Hong Kong Med J 2022 Aug;28(4):315–20 | Epub 10 Mar 2021
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
MEDICAL PRACTICE CME
Airway management in children with COVID-19
Karen KY Leung, MB, BS, MRCPCH1; SW Ku, MB, BS, MRCP1; Ronald CM Fung, MB, ChB, MRCPCH1; WF Hui, MB, ChB, MRCPCH1; CC Au, MB, BS, MRCPCH1; WL Cheung, MB, BS, MRCPCH1; WH Szeto, BNurs, MNurs1; Jeff CP Wong, MB, BS, MRCPCH1; KF Kwan, MB, BS, MRCP (Irel)2; KL Hon, MB, BS, MD1
1 Paediatric Intensive Care Unit, Department of Paediatrics and Adolescent Medicine, The Hong Kong Children’s Hospital, Hong Kong
2 Department of Paediatrics and Adolescent Medicine, The Hong Kong Children’s Hospital, Hong Kong
Corresponding author: Dr KL Hon (ehon@hotmail.com)
Abstract
The novel coronavirus disease (COVID-19) may
result in acute respiratory distress syndrome
and respiratory failure, necessitating mechanical
respiratory support. Healthcare professionals are
exposed to a particularly high risk of contracting the
virus while providing resuscitation and respiratory
support, which may in turn result in grave
consequences and even death. Although COVID-19
has been shown to cause milder disease in children,
paediatricians and intensivists who provide care
for children must be prepared to provide optimal
respiratory support without putting themselves
or other medical, nursing, and paramedical staff
at undue risk. We propose an airway management
approach that is especially relevant in the current
COVID-19 pandemic and provides instructions for:
(1) Elective intubation for respiratory failure; and
(2) Emergency intubation during cardiopulmonary
resuscitation. To minimise risk, intubation methods
must be kept as straightforward as possible and
should include the provision of appropriate personal
protection and equipment to healthcare workers.
We identify two key considerations: that bag-mask
ventilation should be avoided if possible and that
bacterial and viral filters should be placed in the respiratory circuit. Our novel approach provides
a framework for airway management that could
benefit paediatric critical care practitioners who
provide care for any children with a novel viral
illness, with a focus on infection prevention during
high-risk airway management procedures.
Introduction
In late 2019, a novel coronavirus named severe acute
respiratory syndrome coronavirus 2 (SARS-CoV-2)
spread to become a global pandemic, which is now
termed coronavirus disease 2019 (COVID-19).1 2 3 4 5
At the time of writing, more than 12 million people
worldwide have been infected, with a crude mortality
ratio of approximately 5%.6
In both of the erstwhile SARS and MERS
epidemics, there were reported cases of transmission
to healthcare workers.7 8 Many physicians and allied
health staff have contracted SARS-CoV, some of
whom have died of the infection. Endotracheal
intubation is considered as one of the highest risk
procedures in the context of disease transmission.9 10
During the SARS outbreak, 21% of cases worldwide
were among healthcare workers.7 Caputo et al11
estimated that 9% of the interviewed healthcare
workers who performed an intubation ended up
contracting SARS. Intubation is a high-risk aerosol-generating
procedure, and the odds ratio to contract
SARS for healthcare workers performing tracheal
intubation is 6.6 compared with those who did not perform this procedure.12
In the setting of COVID-19, SARS-CoV-2
is a highly contagious, novel virus with many
still-unknown characteristics. Recent literature
on healthcare-related transmission of COVID-19 revealed that up to 20% of infections among
healthcare workers were in those caring for
patients with COVID-19, and that hospital-related
transmission was suspected in 41% of patients.13 14
Amidst the COVID-19 pandemic, it is essential for
paediatricians and intensivists to be equipped with
clear intubation guidelines.15 16
Tracheal intubation of paediatric
patients with COVID-19
In January 2020, we promptly developed a novel
approach and protocol in preparation for the
management of critically ill paediatric patients with
COVID-19. Although several adult intensive care
unit guidelines exist in the public domain, there are
currently no standard or unified paediatric-specific
guidelines in the literature.17 18 19 Adult intubation
guidelines cannot be applied directly to paediatric practice, as children can present at wide age and
weight ranges. In addition, there is a difference in
physiology: children have higher rates of oxygen
consumption and smaller functional residual capacity.
Therefore, we tested different circuit configurations
for endotracheal intubation and propose variations
for the following hypothetical scenarios: (1) elective
intubation for respiratory failure; and (2) emergency
intubation during cardiopulmonary resuscitation.
Preparation for intubation: venue, personnel,
and equipment
Any paediatric patient who is suspected or
confirmed to be infected with SARS-CoV-2 should
be cared for in a single airborne infection isolation
room with negative pressure relative to the
atmosphere, and the outgoing air should be passed
through a high-efficiency particulate air (HEPA)
filter.20 All healthcare workers should wear personal
protective equipment appropriate for airborne
pathogens when caring for the patient, including
a fit-tested N95 respirator, goggles, a face shield, a
fluid-resistant non-sterile gown, and a pair of clean
non-sterile gloves. Staff should receive training and
practice donning and doffing of personal protective
equipment according to standard protocols.
Although SARS-CoV-2 is supposedly transmitted
by droplets instead of being airborne, healthcare
workers are advised to adopt airborne precautions in
face of this rapidly transmitting and novel pathogen
with uncertain viral characteristics.21 Ideally, the
most experienced healthcare professional should
perform the intubation with two other assistants. In the event that cricoid pressure is not given, it may be
possible to have one less assistant to reduce potential
exposure.
Age- and weight-appropriate airway
equipment should ideally be prepared ahead of time
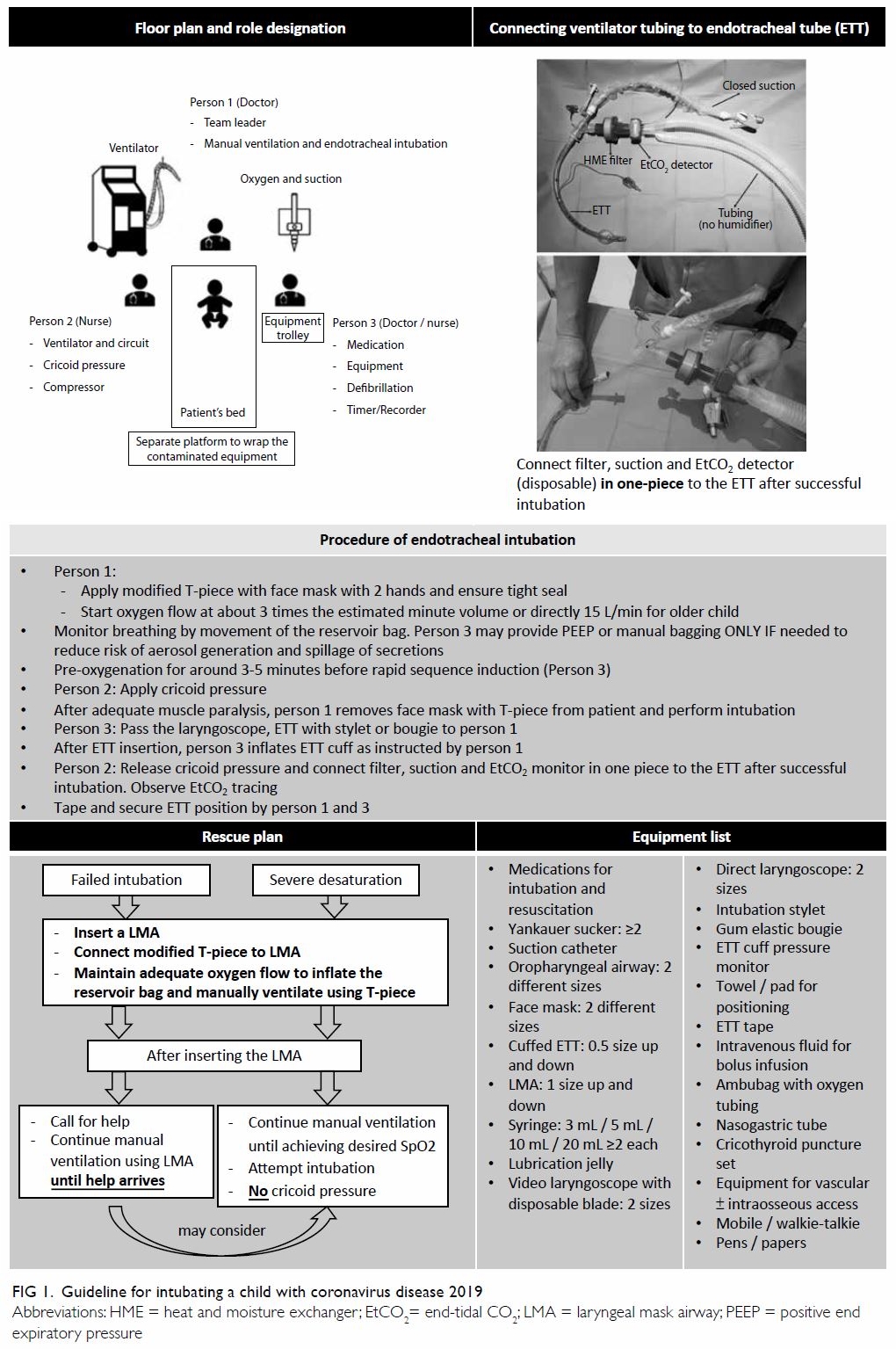
and made readily available by the bedside (Fig 1).
Single-use or dedicated equipment must be used. A
cuffed endotracheal tube (ETT) is preferable. As bag-mask
ventilation prior to intubation can generate
aerosols, the practice should be avoided as far as
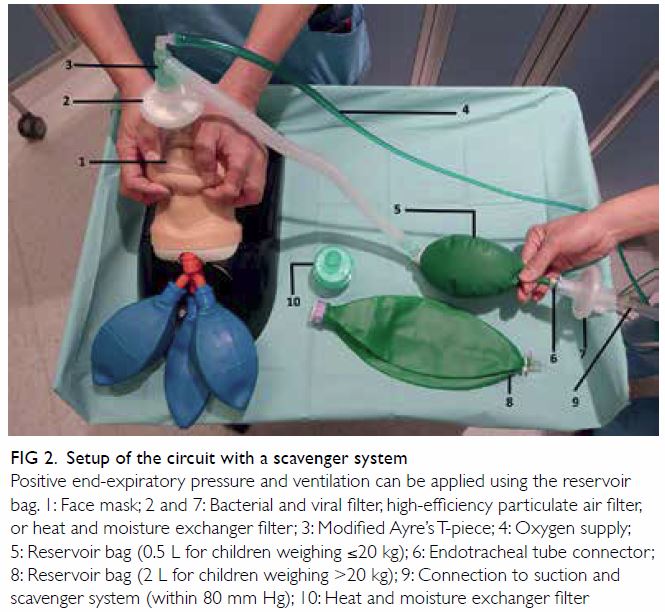
practicable.22 We suggest setting up a closed-circuit
bagging system that can be connected to a bedside scavenger to reduce the risk of viral transmission
by employing unidirectional gas flow directed
away from the patient’s side (Fig 2). A similar
scavenger system has been used in ventilator and
neonatal resuscitation circuits for suspected cases
of SARS and COVID-19.23 24 This circuit can also be
configured with a modified Ayre’s T-piece and either
a 0.5-L bag for children weighing ≤20 kg or a 2-L bag
for children weighing >20 kg. Furthermore, a
bacterial and viral filter (preferably a HEPA filter)
should be added to the system to reduce the risk of
spreading the airborne pathogens to the breathing
system and the ambient air.25 However, the choices
for HEPA filters for paediatric patients are limited,
as most HEPA filters on the market are designed
for adult patients (ie, they require a tidal volume
of at least 200-300 mL). A filter should always be
placed between the face mask and the connecting
tube of the T-piece circuit to filter all expired gas,
and we further recommend placing an additional
filter between the reservoir breathing bag and
the suction tube to filter all scavenging gas, which
would increase the filtration efficacy and reduce
the risk of viral transmission to the ambient air. The
manufacturers’ published filter specifications could
be different from the actual filtration performance,
as filtration efficiency can depend on temperature
and humidity.26 27 Theoretically, based on the size of
SARS-CoV-2 (0.06-0.2 μm), it can be removed by
HEPA filters. However, manufacturers and suppliers
might not have validated these filters for removal of
the SARS-CoV-2 virus; therefore, we suggest that
extra precautions are necessary.27 28 29 Oral suction
during intubation is unavoidably an open suction
procedure, and it is also regarded as an aerosol-generating
procedure. Thus, it should be performed
only after the administration of adequate muscle
relaxant and only when there is genuine need (eg,
when secretions obscure the larynx).
If available, video laryngoscopy should be
used to increase the chance of successful intubation
on the first pass, with the screen ideally located
at the operator’s eye level. Another advantage of
video laryngoscopy is that a longer distance can
be maintained between the intubation field and
the operator, reducing the risk of transmission. A ventilator circuit with heat and moisture
exchanger filter (HMEF), closed suction system,
and mainstream end-tidal CO2 monitor (preferably
disposable airway adaptor) should be prepared
and connected to the ETT in one piece, which
minimises any further disconnection of the circuit
after successful intubation (Fig 1). We recommend
the use of HMEF for paediatric patients as water
bath humidifiers may increase the risk of infection
dissemination. Although there might be increased
risk of sputum retention with the use of HMEF,
especially in small children, close monitoring and
regular close suction can reduce this risk. Previous
studies showed that water bath humidifiers can
produce aerosols containing bacteria, and they could
also potentially carry SARS-CoV-2.30 31
Scenario 1: Elective intubation for
respiratory failure
Patients should be pre-oxygenated by spontaneous
breathing using the modified Ayre’s T-piece system
with a tight-fitting face mask using the two-hand
technique of bag-mask ventilation. Oxygen flow
should be started at about 3 times the estimated
minute volume, and the flow of oxygen and suction
should be adjusted to keep the reservoir bag partially
inflated. The operator’s attention should be directed
to the reservoir bag’s inflation, as this provides an
indication of whether a tight seal, adequate positive
end expiratory pressure (PEEP), and an intact circuit are maintained. Manual bagging should
be avoided as much as possible. Rapid sequence
induction should be used to optimise the chance
of success on the first attempt and to minimise any
coughing or gag reflex during intubation.22 After
5 minutes of pre-oxygenation, apart from other
sedatives for rapid sequence induction, an adequate
muscle relaxant (eg, rocuronium 1.2 mg/kg) can be
administered to the patient.32 Cricoid pressure can
then be applied. After adequate muscle paralysis, the
patient can be intubated with a cuffed ETT. Once the
ETT has been passed though the cords to the proper
depth, the cuff should be immediately inflated. After
successful intubation and cuff inflation, the clinician
must ensure that there is no leakage around the cuff.
Finally, the ETT can be connected to the prepared
ventilator, and ventilation should be started
immediately to avoid bagging as far as possible.
If the intubation attempt is not successful, or if
severe desaturation persists despite pre-oxygenation
without bagging, a laryngeal mask airway can be
inserted. Manual ventilation should be continued
using the laryngeal mask airway and the modified
T-piece system with adequate oxygen flow until
help arrives. For subsequent intubation attempts,
clinicians can consider using the ETT stylet or
Bougie techniques.
Scenario 2: Emergency intubation during
cardiopulmonary resuscitation
Generally, the patient should be intubated as soon
as possible because bagging with a face mask risks
generating aerosols.10 Other than using the two-hand
technique for tight mask fitting, leaking can
also be minimised by using laryngeal mask airway
during cardiopulmonary resuscitation, particularly
if a difficult airway is anticipated or if an experienced
operator is not available.
After successful intubation, clinicians
should inflate the cuff and connect the ETT to the
ventilator immediately while adjusting the ventilator
settings in accordance with the patient’s age and
weight. It is also important to make sure that end-tidal
CO2 monitoring is available, as it is crucial to
ensure correct placement of ETT and the return of
spontaneous circulation.
Discussion
All of the equipment mentioned in this proposed
intubation approach should be commercially
available in most hospitals worldwide that provide
paediatric services. Our proposed system provides
multiple key functions, including respiratory pattern
monitoring, spontaneous respiration oxygenation,
apnoeic oxygenation, manual ventilation, and
scavenging.
Our approach has several advantages. It is a closed breathing system, provided that the face
mask has a tight seal and clinicians use the two-hand
technique, which can minimise the risk of
contaminated secretions leaking out. It allows
contaminated gases to flow in the direction of the
scavenging system, and manual ventilation is possible
by squeezing the reservoir bag if necessary. Positive
end expiratory pressure can be maintained by
partially occluding the tail of the reservoir bag. This
is especially important in the paediatric population,
as children have a low functional residual capacity,
and the addition of PEEP during pre-oxygenation can
potentially minimise or prevent functional residual
capacity reduction, airway closure, and subsequent
atelectasis. The patient’s breathing pattern can be
monitored by the movement of the reservoir bag.
Finally, a manometer can be connected to the circuit
if the operator prefers to monitor pressure in the
circuit.33
Users should be aware of some potential
limitations of our approach. First, the use of an
Ayre’s T-piece with Jackson-Rees modification
requires training. Second, adequate pre-oxygenation
is required, as there is no oxygen supply during the
period between removing the face mask from the
patient and successful endotracheal intubation.
Third, CO2 rebreathing may occur if the patient’s
minute volume is high. This can be mitigated by
using a T-piece with fresh gas flow configured to 2 to
3 times the minute volume. For example, if the fresh
oxygen flow is 15 L/min, CO2 rebreathing may occur
if the patient’s minute volume is more than 5 to
7.5 L/min; Fourth, the system cannot be used in
areas with no oxygen supply. Finally, the whole
system might be under negative pressure during the
entire expiratory phase, which may lead to alveolar
collapse. The application of a low level of PEEP to the
anaesthetic bag would prevent this from occurring.
Further, clinical and radiological evaluations are
indicated to ensure that there is no significant
atelectasis.
With adequate training and practice, our
proposed approach to intubation should be safe and
effective. We would welcome further research in a
laboratory setting to test the system’s integrity and
quantitatively measure the reductions in aerosols
that it generates.
Conclusion
Amidst the current pandemic, in which much
remains unknown about the coronavirus and
COVID-19 disease, healthcare workers should take
the highest levels of precautions and protection
when providing care to patients with suspected
SARS-CoV-2 infection and respiratory failure.
By sharing the approach we have developed for
endotracheal intubation, we aim to raise awareness of the precautions that need to be taken during
intubation to reduce the risk of healthcare-related
transmission, not only in the current COVID-19
pandemic, but also in future outbreaks of airborne
pathogens.34 A review of all published paediatric
airway and intubation protocols is now underway
to evaluate this important management facet in
paediatrics. Paediatricians should be as well prepared
as physicians who care for adults.
Author contributions
All authors contributed to the concept or design of the study,
acquisition of the data, analysis or interpretation of the
data, drafting of the manuscript, and critical revision of the
manuscript for important intellectual content. All authors
had full access to the data, contributed to the study, approved
the final version for publication, and take responsibility for its
accuracy and integrity.
Conflicts of interest
As an editor of the journal, KL Hon was not involved in
the peer review process. Other authors have no conflicts of
interest to disclose.
Funding/support
This research received no specific grant from any funding
agency in the public, commercial, or not-for-profit sectors.
References
1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from
patients with pneumonia in China, 2019. N Engl J Med
2020;382:727-33. Crossref
2. Huang C, Wang Y, Li X, et al. Clinical features of patients
infected with 2019 novel coronavirus in Wuhan, China.
Lancet 2020;395:497-506. Crossref
3. Hon KL, Leung KK. Severe acute respiratory symptoms
and suspected SARS again 2020. Hong Kong Med J
2020;26:78-9. Crossref
4. World Health Organization. Naming the coronavirus
disease (COVID-19) and the virus that causes it. Available
from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it. Accessed 24 Feb 2020.
5. Hon KL, Leung KK, Leung AK, et al. Overview: the history
and pediatric perspectives of severe acute respiratory
syndromes: novel or just like SARS. Pediatr Pulmonol
2020;55:1584-91. Crossref
6. Coronavirus Resource Center, Johns Hopkins University.
COVID-19 dashboard by the Center for Systems Science
and Engineering at Johns Hopkins University. 2020.
Available from: https://coronavirus.jhu.edu/map.html. Accessed 10 Jul 2020.
7. World Health Organization. Summary of probable SARS
cases with onset of illness from 1 November 2002 to 31
July 2003. Available from: https://www.who.int/csr/sars/country/table2004_04_21/en/. Accessed 4 Jan 2020.
8. Al-Tawfiq JA, Auwaerter PG. Healthcare-associated
infections: the hallmark of Middle East respiratory
syndrome coronavirus with review of the literature. J Hosp
Infect 2019;101:20-9. Crossref
9. Fowler RA, Guest CB, Lapinsky SE, et al. Transmission
of severe acute respiratory syndrome during intubation
and mechanical ventilation. Am J Respir Crit Care Med
2004;169:1198-202. Crossref
10. Chan MT, Chow BK, Lo T, et al. Exhaled air dispersion
during bag-mask ventilation and sputum suctioning—implications for infection control. Sci Rep 2018;8:198. Crossref
11. Caputo KM, Byrick R, Chapman MG, Orser BA, Orser BJ.
Intubation of SARS patients: infection and perspectives of
healthcare workers. Can J Anesth 2006;53:122-9. Crossref
12. Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J.
Aerosol generating procedures and risk of transmission
of acute respiratory infections to healthcare workers: a
systematic review. PLoS One 2012;7:e35797. Crossref
13. Remuzzi A, Remuzzi G. COVID-19 and Italy: what next?
Lancet 2020;395:1225-8. Crossref
14. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138
hospitalized patients with 2019 novel coronavirus-infected
pneumonia in Wuhan, China. JAMA 2020;323:1061-9. Crossref
15. Li Q, Guan X, Wu P, et al. Early transmission dynamics in
Wuhan, China, of novel coronavirus-infected pneumonia.
N Engl J Med 2020;382:119-207. Crossref
16. Wu JT, Leung K, Leung GM. Nowcasting and forecasting
the potential domestic and international spread of the
2019-nCoV outbreak originating in Wuhan, China: a
modelling study. Lancet 2020;395:689-97. Crossref
17. Cheung JC, Ho LT, Cheng JV, Cham EY, Lam KN. Staff
safety during emergency airway management for COVID-19 in Hong Kong. Lancet Respir Med 2020;8:e19. Crossref
18. Yao W, Wang T, Jiang B, et al. Emergency tracheal intubation
in 202 patients with COVID-19 in Wuhan, China: lessons
learnt and international expert recommendations. Br J
Anaesth 2020;125:e28-37.
19. Brewster DJ, Chrimes N, Do TB, et al. Consensus statement:
Safe Airway Society principles of airway management and
tracheal intubation specific to the COVID-19 adult patient
group. Med J Aust 2020;212:472-81. Crossref
20. American Society of Anesthesiologists. COVID-19
Information for health care professionals. 2020. Available from: https://www.asahq.org/about-asa/governance-and-committees/asa-committees/committee-on-occupational-health/coronavirus. Accessed 6 Feb 2020.
21. World Health Organization. Infection prevention and
control during health care when novel coronavirus (nCoV)
infection is suspected. Interim guidance. Available from:
https://www.who.int/publications/i/item/10665-331495.
Accessed 9 Feb 2020. Crossref
22. Wax RS, Christian MD. Practical recommendations
for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth
2020;67:568-76. Crossref
23. Ng PC, So KW, Leung TF, et al. Infection control for SARS
in a tertiary neonatal centre. Arch Dis Child Fetal Neonatal
Ed 2003;88:F405-9. Crossref
24. Trevisanuto D, Moschino L, Doglioni N, Roehr CC,
Gervasi MT, Baraldi E. Neonatal resuscitation where the
mother has a suspected or confirmed novel coronavirus
(SARS-CoV-2) infection: suggestion for a pragmatic action
plan. Neonatology 2020;117:133-40. Crossref
25. Heuer JF, Crozier TA, Howard G, Quintel M. Can breathing
circuit filters help prevent the spread of influenza A (H1N1)
virus from intubated patients? GMS Hyg Infect Control
2013;8:Doc09.
26. Dellamonica J, Boisseau N, Goubaux B, Raucoules-Aimé
M. Comparison of manufacturers’ specifications for 44
types of heat and moisture exchanging filters. Br J Anaesth
2004;93:532-9. Crossref
27. Fisher & Paykel Healthcare. Viral & bacterial filtration
efficiency of Fisher & Paykel healthcare filters and F&P
EvaquaTM 2 circuits. 2020. Available from: https://www.
fphcare.com/us/covid-19/filters-evaqua-circuits-covid-
19/#tested-covid. Accessed 13 Jul 2020.
28. Hamilton Medical. Efficiency of HEPA filters. 2020.
Available from: https://www.hamilton-medical.com/fr_CH/E-Learning-and-Education/Knowledge-Base/Knowledge-Base-Detail~2020-03-18~Efficiency-of-HEPA-filters~d5358f88-753e-4644-91c6-5c7b862e941f~.html. Accessed 13 Jul 2020.
29. Smiths Medical. HEPA filter information. 23 Mar 2020.
Available from: https://www.smiths-medical.com/company-information/news-and-events/news/2020/march/23/hepa-filter-letter. Accessed 13 Jul 2020.
30. Gilmour IJ, Boyle MJ, Streifel A, McComb RC. The effects
of circuit and humidifier type on contamination potential
during mechanical ventilation: a laboratory study. Am J
Infect Control 1995;23:65-72. Crossref
31. Al Ashry HS, Modrykamien AM. Humidification during mechanical ventilation in the adult patient. Biomed Res Int
2014;2014:715434. Crossref
32. World Health Organization. Clinical management of
severe acute respiratory infection when novel coronavirus
(nCoV) infection is suspected: interim guidance, 28
January 2020. Available from: https://apps.who.int/iris/handle/10665/330893. Accessed 11 Feb 2020.
33. Trachsel D, Svendsen J, Erb TO, von Ungern-Sternberg BS.
Effects of anaesthesia on paediatric lung function. Br J
Anaesth 2016;117:151-63. Crossref
34. Hon KL. Just like SARS. Pediatr Pulmonol 2009;44:1048-9. Crossref