data: NCY Yeung, STY Lau.
Drafting of the manuscript: NCY Yeung, STY Lau.
Critical revision of the manuscript for important intellectual content: NCY Yeung.
Acquisition of data: NCY Yeung, STY Lau.
Analysis or interpretation of data: NCY Yeung, STY Lau.
Drafting of the manuscript: NCY Yeung, STY Lau.
Critical revision of the manuscript for important intellectual content: NCY Yeung.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This research was supported by the Health and Medical
Research Fund of the Health Bureau, Hong Kong SAR
Government (Ref No.: 18190061). The funder had no role in
the study design, data collection/analysis/interpretation, or
manuscript preparation.
Ethics approval
This research was approved by the Joint Chinese University of
Hong Kong–New Territories East Cluster Clinical Research
Ethics Committee, Hong Kong (Ref No.: 2021.286) and the
Hong Kong Breast Cancer Foundation. Informed consent
was obtained from all individual participants included in the
study.
References
1. Huang J, Wang HH, Zheng ZJ, Wong MC. Impact of the
COVID-19 pandemic on cancer care. Hong Kong Med J
2022;28:427-9. Crossref
2. Zhang H, Xu H, Zhang Z, Zhang Q. Efficacy of virtual
reality–based interventions for patients with breast cancer
symptom and rehabilitation management: a systematic
review and meta-analysis. BMJ Open 2022;12:e051808. Crossref
3. Cheung DS, Takemura N, Lui HY, et al. A cross-sectional
study on the unmet supportive care needs of cancer
patients under the COVID-19 pandemic. Cancer Care Res
Online 2022;2:e028. Crossref
4. Koczwara B. Cancer survivorship care at the time of the
COVID-19 pandemic. Med J Aust 2020;213:107-8.e1. Crossref
5. Prabani KI, Damayanthi HD. Quality of life, anxiety,
depression and psychological distress in patients with
cancer during the COVID 19 pandemic: a systematic
review. Intl Health Trends Perspect 2022;2:51-66. Crossref
6. Swainston J, Chapman B, Grunfeld EA, Derakshan N.
COVID-19 lockdown and its adverse impact on
psychological health in breast cancer. Front Psychol
2020;11:2033. Crossref
7. Wang Y, Yang Y, Yan C, et al. COVID-induced 3 weeks’
treatment delay may exacerbate breast cancer patient’s
psychological symptoms. Front Psychol 2022;13:1003016. Crossref
8. Slivjak ET, Fishbein JN, Nealis M, Schmiege SJ, Arch JJ.
Cancer survivors’ perceived vulnerability to COVID-19 and
impacts on cognitive, affective, and behavioral responses to
the pandemic. J Psychosoc Oncol 2021;39:366-84. Crossref
9. Glidden C, Howden K, Romanescu RG, et al. Psychological
distress and experiences of adolescents and young adults
with cancer during the COVID-19 pandemic: a cross-sectional
survey. Psychooncology 2022;31:631-40. Crossref
10. Shay LA, Allicock M, Li A. “Every day is just kind of
weighing my options.” Perspectives of young adult cancer
survivors dealing with the uncertainty of the COVID-19
global pandemic. J Cancer Surviv 2022;16:760-70. Crossref
11. Muls A, Georgopoulou S, Hainsworth E, et al. The
psychosocial and emotional experiences of cancer patients
during the COVID-19 pandemic: a systematic review.
Semin Oncol 2022;49:371-82. Crossref
12. Ng DW, Chan FH, Barry TJ, et al. Psychological distress
during the 2019 coronavirus disease (COVID-19)
pandemic among cancer survivors and healthy controls.
Psychooncology 2020;29:1380-3. Crossref
13. Fitch MI. Supportive Care Framework [in English, French].
Can Oncol Nurs J 2008;18:6-24. Crossref
14. Legge H, Toohey K, Kavanagh PS, Paterson C. The unmet
supportive care needs of people affected by cancer during
the COVID-19 pandemic: an integrative review. J Cancer
Surviv 2023;17:1036-56. Crossref
15. Wang K, Ma C, Li FM, et al. Patient-reported supportive
care needs among Asian American cancer patients.
Support Care Cancer 2022;30:9163-70. Crossref
16. Zomerdijk N, Jongenelis M, Short CE, Smith A, Turner J,
Huntley K. Prevalence and correlates of psychological
distress, unmet supportive care needs, and fear of cancer
recurrence among haematological cancer patients
during the COVID-19 pandemic. Support Care Cancer
2021;29:7755-64. Crossref
17. Hong Kong Breast Cancer Foundation. Hong Kong Breast
Cancer Registry Report No. 11. 2019. Available from:
https://www.hkbcf.org/en/our_research/main/468/. Accessed 26 May 2023.
18. National Comprehensive Cancer Network: Distress
Thermometer Tool Translations. Available from: https://www.nccn.org/global/what-we-do/distress-thermometer-tool-translations. Accessed 10 Jul 2023.
19. Ownby KK. Use of the Distress Thermometer in clinical
practice. J Adv Pract Oncol 2019;10:175-9. Crossref
20. Wood DE. National Comprehensive Cancer Network
(NCCN) clinical practice guidelines for lung cancer
screening. Thorac Surg Clin 2015;25:185-97. Crossref
21. Thapa S, Sun H, Pokhrel G, Wang B, Dahal S, Yu S.
Performance of Distress Thermometer and associated
factors of psychological distress among Chinese cancer
patients. J Oncol 2020;2020:3293589. Crossref
22. Au A, Lam W, Tsang J, et al. Supportive care needs in Hong
Kong Chinese women confronting advanced breast cancer.
Psychooncology 2013;22:1144-51. Crossref
23. Chi X, Chen S, Chen Y, et al. Psychometric evaluation of
the Fear of COVID-19 Scale among Chinese population.
Int J Ment Health Addict 2022;20:1273-88. Crossref
24. Vanni G, Materazzo M, Santori F, et al. The effect of
coronavirus (COVID-19) on breast cancer teamwork: a
multicentric survey. In Vivo 2020;34(3 Suppl):1685-94. Crossref
25. Pang L, Yao S, Li W, Jing Y, Yin X, Cheng H. Impact of the
CALM intervention on breast cancer patients during the
COVID-19 pandemic. Support Care Cancer 2023;31:121. Crossref
26. Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power
analyses using G*Power 3.1: tests for correlation and
regression analyses. Behav Res Methods 2009;41:1149-60. Crossref
27. Yavuz AD, Dolanbay M, Akyüz Çim EF, Dişli Gürler A,
Cündübey CF. Analysis of distress in patients with
gynecological cancers during the COVID-19 pandemic: a
telephone survey. J Clin Obstet Gynecol 2022;32:93-9. Crossref
28. Onesti CE, Vari S, Minghelli D, et al. Quality of life and
emotional distress in sarcoma patients diagnosed during
COVID-19 pandemic: a supplementary analysis from the
SarCorD study. Front Psychol 2023;14:1078992. Crossref
29. Massicotte V, Ivers H, Savard J. COVID-19 pandemic
stressors and psychological symptoms in breast cancer
patients. Curr Oncol 2021;28:294-300. Crossref
30. Myers C, Bennett K, Kelly C, et al. Impact of COVID-19 on
health care and quality of life in women with breast cancer.
JNCI Cancer Spectr 2023;7:pkad033. Crossref
31. Erdoğan Yüce G, Döner A, Muz G. Psychological distress
and its association with unmet needs and symptom burden
in outpatient cancer patients: a cross-sectional study.
Semin Oncol Nurs 2021;37:151214. Crossref
32. Al-Omari A, Al-Rawashdeh N, Damsees R, et al.
Supportive care needs assessment for cancer survivors at a
comprehensive cancer center in the Middle East: mending
the gap. Cancers (Basel) 2022;14:1002. Crossref
33. Caston NE, Lawhon VM, Smith KL, et al. Examining
the association among fear of COVID-19, psychological
distress, and delays in cancer care. Cancer Med 2021;10:8854-65. Crossref
34. Chair SY, Chien WT, Liu T, et al. Psychological distress, fear
and coping strategies among Hong Kong people during the
COVID-19 pandemic. Curr Psychol 2023;42:2538-57. Crossref
35. Matus K, Sharif N, Li A, Cai Z, Lee WH, Song M. From
SARS to COVID-19: the role of experience and experts
in Hong Kong’s initial policy response to an emerging
pandemic. Humanit Soc Sci Commun 2023;10:9. Crossref
36. Leung HT, Gong W, Sit SM, et al. COVID-19 pandemic
fatigue and its sociodemographic and psycho-behavioral
correlates: a population-based cross-sectional study in
Hong Kong. Sci Rep 2022;12:16114. Crossref
37. Liu R, Huang YC, Sun J. The media-mediated model of
information seeking behavior: a proposed framework in
the Chinese culture during the COVID-19 pandemic. Health Commun 2024;39:3468-79. Crossref
38. Yeung NC, Tang JL, Hui KH, Lau ST, Cheung AW,
Wong EL. “The light after the storm”: psychosocial
correlates of adversarial growth among nurses in Hong
Kong amid the fifth wave of the COVID-19 pandemic.
Psychol Trauma 2024;16:989-98. Crossref
39. Thompson CA, Overholser LS, Hébert JR, Risendal BC,
Morrato EH, Wheeler SB. Addressing cancer survivorship
care under COVID-19: perspectives from the cancer
prevention and control research network. Am J Prev Med
2021;60:732-6. Crossref
40. Ebrahimabadi M, Rafiei F, Nejat N. Can tele-nursing
affect the supportive care needs of patients with cancer
undergoing chemotherapy? A randomized controlled trial
follow-up study. Support Care Cancer 2021;29:5865-72. Crossref