Hong Kong Med J 2026;32:Epub 27 Jan 2026
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Caecal bascule as an ultra-rare cause of intestinal obstruction: a case report
HW Ip, MB, ChB, FCSHK1; WH Hui, MB, ChB, FHKCR2
1 Department of Surgery, North District Hospital, Hong Kong SAR, China
2 Department of Radiology, Prince of Wales Hospital, Hong Kong SAR, China
Corresponding author: Dr HW Ip (ihw642@ha.org.hk)
Case presentation
A 60-year-old man was admitted as an emergency
to North District Hospital in March 2024 with a
1-day history of progressive abdominal distension.
He also reported colicky central abdominal pain
without radiation, vomiting of clear fluid, and no
bowel movements for 2 days. He was a chronic
smoker and social drinker but past medical history
was unremarkable, except for bilateral renal stones
treated with extracorporeal shock wave lithotripsy in
1998 and 2003.
His vital signs on admission were temperature
36.6°C, heart rate 104 bpm, blood pressure 157/99 mm
Hg, and respiratory rate of 16. Physical examination
revealed a mildly distended abdomen without
peritoneal signs. Laboratory tests were abnormal
with a white blood cell count of 21.0×103/μL and
lactate of 4.9 mmol/L. Abdominal X-ray showed
prominent bowel loops in the central abdomen.
Computed tomography revealed a distended
gallbladder, oedematous gallbladder wall thickening
and pericholecystic inflammatory fat stranding
without gallstones; the caecum and a segment of
terminal ileum were prominently dilated, measuring
up to 8.4 cm and 2.8 cm, respectively, with a gradual
transition zone identified between the caecum and ascending colon (Fig 1). Initial radiology suggested
acute cholecystitis and faecal impaction. However,
after further clarification and in the absence of any
mesenteric rotation or twisting, a diagnosis of caecal
volvulus (bascule type) could not be made.
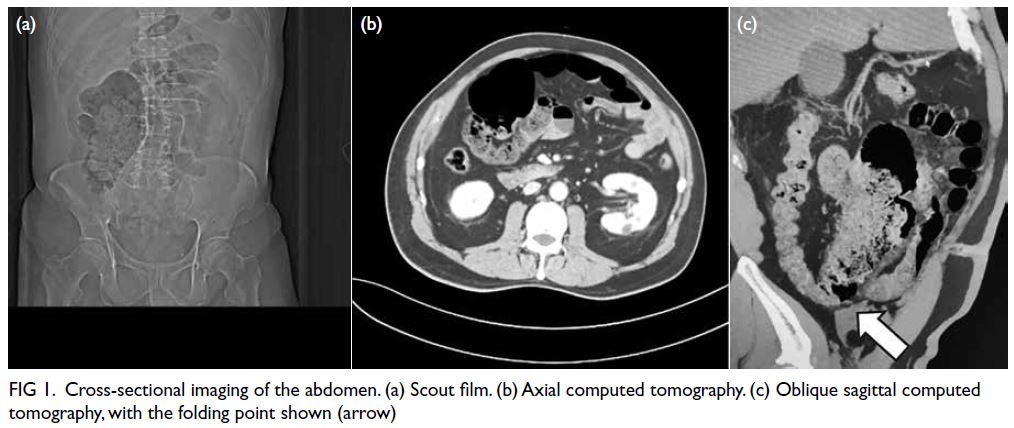
Figure 1. Cross-sectional imaging of the abdomen. (a) Scout film. (b) Axial computed tomography. (c) Oblique sagittal computed tomography, with the folding point shown (arrow)
Antibiotics were started immediately.
Emergency surgery for cholecystectomy and
evaluation of the caecum was offered. Laparoscopy
revealed a grossly distended caecum with congestion
of part of the caecal wall, which appeared to
fold anteromedially, creating a closed-loop
obstruction (Fig 2). The gallbladder was inflamed.
Laparoscopy proceeded to open surgery, and a right
hemicolectomy with primary ileo-colic anastomosis
and cholecystectomy were performed. A 3-cm
gallstone was found inside the gallbladder.
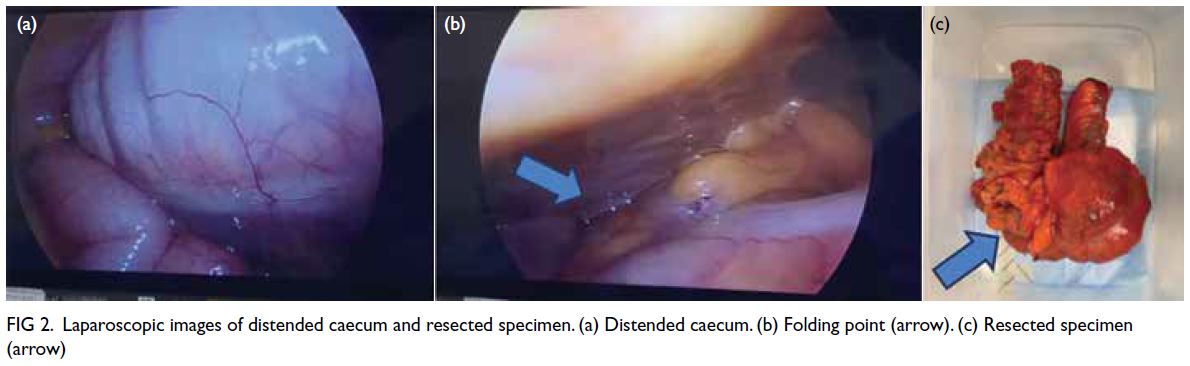
Figure 2. Laparoscopic images of distended caecum and resected specimen. (a) Distended caecum. (b) Folding point (arrow). (c) Resected specimen (arrow)
Pathological examination of the right
hemicolectomy specimen revealed marked thinning
of the intestinal wall (1 mm thick) with features
consistent with volvulus. The overlying mucosa
appeared dusky. Microscopically, there were
features of early-stage ischaemia with sloughing of
the overlying epithelium, submucosal oedema, and
purulent fibrinous exudate over the serosal surface.
Gallbladder pathology confirmed acute gangrenous
cholecystitis.
Discussion
Caecal volvulus accounts for 1% of intestinal
obstruction cases, with an incidence of 2.8 to 7.1
per million people per year.1 It is classified according
to geometry: the caecal bascule is the rarest form,
designated as type III caecal volvulus, accounting
for 20% of all caecal volvuli.1 A systematic review
in 2018 reported only 26 cases in the literature,
with a median age of 55 years and a male-to-female
ratio of 14:12.2 It involves anterior-superior folding
of the caecum without axial twisting, leading to
obstruction of the ascending colon.1 If the ileocaecal
valve is competent, bowel dilatation is confined to
the caecum, forming a closed-loop obstruction. In
the absence of torsion, diagnosis via cross-sectional
imaging is more challenging. Delayed diagnosis and
treatment may result in bowel ischaemia, gangrene,
and perforation.
The caecum is normally a secondary
retroperitoneal and immobile structure. However,
it can become mobile due to congenital or acquired
factors, predisposing it to volvulus. Common risk
factors include previous abdominal surgery, high
fibre intake, chronic constipation, and distal bowel
obstruction.
Clinically, caecal volvulus presents similarly to
small bowel obstruction. Cardinal symptoms include
nausea, vomiting (30%), abdominal pain (61%), and
abdominal distension (84%).2 Caecal bascule may
manifest with milder symptoms and reduced risk of
ischaemia, as there is less mesenteric torsion and the
caecum may return to its anatomical position.
Although computed tomography is the initial
diagnostic tool of choice, with a reported sensitivity
of 61%, some cases are diagnosed only during
exploratory laparotomy.2 The classic ‘whirl sign’,
seen in types I and II caecal volvulus, is absent in
caecal bascule. Instead, the distended caecum folds
anteriorly without torsion and typically located
in the central abdomen.3 The transition zone lies
between the ascending colon and caecum.
In our patient, diagnosis of caecal bascule was
difficult, likely due to the rarity of the condition.
With hindsight, the appendiceal orifice lay medial
and superior to the terminal ileum, offering indirect
evidence of anterior-superior folding to the caecum.
A grossly distended caecum in isolation should raise
suspicion of caecal volvulus. Examining the relative
positions of the appendix and terminal ileum may
provide diagnostic clues.
Prompt surgical intervention is often
recommended due to the high risk of perforation.
Non-operative management has a success rate as
low as 3.8%, and endoscopic treatment success
is reported at up to 30%, much lower than 70% to
95% in sigmoid volvulus.3 Surgical options depend
on bowel viability and intraoperative stability. Right
hemicolectomy with primary ileo-colic anastomosis
is the treatment of choice with the lowest recurrence
risk. Alternatives such as ileocecal resection with
colopexy of the right colon remnant2 and derotation
with caecopexy or caecostomy have been reported.2 3
Acute cholecystitis is rarely associated with
caecal volvulus, with the first report in 2013.4 It
was believed that the right colon adhered to the
inflamed gallbladder formed part of an inflammatory
phlegmon, acting as a pivot for caecal rotation.
However, this phenomenon was not observed
intraoperatively in our case.
To the best of our knowledge, this is the
second reported case of caecal bascule in Hong
Kong.5 This case highlights the diagnostic challenge
for this rare condition. A high index of clinical
suspicion is needed for timely diagnosis. Greater
awareness among healthcare professionals may help
prevent serious outcomes from this potentially life-threatening
presentation.
Author contributions
Concept or design: Both authors.
Acquisition of data: Both authors.
Analysis or interpretation of data: HW Ip.
Drafting of the manuscript: Both authors.
Critical revision of the manuscript for important intellectual content: HW Ip.
Acquisition of data: Both authors.
Analysis or interpretation of data: HW Ip.
Drafting of the manuscript: Both authors.
Critical revision of the manuscript for important intellectual content: HW Ip.
Both authors had full access to the data, contributed to the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
Both authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki. Written consent was obtained from the patient for all treatments and procedures, and publication of the case
report, including the accompanying clinical images.
References
1. Delabrousse E, Sarliève P, Sailley N, Aubry S, Kastler BA.
Cecal volvulus: CT findings and correlation with
pathophysiology. Emerg Radiol 2007;14:411-5. Crossref
2. Lung BE, Yelika SB, Murthy AS, Gachabayov M, Denoya P.
Cecal bascule: a systematic review of the literature. Tech
Coloproctol 2018;22:75-80. Crossref
3. Takahashi M, Ando Y, Kochi S, et al. Three surgical cases of
cecal volvulus. Cureus. 2024;16:e72794. Crossref
4. Anjum GA, Jaberansari S, Habeeb K. Caecal volvulus:
a consequence of acute cholecystitis. BMJ Case Rep
2013;2013:bcr2013009705. Crossref
5. Kim YI, Han SK, Min MK, Park SW, Yeom SR. Improvement
of a cecal bascule by supportive care. Hong Kong J Emerg
Med 2017;25:102490791774814. Crossref

