Hong Kong Med J 2025;31:Epub 9 Dec 2025
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Improving efficiency and effectiveness of workplace-based assessment workshop in postgraduate medical education using a conjoint design
HY So, FHKAM (Anaesthesiology), MHPE1; Eddy WY Wong, FHKCORL, FRCSEd (ORL)2; Albert KM Chan, FHKCA, MHPE1; George KC Wong, MD, FCSHK1; Jessica YP Law, FHKCOG, MHQS (Harvard)3; PT Chan, FHKCOS, MMEd1; CM Ngai, FHKCORL, FRCS (Edin)2
1 The Jockey Club Institute for Medical Education and Development, Hong Kong Academy of Medicine, Hong Kong SAR, China
2 The Hong Kong College of Otorhinolaryngologists, Hong Kong SAR, China
3 Department of Obstetrics and Gynaecology, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China
Corresponding author: Dr HY So (sohingyu@fellow.hkam.hk)
Abstract
Introduction: Faculty development for trainers and
nurturing feedback literacy in trainees is crucial for
effective workplace-based assessments (WBAs) to
support trainee competency development. Separate
training sessions for trainers and trainees can be
challenging when resources are limited. Combined
training can optimise resources and foster mutual
understanding, although such approaches face
challenges related to power dynamics. This study
aimed to evaluate the effectiveness of a conjoint
WBA workshop in enhancing trainer engagement,
improving trainee feedback literacy, and exploring
the benefits and challenges of integrating trainers
and trainees in a shared learning environment.
Methods: A mixed-methods study was conducted
with 13 trainers and five trainees from the Hong Kong
College of Otorhinolaryngologists. Quantitative
data were collected using the Feedback Literacy
Behaviour Scale for trainees and the Continuing
Professional Development–Reaction Questionnaire
for trainers. Pre- and post-intervention comparisons
were analysed using paired t tests. Qualitative data
from focus group interviews were thematically
analysed.
Results: Quantitative analysis showed statistically
significant increases in trainee feedback literacy
(P<0.001) and improvements in trainers’ beliefs
about capabilities and engagement intentions
(P<0.05). The qualitative analysis supported these findings and identified three key factors: mutual
understanding, clarification of the WBA purpose,
and effective instructional design. Participants
valued the mutual understanding fostered in the
conjoint setting, which aligned expectations and
created a supportive learning environment.
Conclusion: Conjoint WBA workshops may
effectively promote trainer engagement and trainee
feedback literacy, aligning expectations and fostering
a positive feedback culture. Further research is
needed to explore the longitudinal impact and
applicability to other specialties.
New knowledge added by this study
- Trainers and trainees learning together in the same workplace-based assessment (WBA) workshop facilitates effective mutual learning.
- Despite potential power dynamics, psychological safety can be maintained in this setting.
- Collaboration strengthens trainees’ trust in the value of WBA as a tool for learning.
- Conjoint training can be considered an alternative for organising WBA workshops.
- The Hong Kong Academy of Medicine should support further studies on this design to enhance the effectiveness of WBA workshops.
Introduction
Competency-based medical education (CBME)
emphasises the assessment of trainees through direct
observation and feedback using workplace-based
assessments (WBA).1 These assessments are designed to support continuous learning and competency
development through meaningful feedback.2 Effective
implementation of WBA requires trainers who are
willing and able to provide constructive feedback,3 4 5
and trainees who are motivated to seek and use feedback. This active engagement with feedback is
the essence of feedback literacy, defined by Carless
and Boud6 as “the understandings, capacities, and
dispositions needed to make sense of information
and use it to enhance work or learning strategies”.
The construct of intention, based on the theory of
planned behaviour, highlights that an individual’s
willingness to perform a behaviour is influenced
by their attitudes, subjective norms, and perceived
behavioural control.7 Intention is emphasised as
the best predictor of behaviour, especially where
constraints or barriers exist. In the context of WBA,
focusing on intention helps us understand the
underlying motivations and readiness of trainers and
trainees to engage in feedback practices. Trainers’
intentions are shaped by their beliefs about the value
of feedback, the expectations of peers, and their
confidence in their ability to provide that feedback.
Dawson et al,8 building on the works of Carless and
Boud6 and Molloy et al,9 conceptualised feedback
literacy as five key skills: seeking feedback, making
sense of information, using feedback, managing
emotional responses, and providing feedback. Based
on this framework, effective training is essential for
fostering engagement and capability in meaningful
feedback practices.
Faculty development is often implemented to
enhance trainers’ skills, whereas separate sessions aim to build feedback literacy among trainees.
However, specialties with small numbers of trainers
and trainees face unique challenges in implementing
WBA, including limited opportunities to conduct
separate training sessions. A conjoint WBA
workshop, where both groups train together, may offer
an innovative solution to these constraints. Potential
benefits include promoting mutual understanding,
aligning feedback practices, and fostering a
consistent approach to WBA implementation.10
However, concerns regarding power imbalances and
psychological safety in mixed-group settings could
undermine its effectiveness.11 Thus far, there have
been no studies regarding such conjoint workshops;
the actual participant experience, including potential
advantages and disadvantages, remains unexplored.
Therefore, this study aimed to address the following research questions:
- Can conjoint training improve the intention of trainers to participate in WBA?
- Can conjoint training improve the feedback literacy of trainees?
- What are the experiences of trainers in a conjoint training setting?
- What are the experiences of trainees in a conjoint training setting?
Methods
This study was designed according to the requirements
of the SQUIRE-EDU (Standards for QUality
Improvement Reporting Excellence in Education)
guidelines for educational improvement.12
Study setting
The study was conducted with trainers and trainees
of the Hong Kong College of Otorhinolaryngologists
(HKCORL), a specialty college under the Hong
Kong Academy of Medicine. The HKCORL is
responsible for training and accrediting specialists in
otorhinolaryngology, and has been integrating WBAs
into its training curriculum since 2021. The College
currently has a total of 206 fellows, 57 of whom
are trainers. In May 2023, 20 trainers participated
in a WBA workshop specifically designed for
them. During the first 2 years, basic surgical
trainees are under the Hong Kong Intercollegiate
Board of Surgical Colleges and rotate through
different surgical specialties. Specialist training in
otorhinolaryngology takes place only during the 4
years of higher training. Over the past 5 years, the
annual intake of higher trainees has ranged from
four to 11. Currently, there are 31 higher trainees,
26 of whom participated in a WBA workshop for
trainees held in September 2023. Relationships
among fellows and trainees are strengthened
through regular training courses, academic lectures,
workshops, and an annual scientific meeting, complemented by active participation from the
Young Fellows Chapter to enhance engagement
in College activities. Camaraderie is also fostered
through sports activities and social events.
Participant sampling and recruitment
All participants in the workshop were invited by
email to participate in this study on a voluntary
basis. All 13 trainers and five trainees enrolled in
the workshop volunteered to participate in the
study. The cohort of trainers was relatively young; 11
were within 10 years of obtaining their fellowship,
and seven had only 1 to 2 years of experience as
specialists.
Instructional design
The 4-hour workshop was designed based on the
first principles of instruction, emphasising task-centred
learning as the core instructional approach.13
Participants engaged in two authentic learning
tasks: procedural-based assessment and case-based
discussion, each followed by guided reflection. These
tasks provided opportunities to practise giving and
receiving feedback, which was the main focus of the
workshop.
To prepare for these tasks, participants first
completed a pre-course e-learning module consisting
of five interactive videos (total duration: 53 minutes).
These videos introduced essential concepts,
including CBME, self-regulated learning, feedback
literacy, and the procedures of WBA. The workshop
began with an activity to establish psychological
safety, following the recommendations of Rudolph
et al,14 ensuring that participants felt comfortable to
learn and engage openly. Subsequently, participants’
knowledge was reactivated through interactive
lectures and demonstrations, effectively preparing
them for the practice activities.
Quantitative measures
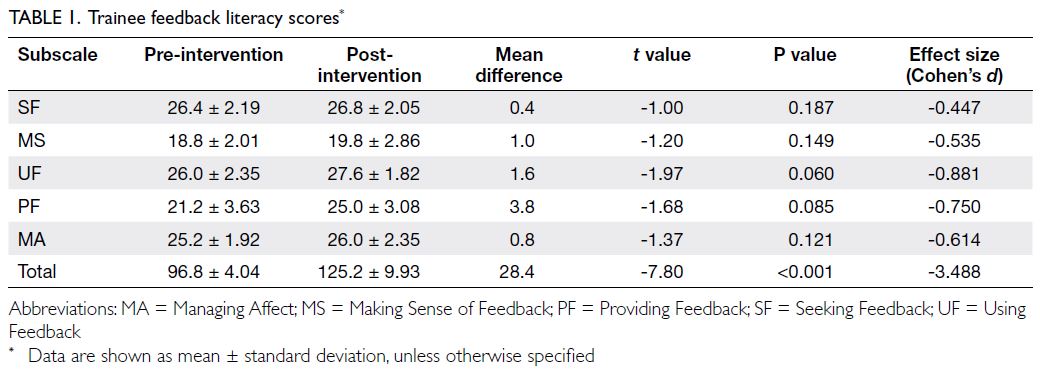
- Trainee feedback literacy: The Feedback Literacy Behaviour Scale was used to assess changes in trainees’ feedback literacy. It measures five subscales: Seeking Feedback, Making Sense of Feedback, Using Feedback, Providing Feedback, and Managing Affect.8
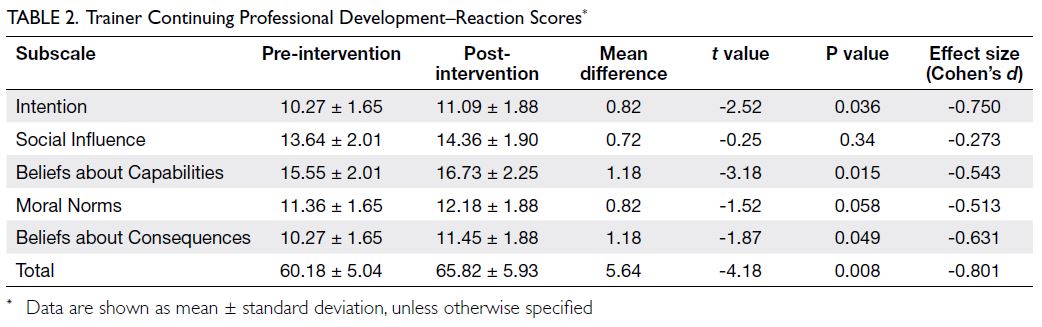
- Trainer engagement in WBA: Trainers’ engagement was measured using the Continuing Professional Development (CPD)–Reaction Questionnaire, based on social cognitive theories (theory of planned behaviour and Triandis’ theory of interpersonal behaviour). It measures intention, social influence, beliefs about capabilities, beliefs about consequences, and moral norms.7 15 16
Both surveys were administered before
participants began their e-learning and repeated after completion of the workshop.
Statistical analysis
Paired t tests were utilised to compare pre- and post-intervention
scores for both groups because this
method offers more precise estimates of the effect
and improved control over confounding variables
compared with an unpaired t test, particularly
given the small sample size. Descriptive statistics,
including means, standard deviations, and Cohen’s d
effect sizes, were calculated for each measure using
Jamovi (desktop version 2.3.28).17
Qualitative data collection and analysis
Separate focus group interviews were conducted
for trainers and trainees immediately after the
workshop, using Cantonese. The two moderators
were research staff trained by the authors. Semi-structured
interviews were conducted using an
interview guide created by the authors (online
Appendix). The interviews were audio-recorded,
anonymised, and transcribed verbatim. Transcripts
were analysed using Braun and Clarke’s thematic
analysis approach,18 assisted by ATLAS.ti software
(version 8.4.5; ATLAS.ti Scientific Software
Development, Berlin, Germany).19
Member checking
To enhance the credibility of the qualitative findings,
results were sent back to participants after thematic
analysis to confirm whether they agreed with the
interpretation and whether they wished to share
additional views. This process helped strengthen the
credibility of the qualitative findings.
Reflexivity
The first author, an intensivist and educationist with
a Master’s degree in Health Professions Education,
played a key role in designing the conjoint workshop
and framing WBA as a learning tool. The second
author, a consultant otorhinolaryngologist and
CBME advocate, proposed the joint training
concept to address challenges in organising
separate trainer and trainee sessions. Support
from the seventh author, president of HKCORL,
was critical for workshop implementation. Other
authors contributed diverse clinical and educational
expertise: the third author, a consultant anaesthetist
and faculty development chair of the Jockey Club
Institute for Medical Education and Development
of the Hong Kong Academy of Medicine; the fifth
author, an obstetrics and gynaecology consultant
with expertise in healthcare quality and simulation;
the sixth author, an orthopaedic surgeon and former
college censor; and the fourth author, a neurosurgeon
experienced in WBA workshops.
Their collective advocacy for CBME and WBA
informed the study design and interpretation. While
offering rich, multifaceted insights into WBA, this
commitment may have influenced the emphasis on
the conjoint workshop’s benefits, shaping research
questions and conclusions accordingly.
Results
Quantitative findings
Among the trainees, the total Feedback Literacy
Score significantly increased (pre=96.8 ± 4.04,
post=125.2 ± 9.93; P<0.001), associated with a large
effect size (d= –3.488). There was no statistically
significant difference in the subscales of the Feedback
Literacy Score (Table 1).
Among the trainers, the CPD–Reaction Scores
showed statistically significant improvement in
intention (pre=10.27 ± 1.65, post=11.09 ± 1.88;
P=0.036), beliefs about capabilities (pre=15.55 ±
2.01, post=16.73 ± 2.25; P=0.015), beliefs about
consequences (pre=10.27 ± 1.65, post=11.45 ± 1.88; P=0.049), and total score (pre=60.18 ± 5.04,
post=65.82 ± 5.93; P=0.008). The effect sizes
were moderate to large for intention (d= –0.750),
moderate for beliefs about capabilities (d= –0.543)
and beliefs about consequences (d= –0.631), and
large for the total score (d= –0.801) [Table 2].
Qualitative findings
Trainee focus group analysis
Four themes were identified: understanding WBA
assessment, enhancing feedback literacy, presence
of trainers in the workshop, and workshop design
and delivery. Subthemes and quotations under each
theme are listed in online supplementary Table 1.
Trainer focus group analysis
Four themes were identified: perceptions of WBA, improvement in feedback skills, presence of trainees
in the workshop, and workshop design and delivery.
Subthemes and quotations under each theme are
listed in online supplementary Table 2.
Discussion
This mixed-methods study evaluated the impact of a
conjoint WBA workshop designed to enhance both
trainer intention to participate in WBA and trainee
feedback literacy. The quantitative and qualitative
data converged to show that the conjoint workshop
improved trainer intention and appreciation of
feedback skills; it also enhanced trainee feedback
literacy and confidence in managing feedback during
their learning process. Specifically, the quantitative
results showed statistically significant improvement in trainer intention to participate in WBA as measured
by the CPD–Reaction Questionnaire, and in trainee
feedback literacy as measured by the Feedback
Literacy Behaviour Score. Moreover, the qualitative
findings suggested that trainers appreciated the use
of open-ended questions and integration of feedback
into micro-moments as valuable strategies, whereas
trainees reported increased confidence in managing
feedback and constructively applying it to their
learning processes.
Through analysis of the qualitative data, we
also identified three key factors that contributed
to these findings: mutual understanding between
trainers and trainees, clarification of the purpose of
WBA, and effective instructional design.
Mutual understanding between trainers and
trainees
A key finding of this study was the positive reception
of the mixed-group learning experience. Both
trainers and trainees valued the opportunity to
directly engage with each other, which fostered
mutual understanding of the assessment process
and reduced discrepancies in feedback practices.
Notably, the absence of prominent power dynamics
was striking. This may be partially attributed to
the relatively young cohort of trainers, which likely
fostered a more collaborative atmosphere. Although
previous literature suggests that hierarchical
structures can hinder open communication in
feedback settings,11 the present study demonstrated
that in contexts with flatter hierarchies, conjoint
workshops can be highly effective. Trainees
indicated that the emphasis on psychological
safety during the workshop helped prepare them
for meaningful participation. Adherence to the
recommendations of Rudolph et al14 to establish a
safe environment likely contributed to this positive
outcome. The close relationships already present
between trainers and trainees within this small
specialty could also have contributed. Existing
literature supports the importance of trainer–trainee
relationships in WBA.4 20 Interactions within this
psychologically safe environment facilitated a more
unified understanding of assessment standards and
expectations, which helped minimise discrepancies
in feedback practices. This alignment fostered trust
that both trainers and trainees were working towards
the shared goal of using WBA for learning purposes.
Our qualitative findings indicated that both
groups reported a highly positive experience. The
distinction lay in the focus: trainees emphasised
gains in feedback literacy and confidence, whereas
trainers valued new practical strategies and
enhanced mutual understanding. According to the
conceptual model of Castanelli et al,21 the level of
trust in supervisors influences trainees’ perceptions
of WBA. When trust is low, WBAs are regarded as performance evaluations, leading trainees to
adopt risk-minimising strategies.22 Conversely,
when trust is high, trainees perceive WBA as an
assessment for learning, making them more willing
to embrace vulnerability. Our findings suggest that,
with appropriate measures to ensure psychological
safety, a combined workshop setting may help align
expectations, create a shared understanding of WBA
practices, and strengthen trainees’ trust in their
trainers.
Clarification of the purpose of
workplace-based assessment
Both trainers and trainees recognised that WBA
serves as a formative tool that guides reflective
practice and enhances clinical competence. This
understanding is crucial because it aligns with
the principles of adult learning, particularly the
notion that adults are self-directed learners who
take responsibility for their own education.23 When
both trainers and trainees appreciate that WBA
facilitates reflective practice, they engage in self-directed
learning by utilising feedback to critically
analyse their clinical performance. This process
empowers them to identify areas for improvement
and take actionable steps towards enhancing their
skills. Moreover, adults are motivated to learn when
the material is directly relevant to their professional
needs.23 In this context, WBA’s role in guiding clinical
competence is highly pertinent because it connects
seamlessly with daily practice. Thus, WBA not only
fosters a culture of continuous improvement but
also effectively motivates adult learners by linking
assessment to professional development. However,
motivation alone is insufficient. Participants also
noted barriers such as time constraints in the
clinical setting and the need for effective evaluation
of outcomes. These issues must be addressed to
ensure that motivation remains long-lasting and
that trainees continue to meaningfully engage with
WBAs in their everyday practice.
Effective instructional design
The workshop was designed based on the first
principles of instruction, an evidence-based model
that emphasises moving beyond memorisation to
active knowledge application through real-world
tasks.13 24 This approach encourages learners to
engage in practice, which is often challenging and
requires specific support. To address this, support is
twofold: cognitive and affective. Cognitive support
helps learners understand key concepts through pre-course
e-learning, reactivation of prior knowledge,
demonstration, and facilitated reflection.13 Affective
support focuses on ensuring psychological safety,
which is crucial for effective engagement in practice.14
While overall improvement reflects the combined effect of e-learning and the workshop, the qualitative
data indicate that the interactive, conjoint nature
of the workshop itself was the primary catalyst for
enhancing mutual understanding and feedback
skills. Our analysis revealed that participants valued
this design and highlighted two additional elements
that supported their learning: cognitive aids and
peer feedback.
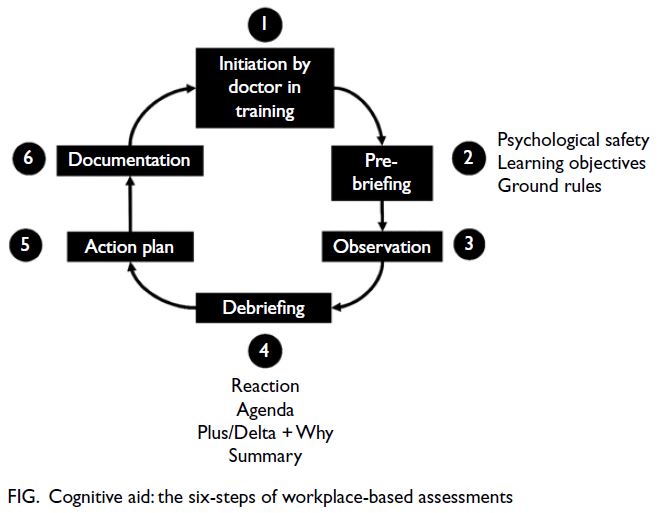
During the course, we used cognitive aids to
remind participants of this six-step framework (Fig),
and they found the use of such a framework effective.
Workplace-based assessments consist of recurrent
constituent skills—the steps to follow—and non-recurrent
constituent skills (eg, how to respond in
the debriefing conversation). The use of a structured
framework and just-in-time information, such as
cognitive aids, has been shown to effectively support
the learning of recurrent skills.25
During the guided reflection, we also engaged
participants in peer feedback. Our analysis showed
that participants found this practice enhanced their
learning. Peer feedback enhances metacognitive
perceptions by encouraging learners to reflect on
their understanding and performance in relation to
their peers. This fosters self-awareness as learners
evaluate their work against others’, facilitating deeper
insights into strengths and areas for improvement.26
There is evidence demonstrating the effectiveness of
peer feedback in enhancing feedback literacy.27 28
Nonetheless, participants noted that the
workshop could be improved by providing clearer
instructions for role-playing exercises and using more
medical-related cases for demonstration. Effective
instruction is important. According to cognitive load
theory, ineffective guidance can increase extrinsic
cognitive load and impair learning, especially when the task itself is already demanding.29 We used a
movie-based scenario not related to medicine to
make the activity fun and interesting. However, the
participants’ comment is valid, considering evidence
that similarity between demonstration and practice is
crucial for effective learning. When demonstrations
closely resemble real-life applications, learners
can better understand and apply concepts. This
alignment enhances procedural knowledge, enabling
learners to transition from observation to imitation
and, eventually, autonomous practice. Furthermore,
relevant demonstrations foster engagement and allow
immediate feedback, which reinforces learning.30 31
Future workshops should focus on improving these
aspects for better learning outcomes.
Limitations and future directions
This study had some limitations. The quantitative
findings are constrained by the small sample
size, particularly among trainees (n=5), which
limits statistical power. Furthermore, although
participation in the workshop was encouraged by
the College, the sample may still reflect a group
more engaged in training initiatives, potentially
affecting generalisability. While the qualitative
data provided rich insights into participants’
experiences, a larger cohort could offer a broader
understanding of the impact of this educational
intervention. Additionally, the study did not assess
long-term changes in behaviour or practice, which
are needed to determine sustained effects of the
conjoint training on WBA implementation. Future
studies could explore the longitudinal impact of
such workshops and investigate their applicability in
larger specialties where power dynamics might differ.
It would also be valuable to assess the scalability of
conjoint workshops in different contexts, particularly
those with more complex hierarchical structures,
to better understand their potential for broader
implementation.
Conclusion
This study provides evidence that conjoint WBA
workshops for trainers and trainees may effectively
enhance trainee feedback literacy and trainer
engagement in CBME. The mixed-group learning
experience promoted mutual understanding
and aligned feedback practices without creating
significant power imbalances, fostering positive
trainer–trainee interactions and enhancing trust,
provided measures are taken to ensure psychological
safety. Despite the positive outcomes, the study’s
limitations, including its small sample size and lack
of long-term follow-up, should be considered. Future
research could explore the longitudinal impact of
conjoint workshops and their applicability in larger
specialties with more complex power dynamics.
Author contributions
Concept or design: HY So, EWY Wong.
Acquisition of data: HY So, CM Ngai.
Analysis or interpretation of data: HY So, AKM Chan, GKC Wong.
Drafting of the manuscript: HY So.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: HY So, CM Ngai.
Analysis or interpretation of data: HY So, AKM Chan, GKC Wong.
Drafting of the manuscript: HY So.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank Mr CF Chan and Ms Cathy Ma of the
Jockey Club Institute for Medical Education and Development
of Hong Kong Academy of Medicine for valuable assistance
in moderating the focus group discussions and preparing
the transcripts. The authors also appreciate the logistical
support provided by Ms Cindy Leung of The Hong Kong
College of Otorhinolaryngologists, as well as Mr CF Chan, Ms
Cathy Ma, and Ms Jojo Lee of the Jockey Club Institute for
Medical Education and Development of Hong Kong Academy
of Medicine in organising the workshop. Additionally, the
authors wish to express their heartfelt thanks to Professor Jack
Pun from the Department of English at The Chinese University
of Hong Kong and Professor Stanley Sau-ching Wong from
the Department of Anaesthesiology at The University of Hong
Kong for insightful contributions to the preparation of the
manuscript.
Declaration
Findings from this study were presented at AMEE 2025 of the
International Association for Health Professions Education,
23-27 August 2025, Barcelona, Spain.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This research was approved by the Survey and Behavioural
Research Ethics Committee of The Chinese University of Hong
Kong, Hong Kong (Ref No.: SBRE-23-0855). Information
sheets regarding the study were provided to all participants,
and signed consent was obtained from each participant prior
to the study
Supplementary material
The supplementary material was provided by the authors and
some information may not have been peer reviewed. Accepted
supplementary material will be published as submitted by the
authors, without any editing or formatting. Any opinions
or recommendations discussed are solely those of the
author(s) and are not endorsed by the Hong Kong Academy
of Medicine and the Hong Kong Medical Association.
The Hong Kong Academy of Medicine and the Hong Kong
Medical Association disclaim all liability and responsibility arising from any reliance placed on the content.
References
1. So HY, Choi YF, Chan PT, Chan AK, Ng GW, Wong GK.
Workplace-based assessments: what, why, and how to
implement? Hong Kong Med J 2024;30:250-4. Crossref
2. Holmboe ES, Sherbino J, Long DM, Swing SR, Frank JR.
The role of assessment in competency-based medical
education. Med Teach 2010;32:676-82. Crossref
3. Anderson HL, Kurtz J, West DC. Implementation and
use of workplace-based assessment in clinical learning
environments: a scoping review. Acad Med 2021;96:S164-74. Crossref
4. Massie J, Ali JM. Workplace-based assessment: a
review of user perceptions and strategies to address the
identified shortcomings. Adv Heal Sci Educ Theory Pract
2016;21:455-73. Crossref
5. Lörwald AC, Lahner FM, Mooser B, et al. Influences on the
implementation of Mini-CEX and DOPS for postgraduate
medical trainees’ learning: a grounded theory study. Med
Teach 2019;41:448-56. Crossref
6. Carless D, Boud D. The development of student feedback
literacy: enabling uptake of feedback. Assess & Eval High
Educ 2018;43:1315-25. Crossref
7. Ajzen I. The theory of planned behaviour. Organ Behav
Hum Decis Processes 1991;50:179-211. Crossref
8. Dawson P, Yan Z, Lipnevich A, Tai J, Boud D, Mahoney P.
Measuring what learners do in feedback: the Feedback
Literacy Behaviour Scale. Assess Eval High Educ
2023;49:348-62. Crossref
9. Molloy E, Boud D, Henderson M. Developing a learning-centred
framework for feedback literacy. Assess Eval High
Educ 2020;45:527-40. Crossref
10. Illingworth P, Chelvanayagam S. Benefits of
interprofessional education in health care. Br J Nurs
2007;16:121-4. Crossref
11. Brooks AK. Power and the production of knowledge:
collective team learning in work organizations. Hum
Resour Dev Q 1994;5:213-35. Crossref
12. Ogrinc G, Armstrong GE, Dolansky MA, Singh MK,
Davies L. SQUIRE-EDU (Standards for QUality
Improvement Reporting Excellence in Education):
publication guidelines for educational improvement. Acad
Med 2019;94:1461-70. Crossref
13. Merrill MD. First principles of instruction. In: Reigeluth CM,
Carr-Chellman AA, editors. Instructional Design Theories
and Models: Building a Common Knowledge Base. Vol III.
New York: Routledge Publishers; 2009: 43-59.
14. Ruldolph JW, Raemer DB, Simon R. Establishing a safe
container for learning in simulation: the role of the
presimulation briefing. Simul Healthc 2014;9:339-49. Crossref
15. Légaré F, Borduas F, Freitas A, et al. Development of a
simple 12-item theory-based instrument to assess the
impact of continuing professional development on clinical
behavioral intentions. PLoS One 2014;9:e91013. Crossref
16. Triandis HC. Values, attitudes, and interpersonal behaviour.
In: Howe HE Jr, Page MM, editors. Nebraska Symposium
on Motivation. Lincoln: University of Nebraska Press;
1979: 195-259.
17. Jamovi Project. Jamovi (desktop version 2.3.28 for Mac).
2024. Available from: https://dev.jamovi.org. Accessed 25 Oct 2024.
18. Clarke V, Braun V. Thematic analysis. In Teo T, editor.
Encyclopedia of Critical Psychology. New York: Springer;
2014: 1947-52. Crossref
19. ATLAS.ti Scientific Software Development GmbH.
ATLAS.ti (software version 8.4.5). 2024. Available from: https://atlasti.com. Accessed 25 Oct 2024.
20. Baboolal SO, Singaram VS. Specialist training: workplace-based
assessments impact on teaching, learning and
feedback to support competency-based postgraduate
programs. BMC Med Educ 2023;23:941. Crossref
21. Castanelli DJ, Weller JM, Molloy E, Bearman M. Trust,
power and learning in workplace-based assessment: the
trainee perspective. Med Educ 2022;56:280-91. Crossref
22. Gaunt A, Patel A, Rusius V, Royle TJ, Markham DH,
Pawlikowska T. ‘Playing the game’: how do surgical trainees
seek feedback using workplace-based assessment? Med
Educ 2017;51:953-62. Crossref
23. Knowles MS, Holton EF III, Swanson RA. The Adult
Learner: The Definitive Classic in Adult Education and
Human Resource Development, 6th ed. Amsterdam:
Elsevier; 2005.
24. Francom GM, Gardner J. What is task-centered learning?
TechTrends 2014;58:27-35. Crossref
25. van Merriënboer JJ, Kirschner PA. Ten Steps to Complex
Learning: A Systematic Approach to Four-Component
Instructional Design. 3rd ed. New York: Routledge
Publisher; 2018. Crossref
26. Lerchenfeldt S, Kamel-ElSayed S, Patino G, Loftus S,
Thomas DM. A qualitative analysis on the effectiveness
of peer feedback in team-based learning. Med Sci Educ
2023;33:893-902. Crossref
27. Man D, Kong B, Chau MH. Developing student feedback
literacy through peer review training. RELC J 2024;55:408-21. Crossref
28. Little T, Dawson P, Boud D, Tai J. Can students’ feedback
literacy be improved? A scoping review of interventions.
Assess Eval High Educ 2023;49:39-52. Crossref
29. van Merriënboer JJ, Sweller J. Cognitive load theory in
health professional education: design principles and
strategies. Med Educ 2010;44:85-93. Crossref
30. McLain M. Developing perspectives on ‘the demonstration’
as a signature pedagogy in design and technology
education. Int J Tech Design Educ 2021;31:3-26. Crossref
31. Grossman R, Salas E, Pavlas D, Rosen MA. Using
instructional features to enhance demonstration-based
training in management education. Acad Manag Learn
Educ 2012;12:219-43. Crossref