Hong Kong Med J 2025;31:Epub 30 Jun 2025
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
EDITORIAL
New IMPACT Guideline to help doctors on rational prescription of antimicrobials
Edmond SK Ma, MD, FHKAM (Community Medicine)1,2 †; Edwin LK Tsui, MMed (Public Health), FHKAM (Community Medicine)2; Tak-chiu Wu, FHKAM (Medicine)3 ‡; Pak-leung Ho, MD, FIDSA4 ‡
1 Epidemiology Adviser, Hong Kong Medical Journal
2 Centre for Health Protection, Department of Health, Hong Kong SAR, China
3 Queen Elizabeth Hospital, Hospital Authority, Hong Kong SAR, China
4 Carol Yu Centre for Infection, The University of Hong Kong, Hong Kong SAR, China
† Editorial Board Member, the 6th edition of IMPACT Guidelines
‡ Editor, the 6th edition of IMPACT Guidelines
Corresponding author: Dr Edmond SK Ma (edmond_sk_ma@dh.gov.hk), Dr Pak-leung Ho (plho@hku.hk)
The Centre for Health Protection (CHP) of the
Department of Health launched the 6th edition of
the Interhospital Multi-disciplinary Programme on
Antimicrobial ChemoTherapy (IMPACT) Guideline
at the Infectious Disease Forum on 19 June 2025,
where key updates were presented to healthcare
professionals.1 The latest edition encompasses global
and local antimicrobial resistance (AMR) trends
and provides updated guidance on antimicrobial
use, including dosing, adverse reactions, empirical
treatment of common infections, targeted therapy
for known pathogens, surgical prophylaxis, and
antibiotic allergy management. A new section
on Outpatient Parenteral Antimicrobial Therapy
highlights key considerations for this treatment
modality. The Guideline also includes a list of
calculators to facilitate the clinical management of
various infections such as streptococcal pharyngitis,
pneumonia, acute pancreatitis, sepsis, and pleural
effusions (Light’s criteria). In addition, healthcare
workers can access the antibiograms from both
public and private hospitals to check resistance
patterns of common bacterial isolates including
Escherichia coli, Klebsiella species, Staphylococcus
aureus, Pseudomonas aeruginosa, Haemophilus
influenzae, Enterococcus species, and Acinetobacter
species. These updates address evolving AMR
patterns with the latest clinical evidence to ensure
the judicious use of antimicrobials.
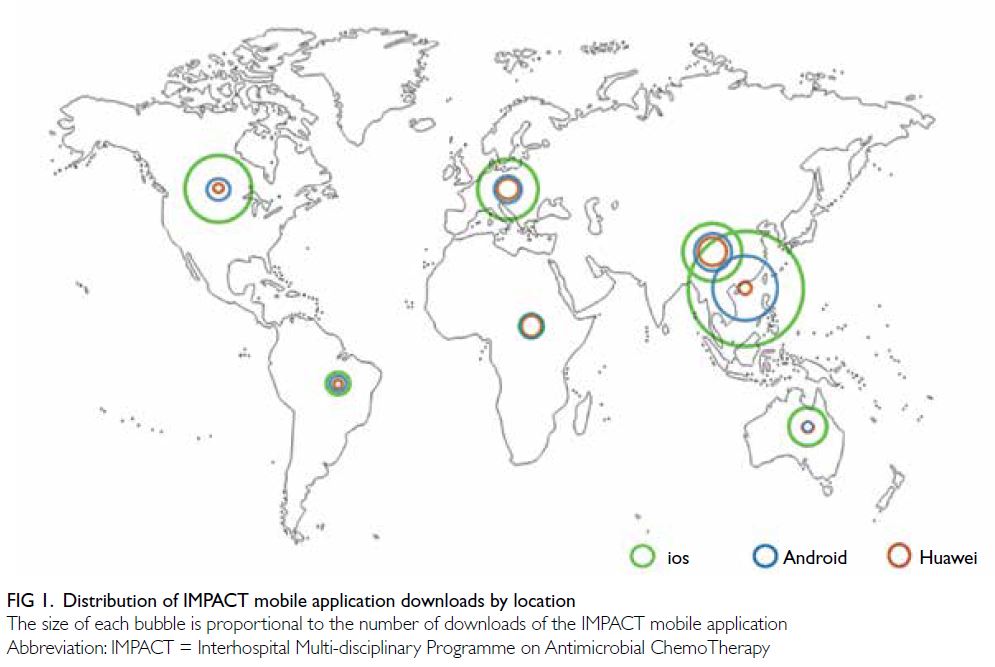
Since its inaugural edition in 1999, the IMPACT
Guideline has served as a vital resource for managing
infections in hospitalised patients. The development
of an e-book and mobile app has improved
accessibility. Since its release in 2013, the mobile app
has been downloaded over 52 000 times, including
by users overseas (Fig 1). In this edition, Editors and
Associate Editors, including clinical microbiologists
and infectious disease specialists, have revised the
content based on international guidelines, up-to-date
scientific research, local epidemiology, and surveillance data. The IMPACT Guideline is a
collaborative effort involving the CHP of the Department of Health,
Li Ka Shing Faculty of Medicine and the Carol Yu
Centre for Infection of The University of Hong Kong,
Faculty of Medicine at The Chinese University of
Hong Kong, the Hong Kong Medical Association,
and the Hong Kong Private Hospitals Association. It
serves as a critical tool for optimising antimicrobial
use across both public and private healthcare sectors
and is a key component of the Government’s Hong
Kong Strategy and Action Plan on Antimicrobial
Resistance 2023-2027.2
The Guideline has become one of the
cornerstones in implementing antimicrobial
stewardship programmes in public hospitals and
could serve as a key reference for enhancing similar
programmes in private hospitals. The CHP has
been tracking antimicrobial supply as a proxy for
consumption through surveillance data collected
from licensed wholesale traders. A significant
reduction in the overall defined DID (daily dose
per 1000 inhabitants per day) was observed during
the three pandemic years (2020-2022), with a
reduction of 27.2% compared to the pre-COVID
baseline, probably due to a decrease in respiratory
infections.3 However, a rebound in DID was noted
beginning in 2023, particularly in the private sector
following the resumption of normalcy.1 The CHP has
also been monitoring antimicrobial consumption
according to the World Health Organization
(WHO)’s AWaRe categorisation, namely Access,
Watch and Reserve.4 This categorisation, based on
resistance risk and medical importance, aims to
improve appropriate antibiotic use. According to
the WHO, “Access” antibiotics can be used freely,
“Watch” antibiotics require caution, and “Reserve”
antibiotics are considered for last-resort cases. The
WHO advocates for “Access” antibiotics to comprise
at least 60% of total antibiotics consumed, reserving “Watch” and “Reserve” antibiotics for specific,
indicated conditions. In Hong Kong, the proportion
of antimicrobial use in the “Access” group has
met the WHO target of 60% since 2020 (Fig 2).
Furthermore, the “Watch” group (lower resistance
potential) decreased from 40.3% in 2016 to 34.6%
in 2024, indicating relatively fewer prescriptions of
broad-spectrum antibiotics.
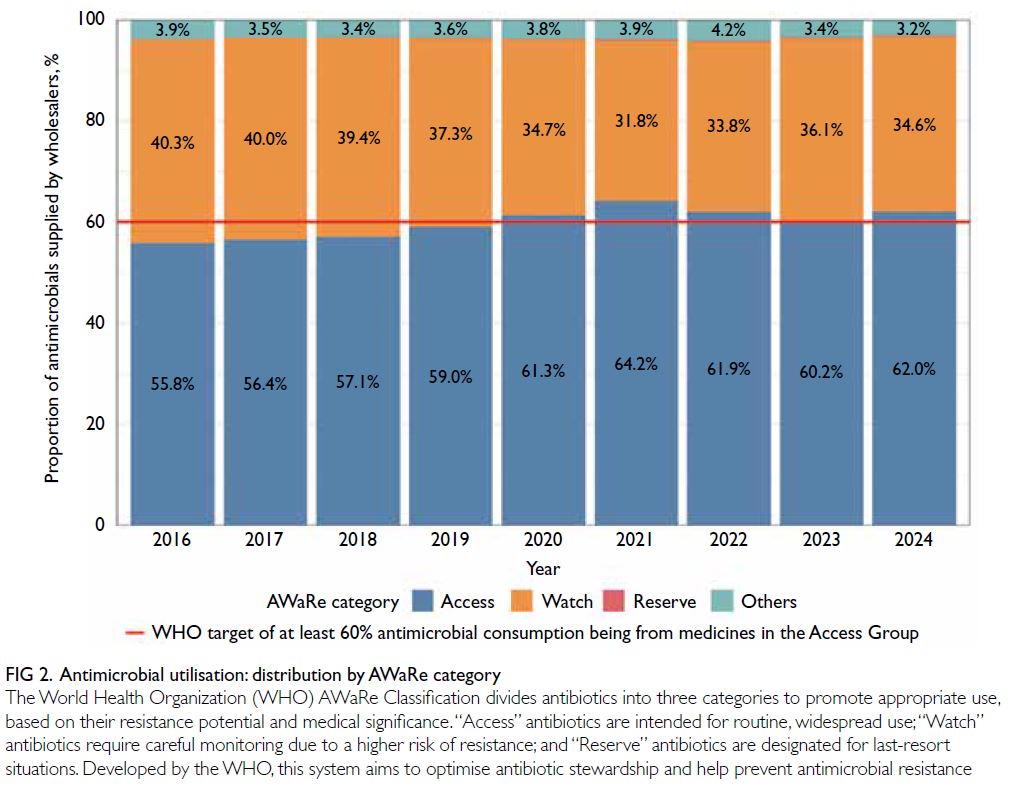
Figure 2. Antimicrobial utilisation: distribution by the World Health Organization (WHO)’s AWaRe categorisation
Nevertheless, we should not become
complacent about the problem of AMR. A recent
global study estimated that 4.71 million deaths
were associated with bacterial AMR, including
1.14 million deaths directly attributable to it.5 The
same study forecasts that an estimated 1.91 million
deaths attributable to AMR and 8.22 million deaths
associated with AMR could occur globally by
2050. These projections do not yet account for the
possible delayed negative impact of the COVID-19
pandemic on AMR.6 The WHO has reported that
approximately 75% of COVID-19 patients received
antibiotics, despite only 8% having bacterial co-infections,
based on data from 450 000 patients
across 65 countries from January 2020 to March
2023.7 Locally, it has been estimated that AMR-related
infections in Hong Kong between 2020
and 2030 could result in 18 433 excess deaths and
incur an economic cost of US$4.3 billion.8 The
CHP surveillance data suggest an upward trend in
various multidrug resistant pathogens, including
carbapenem-resistant Escherichia coli, vancomycin-resistant Enterococcus, and Candida auris, which
have further strained our hospitals.9 10 The local threat of AMR is severe, underscoring the need for robust
antibiotic stewardship. While it takes approximately
10 to 15 years to develop a new antibiotic, resistance
can emerge in much shorter timeframes. At the
79th United Nations General Assembly High-Level
Meeting on AMR held in September 2024, global
leaders approved a political declaration committing
to a clear set of targets and actions, including
reducing the estimated 4.95 million annual deaths
associated with bacterial AMR by 10% by 2030.11 The
declaration also aims for at least 70% of antibiotics
used in human health globally to belong to the
WHO “Access” group, emphasising the critical need
for coordinated efforts to preserve our ability to
treat infections and sustain the healthcare system.
We urge all doctors, both in the public and private
sectors, to prescribe antibiotics only when clinically
indicated and to choose appropriate agents based on
established clinical guidelines, such as the IMPACT
Guideline.
Author contributions
All authors contributed to the editorial, approved the final
version for publication, and take responsibility for its accuracy
and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This editorial received no specific grant from any funding
agency in the public, commercial, or not-for-profit sectors.
References
1. Centre for Health Protection, Department of Health,
Hong Kong SAR Government. CHP updates antimicrobial
guidelines and urges doctors to prescribe antimicrobials
appropriately. 19 Jun 2025. Available from: https://www.info.gov.hk/gia/general/202506/19/P2025061900342.htm. Accessed 20 Jun 2025.
2. Ma ES. Combating antimicrobial resistance in Hong Kong:
where are we and where should we go? Hong Kong Med J
2022;28:424-6. Crossref
3. Ma ES, Hsu E, Chow V, et al. Rebound of antibiotic use
and respiratory infections after resumption of normalcy
from COVID-19 in Hong Kong. Infect Drug Resist
2025;18:1325-37. Crossref
4. World Health Organization. The WHO AWaRe (Access, Watch, Reserve) antibiotic book. Geneva, Switzerland: World Health Organization; 2022.
5. GBD 2021 Antimicrobial Resistance Collaborators.
Global burden of bacterial antimicrobial resistance 1990-2021: a systematic analysis with forecasts to 2050. Lancet
2024;404:1199-226. Crossref
6. Ma ES, Wong SC, Cheng VC, Wu P. Global trends
and projections in antimicrobial resistance. Lancet 2025;405:1904-5. Crossref
7. World Health Organization. WHO reports widespread
overuse of antibiotics in patients hospitalized with
COVID-19. 26 April 2024. Available from: https://www.who.int/news/item/26-04-2024-who-reports-widespread-overuse-of-antibiotics-in-patients--hospitalized-with-covid-19. Accessed 13 Jun 2025.
8. World Health Organization. Health and economic impacts
of antimicrobial resistance in the Western Pacific Region,
2020-2030. 13 June 2023. Available from: https://www.who.int/publications/i/item/9789290620112. Accessed 13 Jun 2025.
9. Centre for Health Protection, Department of Health,
Hong Kong SAR Government. Statistics on antimicrobial
resistance control. Available from: https://www.chp.gov.hk/en/static/101600.html. Accessed 13 Jun 2025.
10. Ma ES, Kung KH, Chen H. Combating antimicrobial resistance during the COVID-19 pandemic. Hong Kong Med J 2021;27:396-8. Crossref
11. World Health Organization. World leaders commit to
decisive action on antimicrobial resistance. 26 September
2024. Available from: https://www.who.int/news/item/26-09-2024-world-leaders-commit-to-decisive-action-on-antimicrobial-resistance. Accessed 13 Jun 2025.