Hong Kong Med J 2023;29:Epub 4 Dec 2025
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
MEDICAL PRACTICE
Expert consensus recommendations on the daily
clinical use of pembrolizumab for early triple-negative
breast cancer
Winnie Yeo, MD, FRCP1; Yolanda HY Chan, FRCSEd, FHKAM (Surgery)2; Roland CY Leung, MRCP, DABIM3; Sharon WW Chan, FRACS, FHKAM (Surgery)4; Lorraine CY Chow, FRCSEd, FHKAM (Surgery)5; William WL Foo, FRCR, FHKAM (Radiology)6; Sara WW Fung, FRCSEd, FHKAM (Surgery)7; Carol CH Kwok,FRCR, FHKAM (Radiology)8; Stephanie HY Lau, FRCSEd, FHKAM (Surgery)9; Alex KC Leung, FRCR, FHKAM (Radiology)10; Ting Ying Ng, FRCR, FHKAM (Radiology)11; Janice Tsang, FRCP, FHKAM (Medicine)12,13; Iris KM Wong, FRCR, FHKAM (Radiology)14; Chun Chung Yau, FRCP, FHKAM (Radiology)15; Marvin HY Yuen, FRACS, FHKAM (Surgery)16; Polly SY Cheung, FRCS, FRACS17
1 Department of Clinical Oncology, The Chinese University of Hong Kong, Hong Kong SAR, China
2 Breast Health Clinic, CUHK Medical Centre, Hong Kong SAR, China
3 Department of Medicine, Queen Mary Hospital, Hong Kong SAR, China
4 Department of Surgery, United Christian Hospital, Hong Kong SAR, China
5 Private Practice, Hong Kong SAR, China
6 Radiotherapy and Oncology Centre, Gleneagles Hospital, Hong Kong SAR, China
7 Department of Surgery, Kwong Wah Hospital, Hong Kong SAR, China
8 Department of Oncology, Princess Margaret Hospital, Hong Kong SAR, China
9 Department of Surgery, Hong Kong Baptist Hospital, Hong Kong SAR, China
10 Department of Clinical Oncology, Queen Elizabeth Hospital, Hong Kong SAR, China
11 Department of Clinical Oncology, Tuen Mun Hospital, Hong Kong SAR, China
12 Founding Convenor, Hong Kong Breast Oncology Group, Hong Kong SAR, China
13 School of Clinical Medicine, The University of Hong Kong, Hong Kong SAR, China
14 Department of Oncology, United Christian Hospital, Hong Kong SAR, China
15 Comprehensive Oncology Centre, Hong Kong Sanatorium & Hospital, Hong Kong SAR, China
16 Department of Surgery, Pok Oi Hospital, Hong Kong SAR, China
17 Breast Care Centre, Hong Kong Sanatorium & Hospital, Hong Kong SAR, China
Corresponding author: Prof Winnie Yeo (winnie@clo.cuhk.edu.hk)
Abstract
Neoadjuvant chemotherapy is a standard treatment for triple-negative breast cancer (TNBC) at an
early stage. Given that pathological complete
response is strongly associated with long-term
clinical and survival benefits, the selection of
appropriate treatment before and after surgery
could further optimise treatment outcomes. With
the emergence of immunotherapy in breast cancer,
more combination treatment options are available,
such as pembrolizumab, a programmed death
receptor 1 inhibitor, which is approved for the
perioperative treatment of stage II and III TNBC.
However, the implementation of immunotherapy
in perioperative settings for TNBC requires further
discussion regarding patient selection and the
use of different treatments in conjunction with
immunotherapy. The Hong Kong Breast Cancer
Foundation convened a multidisciplinary consensus
panel consisting of surgeons, clinical oncologists,
and medical oncologists to initiate this discussion.
A modified Delphi panel was conducted, evaluating
seven topics and 45 statements covering the workup
and perioperative treatment of early-stage TNBC
(eTNBC). The consensus statements provide
guidance on determining whether a patient with
eTNBC is a suitable candidate for neoadjuvant
chemotherapy and immunotherapy.
Introduction
Triple-negative breast cancer (TNBC), representing
10% to 15% of breast cancer cases, is characterised
by the absence of oestrogen receptors (ER),
progesterone receptors (PR), and human epidermal
growth factor receptor 2 (HER2) amplification
or overexpression. It is associated with higher
rates of recurrence, metastasis, and worse overall
survival (OS) than other subtypes.1 2 Given its high immune infiltration rate, with over 50% tumour-infiltrating
lymphocytes in histological samples,3 4
TNBC is amenable to immunomodulation through
immunotherapy.
Immunotherapies directed against
programmed death receptor 1 (PD-1) or
programmed death receptor ligand 1 (PD-L1)
have shown promising and positive results in
patients with metastatic TNBC (mTNBC), based on the phase III randomised KEYNOTE-355
and IMpassion130 trials.5 6 7 Addition of the anti–PD-1 antibody pembrolizumab to chemotherapy
significantly improved progression-free survival and
OS by 4.1 months and 6.9 months, respectively, in
patients with mTNBC whose tumours expressed
PD-L1 (combined positive score [CPS] ≥10).5 6
The effectiveness of neoadjuvant
pembrolizumab in combination with neoadjuvant
chemotherapy (NAC) was demonstrated in the
KEYNOTE-5228 9 and NeoImmunoBoost trials.10
The pathological complete response (pCR) rate
significantly increased from 51.2% among patients
receiving NAC alone to 64.8% among those receiving
pembrolizumab–chemotherapy in the former study,
independent of PD-L1 status.8 Event-free survival
(EFS) at 36 months also increased from 76.8% to
84.5%.9 Although pembrolizumab demonstrated
favourable results in the KEYNOTE-522 study,
several important questions regarding patient
selection, types and schedules of chemotherapy,
and treatment plans for patients with residual
disease after surgery remain in real-world practice.
Therefore, the Hong Kong Breast Cancer Foundation
(HKBCF) convened a multidisciplinary consensus to
guide the practical use of pembrolizumab locally.
The results of this consensus were partially
presented during the Hong Kong Breast Cancer
Symposium in November 2023 and in abstract form
at the American Society of Clinical Oncology Annual
Meeting 2024.11 Here, we present the full results.
Methods
To explore the perioperative use of immunotherapy
and provide expert guidance for routine clinical practice in the treatment of early triple-negative
breast cancer (eTNBC), the HKBCF established
a consensus panel comprising seven breast
surgeons, six clinical oncologists, and three medical
oncologists, each with at least 15 years of clinical
experience.
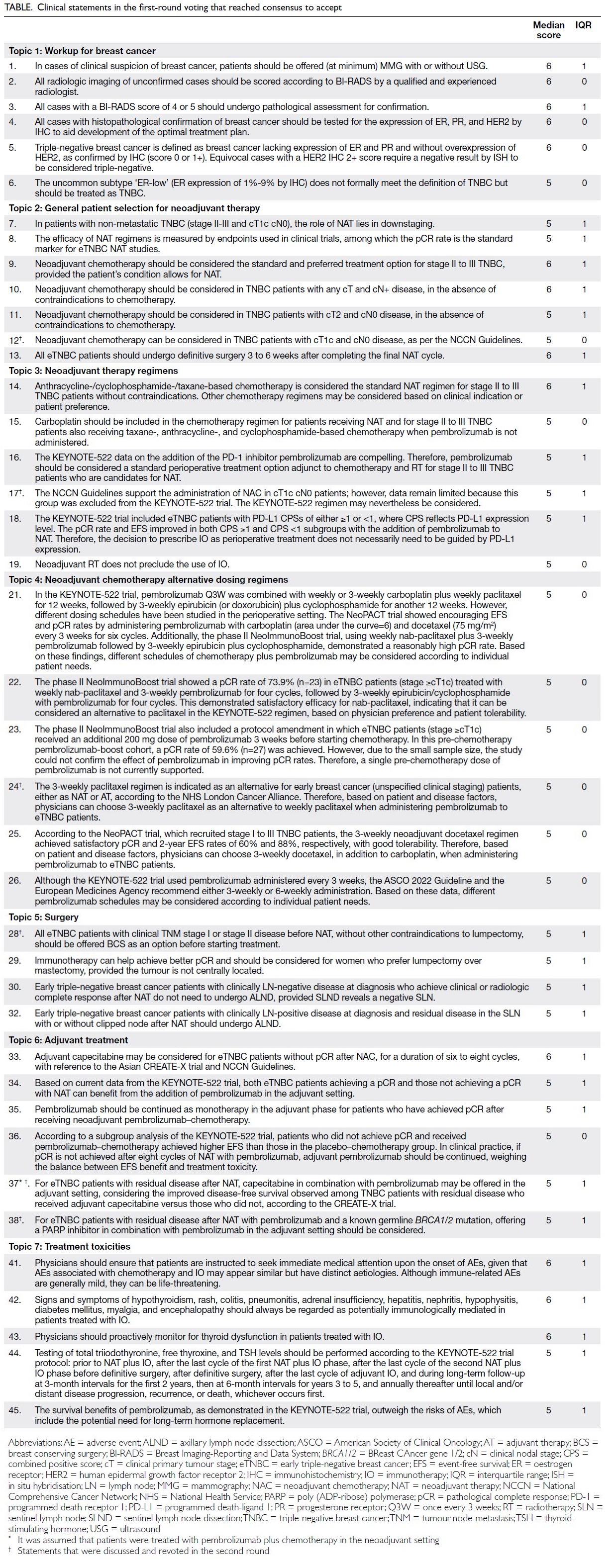
A modified Delphi panel was conducted on
seven topics encompassing 45 statements, covering
the workup for TNBC as well as neoadjuvant and
adjuvant treatment for eTNBC. Statements relating
to surgery were prepared by breast surgeons, whereas
statements concerning non-surgical interventions
were developed by oncologists. The statements were
generated with reference to established guidelines
and clinical trials, after a non-systematic search of
databases for literature published in English without
time restrictions. The levels of evidence and strength
of recommendations were determined using a two-level
grading system.12
In the first round, votes from 64 practising
healthcare professionals in Hong Kong—including
surgeons (n=21), clinical oncologists (n=36), and
medical oncologists (n=7)—were collected through
an online form using a six-point Likert scale:
Strongly disagree = 1; Disagree = 2; Slightly disagree
= 3; Slightly agree = 4; Agree = 5; Strongly agree = 6. No midpoint or neutral option was provided to
encourage definitive responses. Consensus to accept
(CTA) was defined as a median score ≥5 with an
interquartile range (IQR) ≤1.75. Consensus to reject
(CTR) was defined as a median score ≤2 with an
IQR ≤1.75. The results, including statements that
did not reach consensus, were discussed further by
16 senior panellists, who voted anonymously during
a consensus meeting. All panellists were invited to
review the manuscript contents to confirm the final
statements, as described in later sections. The first-and
second-round voting results are summarised in
the Table and online supplementary Tables 1 and 2.
All voting data were analysed using SPSS (Windows
version 28.0; IBM Corp, Armonk [NY], United
States) to determine consensus. Recommendations
were graded using the GRADE (Grading of
Recommendations Assessment, Development and
Evaluation) system as strong (grade 1) or weak
(grade 2); the quality of evidence was classified as
high (grade A), moderate (grade B), or low (grade
C).12 This manuscript follows the AGREE (Appraisal
of Guidelines Research and Evaluation) reporting
guideline.
Consensus statements
Workup for breast cancer
Respondents and panellists agreed that all women
with clinical suspicion of breast cancer should be
offered mammography, with or without ultrasound,
and that imaging should be scored according to the BI-RADS (Breast Imaging Reporting and Data
System) by a qualified and experienced radiologist.
The definition of TNBC was also highlighted,
referring to breast cancer that lacks expression of ER
and PR and does not exhibit overexpression of HER2.
Two key statements relating to the histopathology of
TNBC are presented below:
Statement 4: All cases with histopathological
confirmation of breast cancer should be tested for
the expression of oestrogen receptors, progesterone
receptors, and human epidermal growth factor
receptor 2 by immunohistochemistry to aid the
development of the optimal treatment plan. (CTA;
Recommendation: 1A)
Statement 6: The uncommon subtype ‘oestrogen
receptors–low’ (oestrogen receptor expression of
1%-9% by immunohistochemistry) does not formally
meet the definition of triple-negative breast cancer
but should be treated as triple-negative breast
cancer. (CTA; Recommendation: 2C)
It was agreed that assessment of ER/PR
expression and HER2 overexpression in breast
cancer is essential to facilitate treatment planning
and should be confirmed before treatment initiation.
The panel regarded ER-low–positive (1%-9% ER
expression) breast cancer as a biologically distinct
subgroup for which treatment consensus has not
yet been established, due to the uncertain benefit
of endocrine therapy.13 A prospective multicentre
registry study of 516 patients conducted between
2011 and 2019 showed that demographic and clinical
characteristics, as well as BRCA1/2 mutation status,
were comparable between ER-low breast cancer
and TNBC.14 The respondents therefore believed
that breast cancer exhibiting low ER expression on
immunohistochemistry should be treated as TNBC.
General patient selection for neoadjuvant
therapy
The importance of neoadjuvant therapy (NAT) for downstaging non–metastatic TNBC (non-mTNBC)
was generally agreed upon by respondents and
panellists. Patients with stage II to III disease or
node-negative cases with a primary tumour size
between 1 and 2 cm should be considered for NAT.
Definitive surgery should be performed within 3 to
6 weeks after completion of the final cycle of NAT.
Two key statements relating to NAC use for eTNBC
are discussed below:
Statement 9: Neoadjuvant chemotherapy should be
considered the standard and preferred treatment
option for stage II to III triple-negative breast
cancer, provided the patient’s condition allows for
neoadjuvant therapy. (CTA; Recommendation: 1A)
Statement 12: Neoadjuvant chemotherapy can be
considered in triple-negative breast cancer patients
with clinical tumour stage 1c (cT1c) and clinical
nodal stage 0 (cN0) disease, as per the National
Comprehensive Cancer Network Guidelines. (CTA;
Recommendation: 1C)
The St Gallen Consensus Conference
recommends adding carboplatin to neoadjuvant
paclitaxel, followed by anthracyclines and
cyclophosphamide, for stage II to III TNBC.15
The National Comprehensive Cancer Network
Guidelines state that preoperative systemic therapy
is preferred for TNBC patients at clinical stage ≥cT2
or ≥cN1 and can also be considered for cT1cN0.16
The American Society of Clinical Oncology
recommends offering an anthracycline- and taxane-containing
regimen in the neoadjuvant setting for
patients with TNBC at clinical stage cT1cN0M0,17
whereas the European Society for Medical Oncology
guidelines suggest NAT for TNBC patients with
cT1cN0 disease or greater.18 After reviewing these
guidelines, the panellists agreed on the use of NAT
for TNBC patients with a clinical tumour size of 1 to
2 cm and no palpable lymph nodes (LNs).
The panellists also noted that, in clinical
practice, establishing a multidisciplinary team
comprising surgeons and oncologists is essential
when developing a treatment plan, particularly for
patients who may be eligible for breast conserving
surgery (BCS) after NAT. Patient adherence to
treatment plans proposed by a multidisciplinary team
is reportedly higher, according to a retrospective
study conducted in Europe.19
Neoadjuvant therapy regimens
Anthracycline/cyclophosphamide/taxane-based
chemotherapy is the standard NAT regimen for
stage II to III TNBC.20 In addition to standard
chemotherapy, respondents and panellists agreed
that other regimens may be considered as clinically
indicated or according to patient preferences. The
addition of platinum agents and immune checkpoint
inhibitors should also be considered, given the
improved EFS observed in stage II or III TNBC
patients in recent clinical trials.9 21 Based on the
results of the KEYNOTE-522 trial, respondents and
panellists supported the addition of pembrolizumab
to NAT for TNBC, regardless of PD-L1 expression
level.8 9 Three key statements concerning the use of
pembrolizumab are highlighted below:
Statement 15: Carboplatin should be included in
the chemotherapy regimen for patients receiving
neoadjuvant therapy and for stage II to III triple-negative
breast cancer patients also receiving
taxane-, anthracycline-, and cyclophosphamide-based
chemotherapy when pembrolizumab is not
administered. (CTA; Recommendation: 1C)
Statement 16: The KEYNOTE-522 data on the
addition of the programmed death receptor
ligand 1 inhibitor pembrolizumab are compelling.
Therefore, pembrolizumab should be considered a
standard perioperative treatment option adjunct
to chemotherapy and radiotherapy for stage II
to III triple-negative breast cancer patients who
are candidates for neoadjuvant therapy. (CTA;
Recommendation: 1B)
Statement 17: The National Comprehensive Cancer
Network Guidelines support the administration
of neoadjuvant chemotherapy in clinical tumour
stage 1c (cT1c) and clinical nodal stage 0 (cN0)
patients; however, data remain limited because
this group was excluded from the KEYNOTE-522 trial. The KEYNOTE-522 regimen may
nevertheless be considered. (Neither CTA nor CTR;
Recommendation: 2C)
Respondents and panellists emphasised the
importance of adding carboplatin to backbone
chemotherapy in the NAT of TNBC. A meta-analysis
and systematic review of platinum-based NAT
across 11 randomised controlled trials involving
2946 patients suggested that platinum-based
chemotherapy was associated with a higher pCR rate
(40%) compared with platinum-free chemotherapy
(27%).22 Subgroup analysis showed that taxane plus
platinum chemotherapy increased the pCR rate
to 44.6% vs 27.8% for platinum-free treatment,
supporting the neoadjuvant use of carboplatin plus
taxane chemotherapy.22
The phase III KEYNOTE-522 trial
demonstrated that preoperative pembrolizumab plus
chemotherapy achieved a significantly higher pCR
rate (64.8% vs 51.2%; P<0.001) than chemotherapy
alone in untreated stage II to III TNBC patients.8
These promising findings were further supported by
the trial’s 60-month EFS rates, which were 81.3% and
72.3% in the pembrolizumab and control groups,
respectively.23
Patients with cT1a or cT1bN0 TNBC should
not be routinely offered NAT outside clinical trials;
guidelines suggest a case-by-case approach to
NAT for treating cT1cN0M0 disease.16 Although
combinations of immune checkpoint inhibitors and
chemotherapy have been extensively studied in three
phase II and III neoadjuvant trials (KEYNOTE-522,8 IMpassion031,24 and NeoImmunoBoost10),
none included cT1cN0 patients. Thus, the panel
concluded that there is insufficient evidence to
justify extrapolating the addition of immunotherapy
to chemotherapy for this patient group.
Panellists were divided on the use of immune
checkpoint inhibitors, such as pembrolizumab,
in all cT1N0 disease. Some noted that evidence
from phase III studies is currently limited, whereas
others supported the use of pembrolizumab in cT1N0 disease given its inclusion in the NeoPACT
trial.25 Nonetheless, individualised discussions and
multidisciplinary team consultations are encouraged
for each case before treatment.
Neoadjuvant chemotherapy alternative
dosing regimens
Dosing schedules may influence treatment
response, safety outcomes, and patient compliance.
Respondents and panellists were open to various
dosing regimens combining pembrolizumab with
platinum and taxane, followed by anthracyclines.6 10 25
Dose-dense anthracycline was not considered
an alternative to the 3-weekly schedule when
neoadjuvant pembrolizumab is administered.
Two key statements on 3-weekly and weekly
dosage schedules are highlighted below for further
discussion:
Statement 24: The 3-weekly paclitaxel regimen
is indicated as an alternative for early breast
cancer (unspecified clinical staging) patients,
either as neoadjuvant therapy or adjuvant therapy,
according to the National Health Service London
Cancer Alliance. Therefore, based on patient and
disease factors, physicians can choose 3-weekly
paclitaxel as an alternative to weekly paclitaxel
when administering pembrolizumab to early triple-negative
breast cancer patients. (Neither CTA nor
CTR; Recommendation: 2B)
Statement 25: According to the NeoPACT trial,
which recruited stage I to III triple-negative breast
cancer patients, the 3-weekly neoadjuvant docetaxel
regimen achieved satisfactory pathological complete
response and 2-year event-free survival rates of
60% and 88%, respectively, with good tolerability.
Therefore, based on patient and disease factors,
physicians can choose 3-weekly docetaxel, in
addition to carboplatin, when administering
pembrolizumab to early triple-negative breast
cancer patients. (CTA; Recommendation: 2C)
The National Health Service London Cancer
Alliance recommends administering paclitaxel once
every 3 weeks (Q3W) for four cycles in early breast
cancer.26 However, the E1199 trial investigated
the optimal dosing of docetaxel or paclitaxel after
anthracycline plus cyclophosphamide in 4954
patients with axillary LN-positive or high-risk
LN-negative breast cancer, including 1025 TNBC
patients.27 Although no difference was observed in
the primary comparisons of taxane type (docetaxel
vs paclitaxel) or schedule (3-weekly vs weekly), a
secondary analysis with a 10-year update reported
that weekly paclitaxel produced more favourable
survival outcomes than the 3-weekly schedule. In
TNBC patients, higher 10-year disease-free survival
(DFS) and OS were noted with weekly paclitaxel (Q1W) compared with Q3W (69% vs 58.7%; hazard
ratio [HR]=0.69; P=0.01 and 75.1% vs 65.6%; HR=0.69;
P=0.019, respectively), supporting the adjuvant
use of weekly paclitaxel.27 In the recent phase II
NeoPACT trial, the neoadjuvant combination of
pembrolizumab, carboplatin, and docetaxel Q3W
achieved a pCR rate of 58% (95% confidence interval
[95% CI]=48%-67%) and a 3-year EFS of 86% for all
patients.25 If validated in a phase III randomised
study, this combination may represent a future 3-weekly anthracycline-free chemoimmunotherapy
option for TNBC patients.25
The efficacy of paclitaxel Q3W remains
controversial. Although consensus was not reached,
all panellists participating in the discussion preferred
weekly paclitaxel (Q1W), considering its long-term
data on efficacy, tolerability, and toxicity, as well as
its consistency with the KEYNOTE-522 regimen,
which utilises weekly paclitaxel in combination with
pembrolizumab.8 9 The panellists did not consider
paclitaxel Q3W to be an optimal alternative to
weekly regimens but agreed that 3-weekly taxane
(docetaxel or paclitaxel) regimens may provide a
practical treatment schedule for selected patients.
Surgery
Respondents and panellists agreed that the addition
of immunotherapy to chemotherapy improves pCR
rates in patients who wish to undergo BCS after
NAT. For patients with clinically negative LNs at
diagnosis who achieve a complete response after
NAT, extensive axillary surgery may be omitted
if sentinel LN dissection reveals negative nodes.
However, the panellists did not support applying
the same approach to patients who had clinically
positive LNs at diagnosis.
One statement concerning the option of
offering BCS before the initiation of treatment was
discussed:
Statement 28: All early triple-negative breast cancer
patients with clinical tumour-node-metastasis stage
I or stage II disease before neoadjuvant therapy,
without other contraindications to lumpectomy,
should be offered breast conserving surgery as an
option before starting treatment. (Neither CTA nor
CTR; Recommendation: 1C)
According to the National Comprehensive
Cancer Network Guidelines,16 early-stage
(≤cT1cN0) operable breast cancer patients may
undergo upfront BCS or mastectomy with adjuvant
systemic therapy where indicated, whereas patients
with clinical stage ≥cT2 or ≥cN disease should be
treated with NAT. The European Society for Medical
Oncology guidelines state that BCS is the preferred
local treatment option for most early breast cancer
patients, but aggressive phenotypes such as eTNBC
should receive NAT first28; BCS should only be offered when the response to NAT is satisfactory.28
The 17th St Gallen International Guidelines also
recommend dose-dense anthracycline- and taxane-based
NAT for stage II or III eTNBC but do not
comment on stage I disease.29
The panellists declined to endorse the
statement, noting that NAT is a treatment option
for eTNBC patients but not a prerequisite for BCS
in stage I or II disease. However, it is noteworthy
that in-breast recurrences represent 5% to 15% of
all recurrence events in early-stage breast cancer
under contemporary BCS and RT management.30 31
Recurrence rates have continued to improve with
advances in therapy. In a recent meta-analysis of
14 studies involving 19 819 TNBC patients who
underwent BCS (plus radiotherapy) or mastectomy,
the pooled odds ratio for locoregional recurrence
was 0.64 (95% CI=0.48-0.85; P=0.002), the pooled
odds ratio for distant metastasis was 0.70 (95%
CI=0.53-0.94; P=0.02), and the pooled HR for
all-cause mortality was 0.78 (95% CI=0.69-0.89;
P<0.001) among patients who underwent BCS
relative to mastectomy.32 Another retrospective
study of 12 761 patients with T1-2N0M0 TNBC
also revealed significantly higher 5-year OS (89% vs
84.5%; P<0.001) and breast cancer–specific survival
(93% vs 91%; P<0.001) in patients receiving BCS
and radiotherapy compared with those undergoing
mastectomy alone.33 Both meta-analyses did not
report outcome differences between adjuvant
therapy with upfront BCS and NAT followed by
BCS in eTNBC. Given these encouraging data, the
panellists regarded the statement as unclear but
raised no objection to recommending upfront BCS
for selected patients with ≤cT1cN0 eTNBC. Risk
factors, including age, tumour grade, and disease
stage, should be considered when offering this
treatment option.
Adjuvant treatment
For patients with residual disease after neoadjuvant
pembrolizumab plus chemotherapy, adding
capecitabine to adjuvant pembrolizumab was
considered acceptable. However, consensus
was not reached among panellists regarding the
combined use of a poly (ADP-ribose) polymerase
inhibitor and pembrolizumab in the adjuvant setting
for patients with residual disease and a known
germline BRCA1/2 mutation (gBRCA1/2m), due to
variations in local testing practices for gBRCA1/2m.
Discussions of scenarios that may benefit from the
adjuvant use of pembrolizumab are summarised in
the two statements below:
Statement 34: Based on current data from the
KEYNOTE-522 trial, both early triple-negative
breast cancer patients achieving a pathological
complete response and those not achieving a pathological complete response with neoadjuvant
therapy can benefit from the addition of
pembrolizumab in the adjuvant setting. (CTA; Recommendation: 1B)
Statement 37: For early triple-negative breast cancer
patients with residual disease after neoadjuvant
therapy, capecitabine in combination with
pembrolizumab may be offered in the adjuvant
setting, considering the improved disease-free
survival observed among triple-negative breast
cancer patients with residual disease who received
adjuvant capecitabine versus those who did
not, according to the CREATE-X trial. (CTA; Recommendation: 2B)
According to the KEYNOTE-522 trial, patients
receiving perioperative pembrolizumab and NAC
demonstrated better EFS than those treated with
NAC alone (84.5% vs 76.8%, HR=0.63; 95% CI=0.48-0.82) at a median follow-up of 39.1 months.9 Further
EFS analysis based on pCR outcomes showed that
patients who did not achieve pCR also benefited
from the KEYNOTE-522 regimen (67.4% vs 56.8%,
HR=0.7; 95% CI=0.52-0.95).9 The panellists agreed
that for patients who did not achieve pCR after
neoadjuvant pembrolizumab plus chemotherapy,
adjuvant pembrolizumab—or pembrolizumab
combined with capecitabine—should be
administered.
Based on the CREATE-X (Capecitabine for
Residual Cancer as Adjuvant Therapy)34 and EA1131
trials,35 patients without a pCR after NAT may
benefit from adjuvant capecitabine. The phase III
CREATE-X study enrolled 910 HER2-negative breast
cancer patients with residual disease after NAT
containing anthracycline, taxane, or both. Those
who received standard treatment with capecitabine
demonstrated better long-term survival outcomes
than the control (capecitabine-free) group. Among
286 patients with residual TNBC, those receiving
adjuvant capecitabine achieved higher DFS (69.8%
vs 56.1%; HR=0.58; 95% CI=0.39-0.87) and OS
(78.8% vs 70.3%; HR=0.52; 95% CI=0.30-0.90) than
those in the control group at 5 years.34 Another
phase III EA1131 study of 410 patients with residual
TNBC after NAT also showed better 3-year invasive
DFS among those receiving adjuvant capecitabine
(49.4%; 95% CI=39.0%-59.0%) than among those
receiving adjuvant platinum (42.0%; 95% CI=30.5%-53.1%), although the difference was not statistically
significant.35
Despite the lack of mature data regarding
the adjuvant use of capecitabine in combination
with pembrolizumab, the KEYNOTE-522 study
demonstrated the additional benefit of perioperative
pembrolizumab with NAC without increasing
chemotherapy-related adverse effects in the
neoadjuvant setting.8 9 The panellists considered that adding capecitabine to pembrolizumab in patients
without pCR after NAT plus pembrolizumab
represents a clinically feasible option to improve
long-term survival outcomes in cases where residual
disease is observed after pembrolizumab-based NAT.
They noted that the combination of pembrolizumab
and capecitabine has been reported to be safe and
tolerable in mTNBC.36 However, further prospective
studies are required to determine the long-term
survival and safety benefits, as well as the optimal
dosing schedule, in eTNBC. The panellists ultimately
reached a consensus to accept this statement, adding
that adjuvant capecitabine with pembrolizumab may
be considered on a case-by-case basis.
Treatment toxicities
Respondents and panellists reached consensus on all
statements relating to treatment toxicities without
requiring further discussion in the second round.
In summary, for patients receiving immunotherapy
plus chemotherapy, clinicians should monitor for
potential immunotherapy-related adverse events,
which are generally mild in most patients but
may be life-threatening in some cases. Thyroid
function should be proactively monitored, given
that reversible destructive thyroiditis and overt
hypothyroidism commonly occur in patients
receiving pembrolizumab.37
Conclusion
The development of these consensus statements
on the management of eTNBC involved a
multidisciplinary panel of oncologists and breast
surgeons from public, private, and academic
institutions, providing a comprehensive overview
of clinical practice in Hong Kong. These statements
offer guidance to clinicians regarding the general
work-up, treatment, and use of immunotherapy for
TNBC patients who do not fit the patient profile
enrolled in the KEYNOTE-522 study.
Author contributions
Concept or design: PSY Cheung, W Yeo.
Acquisition of data: All authors.
Analysis or interpretation of data: PSY Cheung, W Yeo.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: PSY Cheung, W Yeo, YHY Chan, RCY Leung.
Acquisition of data: All authors.
Analysis or interpretation of data: PSY Cheung, W Yeo.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: PSY Cheung, W Yeo, YHY Chan, RCY Leung.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
CC Yau received speaker’s honoraria from Novartis and
Eli Lilly. AKC Leung is the Second Vice President of the
Hong Kong Breast Oncology Group. All other authors have
disclosed no conflicts of interest.
Acknowledgement
The authors acknowledge and thank all breast surgeons,
clinical oncologists, and medical oncologists in Hong Kong
who supported this consensus by voting during the first round
of the Delphi methodology.
Declaration
The consensus statement results were presented at The
Chinese University of Hong Kong Breast Cancer Meeting
(28-29 October 2023, Hong Kong) and as a poster presentation
at the American Society of Clinical Oncology Annual Meeting
2024 (31 May to 4 June 2024, Chicago, United States).
Funding/support
The study was funded by the Hong Kong Breast Cancer
Foundation Limited with the support of Merck Sharp and
Dohme (Asia) Limited. Medical writing support was provided
by MediPaper Medical Communications Limited. The funders
had no role in the study design, data collection/analysis/interpretation, or manuscript preparation.
Supplementary material
The supplementary material was provided by the authors and
some information may not have been peer reviewed. Accepted
supplementary material will be published as submitted by the
authors, without any editing or formatting. Any opinions
or recommendations discussed are solely those of the
author(s) and are not endorsed by the Hong Kong Academy
of Medicine and the Hong Kong Medical Association.
The Hong Kong Academy of Medicine and the Hong Kong
Medical Association disclaim all liability and responsibility
arising from any reliance placed on the content.
References
1. Ahn SG, Kim SJ, Kim C, Jeong J. Molecular classification of
triple-negative breast cancer. J Breast Cancer 2016;19:223-30. Crossref
2. Dent R, Trudeau M, Pritchard KI, et al. Triple-negative
breast cancer: clinical features and patterns of recurrence.
Clin Cancer Res 2007;13:4429-34. Crossref
3. Solinas C, Carbognin L, De Silva P, Criscitiello C,
Lambertini M. Tumor-infiltrating lymphocytes in breast
cancer according to tumor subtype: current state of the art.
Breast 2017;35:142-50. Crossref
4. Stanton SE, Adams S, Disis ML. Variation in the incidence
and magnitude of tumor-infiltrating lymphocytes in
breast cancer subtypes: a systematic review. JAMA Oncol
2016;2:1354-60. Crossref
5. Cortes J, Cescon DW, Rugo HS, et al. Pembrolizumab
plus chemotherapy versus placebo plus chemotherapy
for previously untreated locally recurrent inoperable or
metastatic triple-negative breast cancer (KEYNOTE-355):
a randomised, placebo-controlled, double-blind, phase 3
clinical trial. Lancet 2020;396:1817-28. Crossref
6. Cortes J, Rugo HS, Cescon DW, et al. Pembrolizumab plus
chemotherapy in advanced triple-negative breast cancer. N
Engl J Med 2022;387:217-26. Crossref
7. Schmid P, Adams S, Rugo HS, et al. Atezolizumab and nab-paclitaxel
in advanced triple-negative breast cancer. N Engl J Med 2018;379:2108-21. Crossref
8. Schmid P, Cortes J, Pusztai L, et al. Pembrolizumab for early
triple-negative breast cancer. N Engl J Med 2020;382:810-21. Crossref
9. Schmid P, Cortes J, Dent R, et al. Event-free survival with
pembrolizumab in early triple-negative breast cancer. N
Engl J Med 2022;386:556-67. Crossref
10. Fasching PA, Hein A, Kolberg HC, et al. Pembrolizumab
in combination with nab-paclitaxel for the treatment of
patients with early-stage triple-negative breast cancer—a
single-arm phase II trial (NeoImmunoboost, AGO-B-041).
Eur J Cancer 2023;184:1-9. Crossref
11. Yeo W, Chan YH, Leung RC, et al. Expert consensus
recommendations on the daily clinical use of
pembrolizumab for early triple-negative breast cancer
[abstract]. J Clin Oncol 2024;42(Suppl 16):e12521. Crossref
12. Guyatt G, Gutterman D, Baumann MH, et al. Grading
strength of recommendations and quality of evidence in
clinical guidelines: report from an American College of
Chest Physicians task force. Chest 2006;129:174-81. Crossref
13. Malainou CP, Stachika N, Damianou AK, et al. Estrogen-receptor-low–positive breast cancer: pathological and clinical perspectives. Curr Oncol 2023;30:9734-45. Crossref
14. Yoder R, Kimler BF, Staley JM, et al. Impact of low versus
negative estrogen/progesterone receptor status on clinico-pathologic
characteristics and survival outcomes in HER2-negative breast cancer. NPJ Breast Cancer 2022;8:80. Crossref
15. Curigliano G, Burstein HJ, Gnant M, et al. Understanding
breast cancer complexity to improve patient outcomes:
The St Gallen International Consensus Conference for the
Primary Therapy of Individuals with Early Breast Cancer
2023. Ann Oncol 2023;34:970-86. Crossref
16. National Comprehensive Cancer Network. NCCN
Guidelines. Breast Cancer. Available from: www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed 2 Sep 2023. Crossref
17. Korde LA, Somerfield MR, Carey LA, et al. Neoadjuvant
chemotherapy, endocrine therapy, and targeted therapy for
breast cancer: ASCO Guideline. J Clin Oncol 2021;39:1485-505. Crossref
18. Loibl S, André F, Bachelot T, et al. Early breast cancer:
ESMO Clinical Practice Guideline for diagnosis, treatment
and follow-up. Ann Oncol 2024;35:159-82. Crossref
19. Fancellu A, Pasqualitto V, Cottu P, et al. The importance of
the multidisciplinary team in the decision-making process
of patients undergoing neoadjuvant chemotherapy for
breast cancer. Updates Surg 2024;76:1919-26. Crossref
20. von Minckwitz G, Martin M. Neoadjuvant treatments for
triple-negative breast cancer (TNBC). Ann Oncol 2012;23
Suppl 6:vi35-9. Crossref
21. Geyer CE, Sikov WM, Huober J, et al. Long-term efficacy
and safety of addition of carboplatin with or without
veliparib to standard neoadjuvant chemotherapy in
triple-negative breast cancer: 4-year follow-up data from
BrighTNess, a randomized phase III trial. Ann Oncol
2022;33:384-94. Crossref
22. Pandy JG, Balolong-Garcia JC, Cruz-Ordinario MV, Que FV.
Triple negative breast cancer and platinum-based systemic
treatment: a meta-analysis and systematic review. BMC
Cancer 2019;19:1065. Crossref
23. Schmid P, Cortés J, Dent RA, et al. LBA18 Pembrolizumab
or placebo plus chemotherapy followed by pembrolizumab
or placebo for early-stage TNBC: updated EFS results from the phase III KEYNOTE-522 study [abstract]. Ann Oncol
2023;34 Suppl:S1257. Crossref
24. Mittendorf EA, Zhang H, Barrios CH, et al. Neoadjuvant
atezolizumab in combination with sequential nab-paclitaxel
and anthracycline-based chemotherapy versus placebo and
chemotherapy in patients with early-stage triple-negative
breast cancer (IMpassion031): a randomised, double-blind,
phase 3 trial. Lancet 2020;396:1090-100. Crossref
25. Sharma P, Stecklein SR, Yoder R, et al. Clinical and
biomarker findings of neoadjuvant pembrolizumab and
carboplatin plus docetaxel in triple-negative breast cancer:
NeoPACT phase 2 clinical trial. JAMA Oncol 2024;10:227-35. Crossref
26. London Cancer Alliance. LCA Breast Cancer Clinical
Guidelines. Oct 2013. Available from: https://www.transformationpartners.nhs.uk/wp-content/uploads/2020/10/LCA-Breast-Cancer-Clinical-Guidelines.pdf. Accessed 5 Nov 2025.
27. Sparano JA, Zhao F, Martino S, Ligibel JA, et al. Long-term
follow-up of the E1199 phase III trial evaluating the role of
taxane and schedule in operable breast cancer. J Clin Oncol
2015;33:2353-60. Crossref
28. Cardoso F, Kyriakides S, Ohno S, et al. Early breast
cancer: ESMO Clinical Practice Guidelines for diagnosis,
treatment and follow-up. Ann Oncol 2019;30:1194-220. Crossref
29. Burstein HJ, Curigliano G, Thürlimann B, et al. Customizing
local and systemic therapies for women with early breast
cancer: the St. Gallen International Consensus Guidelines
for treatment of early breast cancer 2021. Ann Oncol
2021;32:1216-35. Crossref
30. Sestak I, Cuzick J, Bonanni B, et al. Abstract GS2-02:
12-year results of anastrozole versus tamoxifen for the prevention of breast cancer in postmenopausal women
with locally excised ductal carcinoma in-situ [abstract].
Cancer Res 2021;81 Suppl 4:GS2-02. Crossref
31. Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up
of a randomized trial comparing total mastectomy,
lumpectomy, and lumpectomy plus irradiation for
the treatment of invasive breast cancer. N Engl J Med
2002;347:1233-41. Crossref
32. Fancellu A, Houssami N, Sanna V, Porcu A, Ninniri C,
Marinovich ML. Outcomes after breast-conserving
surgery or mastectomy in patients with triple-negative
breast cancer: meta-analysis. Br J Surg 2021;108:760-8. Crossref
33. Saifi O, Chahrour MA, Li Z, et al. Is breast conservation
superior to mastectomy in early stage triple negative breast
cancer? Breast 2022;62:144-51. Crossref
34. Masuda N, Lee SJ, Ohtani S, et al. Adjuvant capecitabine
for breast cancer after preoperative chemotherapy. N Engl
J Med 2017;376:2147-59. Crossref
35. Mayer IA, Zhao F, Arteaga CL, et al. Randomized phase III
postoperative trial of platinum-based chemotherapy versus
capecitabine in patients with residual triple-negative breast
cancer following neoadjuvant chemotherapy: ECOG-ACRIN
EA1131. J Clin Oncol 2021;39:2539-51. Crossref
36. Page DB, Pucilowska J, Chun B, et al. A phase Ib trial of
pembrolizumab plus paclitaxel or flat-dose capecitabine in
1st/2nd line metastatic triple-negative breast cancer. NPJ
Breast Cancer 2023;9:53. Crossref
37. Delivanis DA, Gustafson MP, Bornschlegl S, et al.
Pembrolizumab-induced thyroiditis: comprehensive
clinical review and insights into underlying involved
mechanisms. J Clin Endocrinol Metab 2017;102:2770-80. Crossref