Hong Kong Med J 2026;32:Epub 30 Jan 2026
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Validation of diagnosis codes for pleural diseases
and procedure codes for relevant respiratory
procedures in a healthcare database in Hong
Kong: a single tertiary centre study
Ken KP Chan, MB, ChB, FRCP1,2; Timothy CC Ng, BSc1; CY Sze, BSc1; KC Ling, MPH1; Christopher Chan, MB, ChB, MRCP1; Charlotte HY Lau, MB, ChB, MRCP1; Stephanie WT Ho, MB, ChB, MRCP1; Joyce KC Ng, MB, ChB, FHKCP1; Rachel LP Lo, MB, ChB, FHKCP1; WH Yip, MB, ChB, FHKCP1; Jenny CL Ngai, MB, ChB, FRCP1; KW To, MB, ChB, FRCP1; Fanny WS Ko, MD, FRCP1; David SC Hui, MD, FRCP1
1 Department of Medicine and Therapeutics, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR, China
2 Li Ka Shing Institute of Health Sciences, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR, China
Corresponding author: Prof David SC Hui (dschui@cuhk.edu.hk)
Abstract
Introduction: There are insufficient population-based
epidemiological data on various pleural
diseases in Hong Kong. We aimed to validate ICD-9-CM (International Classification of Diseases,
Ninth Revision, Clinical Modification) codes for
pleural diseases and relevant procedures prior to
conducting epidemiological analyses using local
electronic health records.
Methods: Hospitalisation episodes coded as
‘pneumothorax’, ‘pleural effusion’, and trauma-related
pleural events, as well as procedures
beginning with ICD-9-CM codes 33 and 34 between
2013 and 2022, were retrieved from the Hospital
Authority. Paediatric patients and uninterrupted
hospitalisation episodes were excluded. The cohort
was filtered to include those hospitalised at Prince
of Wales Hospital (PWH). Up to 50 hospitalisation
episodes were randomly selected for manual
validation. Positive predictive values (PPVs) with
95% confidence intervals of individual codes were
calculated; successful validation was defined as a
PPV ≥0.700. The primary endpoint was the PPV of
individual diagnosis and procedure codes.
Results: A total of 26 757, 218 018, 1269, 185 154,
and 106 450 hospitalisation episodes with non-traumatic
pneumothorax, non-traumatic pleural
effusion, trauma-related pleural events, procedures
with code 33, and procedures with code 34,
respectively, were retrieved. Within the PWH
cohort, PPVs for these diagnosis and procedure
codes were 0.853 (0.787-0.904), 0.928 (0.903-0.948), 0.957 (0.907-0.981), 0.932 (0.913-0.948), and 0.933
(0.916-0.948), respectively. Procedures involving
indwelling pleural catheterisation and open drainage
of the pleural cavity failed validation due to frequent
miscoding.
Conclusion: This is the first validation study of
clinical codes for pleural diseases and related
procedures in Hong Kong. All diagnosis codes and
most procedure codes were successfully validated.
New knowledge added by this study
- This is the first validation study of clinical codes (International Classification of Diseases, Ninth Revision, Clinical Modification) for pleural diseases and relevant procedures in Hong Kong.
- All diagnosis codes and most procedure codes were successfully validated.
- Duplication of codes for similar diagnoses or procedures was identified.
- With the emergence of new respiratory procedures, diagnosis and procedure codes should be updated regularly.
- Removal or consolidation of duplicated subcodes in the Hospital Authority system is necessary to facilitate accurate future research and analysis using clinical codes.
- Researchers should be reminded to search all relevant diagnosis and procedure codes to minimise missing data when identifying specific diseases or procedures.
Introduction
Pleural diseases are common respiratory conditions
that often require hospital admission and have
shown an increasing incidence.1 2 In the United
States, approximately 1.5 million patients experience
pleural effusion annually, with most cases attributed
to congestive heart failure, pneumonia, and cancer.3 4
A recent multicentre, cross-sectional study in China
estimated the prevalence of pleural effusion at 4684
per 1 million Chinese adults.5 In that study, the most
common causes were parapneumonic effusion and
empyema (25.1%), malignant neoplasms (23.7%), and
tuberculosis (12.3%).5 The median hospitalisation
cost was ¥15 534.5 (interquartile range, 9447.2-29 000.0).5 Additionally, an increasing trend in
admissions for spontaneous pneumothorax has been
observed in England, highlighting the prevalence of
the disease and its associated healthcare burden.2
Management of pleural diseases involves
various diagnostic and therapeutic procedures that
extend beyond the pleural space to include the airway
and lung parenchyma. Whether closed or open, these
procedures substantially contribute to the overall
healthcare burden. However, information about
pleural diseases and related respiratory procedures
in Hong Kong remains limited, highlighting the need for contemporary, population-based epidemiological data.
The Hospital Authority, which provides
healthcare services to over 90% of Hong Kong’s
population, maintains extensive healthcare
databases. These include the Clinical Management
System (CMS) and the Clinical Data Analysis and
Reporting System (CDARS), which capture a wide
range of longitudinal clinical data. Examples include
hospital discharge records, diagnosis and procedure
codes for each hospitalisation episode, radiological
findings, and laboratory parameters, particularly
blood and pleural fluid analyses. This comprehensive
dataset provides valuable insights into the burden of
pleural diseases and accurately represents the local
population.
Before analysing diseases and procedures using
administrative data, it is essential to validate the
accuracy of diagnosis and procedure codes within
the healthcare database. These codes are typically
entered by attending physicians, interventionists, or
surgeons performing the procedures, which suggests
a high degree of reliability. However, no prior local
validation study has been conducted. Therefore,
we aimed to assess whether diagnosis codes for
pleural diseases and procedure codes for relevant
respiratory procedures are accurately recorded for
each hospitalisation episode within the Hospital
Authority systems.
Methods
This retrospective, observational validation study of
diagnosis and procedure codes utilised data from a
territory-wide healthcare database in Hong Kong.
Clinical data were obtained from CDARS, provided
by the Hospital Authority. Hospitalisation episodes
with the targeted diagnosis and procedure codes
between 1 January 2013 and 31 December 2022
were retrieved from the system. Each observation
represented a hospitalisation episode rather than
a unique patient, and no patient recruitment was
involved.
Diagnosis and procedure codes were defined
using the International Classification of Diseases,
Ninth Revision, Clinical Modification (ICD-9-CM).
The basic format of an ICD-9-CM code consists of
three to six digits. The Hospital Authority further
extends these codes with additional characters
after the decimal point to specify particular
diagnoses or procedures within an ICD-9-CM
code subgroup (‘subcodes’). These subcodes are
displayed in CDARS but are not typically accessible
to frontline CMS users. All hospitalisation episodes
in acute hospitals with a discharge diagnosis code
of pneumothorax (codes starting with 512), pleural
effusion (codes starting with 012, 197.2, 220.4, 510,
or 511), traumatic pneumothorax or haemothorax
(trauma-related pleural events, codes starting with 860), or procedure codes for relevant respiratory
procedures (codes starting with 33 or 34) were
retrieved, regardless of their position in the coding
list. Hospitalisation episodes for patients younger
than 18 years or from paediatric departments were
excluded from subsequent validation analyses.
Uninterrupted hospitalisation episodes following
the index episodes, including those in acute or
convalescent hospitals with the same diagnosis
code of interest, were also excluded, as these may
represent duplicate entries for the same clinical
event. The remaining hospitalisation episodes after
exclusions were grouped as the main cohort.
Manual verification of a proportion of the
retrieved diagnosis and procedure codes, down to
the subcode level, was conducted to ensure data
accuracy. The main cohort was first filtered to
include only hospitalisation episodes at the authors’
affiliated institution, Prince of Wales Hospital
(PWH), forming the PWH cohort. A maximum of
50 hospitalisation episodes for each diagnosis or
procedure code were randomly extracted from the
PWH cohort to estimate the true positive predictive
values (PPVs) within a 13% margin of error at a
95% confidence interval (95% CI). This precision
level was chosen pragmatically to balance statistical
rigour with the substantial manual effort required for
chart review in this validation study. Prince of Wales
Hospital is a tertiary care centre with a complex case
mix, encompassing a wide range of pleural diseases
and advanced respiratory procedures. Within the
PWH cohort, the types of pleural disease (pleural
effusion, pneumothorax, and trauma-related pleural
events) and their underlying aetiologies (eg, non-tuberculous
infection, tuberculosis, and malignancy)
were determined through retrospective review of
clinical notes, discharge summaries, radiological
findings, and blood and pleural fluid analysis
results using the CMS. Procedure codes were
verified by reviewing procedure records within the
corresponding hospitalisation episodes. All cases
were independently reviewed by two board-certified
respiratory physicians. Discrepancies were resolved
through joint case review until consensus was
reached. Coding accuracy was expressed as PPVs
with 95% CIs. The PPV was calculated by dividing the
number of true positives (ie, hospitalisation episodes
in the PWH cohort where diagnosis and procedure
codes were confirmed by manual verification) by the
total number of true positives and false positives (ie,
episodes where codes were rejected upon manual
review). The 95% CI was calculated using the exact
binomial method.
We hypothesised that the PPVs for the accuracy
of diagnosis and procedure codes would be equal to
or greater than 0.700, a commonly used threshold for
successful validation.6 7 8 The primary endpoint was
the determination of PPVs for the listed diagnosis and procedure codes. All statistical analyses were
performed using Python (version 3.12.6).
Results
A total of 26 757 non-traumatic pneumothorax,
218 018 non-traumatic pleural effusion, and 1269
trauma-related pleural events were retrieved from
CDARS between 2013 and 2022. Following the
exclusion of paediatric patients and uninterrupted
hospitalisation episodes, 20 888 non-traumatic
pneumothorax, 199 323 non-traumatic pleural
effusion, and 1127 trauma-related pleural events
remained in the main cohort. Of these, 2451 (11.7%),
24 938 (12.5%), and 251 (22.3%) diagnosis codes
for non-traumatic pneumothorax, non-traumatic
pleural effusion, and trauma-related pleural events,
respectively, were identified from PWH (Fig).
Additionally, 185 154 and 106 450 relevant respiratory
procedures with ICD-9-CM codes starting with 33
and 34, respectively, were retrieved. After exclusions,
181 770 and 101 336 procedure codes remained, of
which 16 078 (8.8%) and 17 299 (17.1%) procedure
codes, respectively, were identified from PWH (Fig).
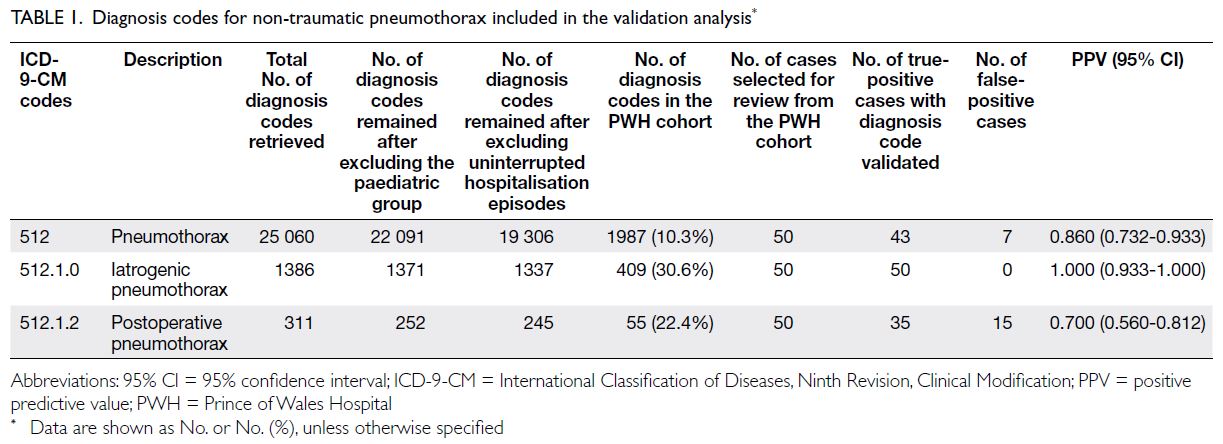
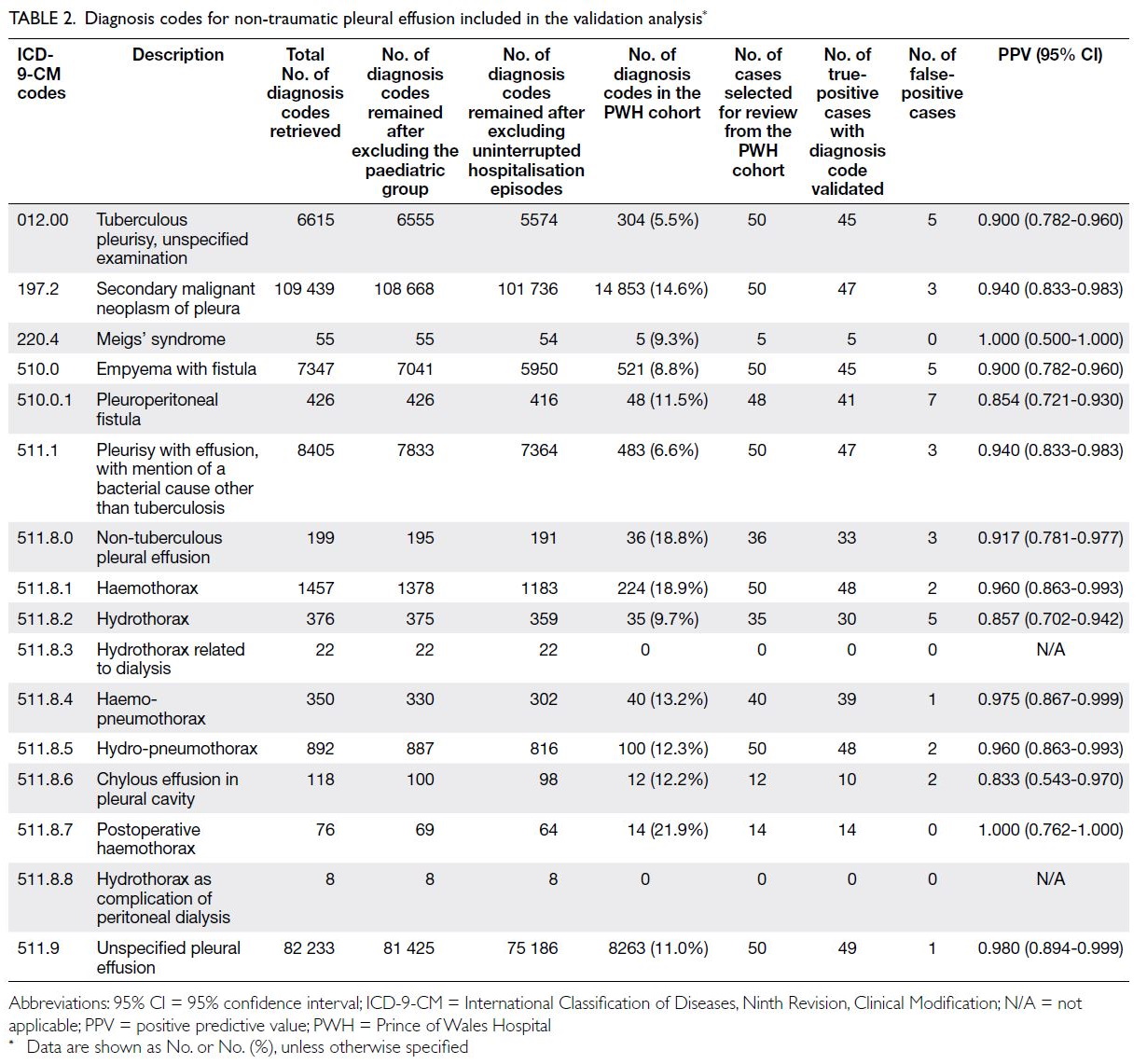
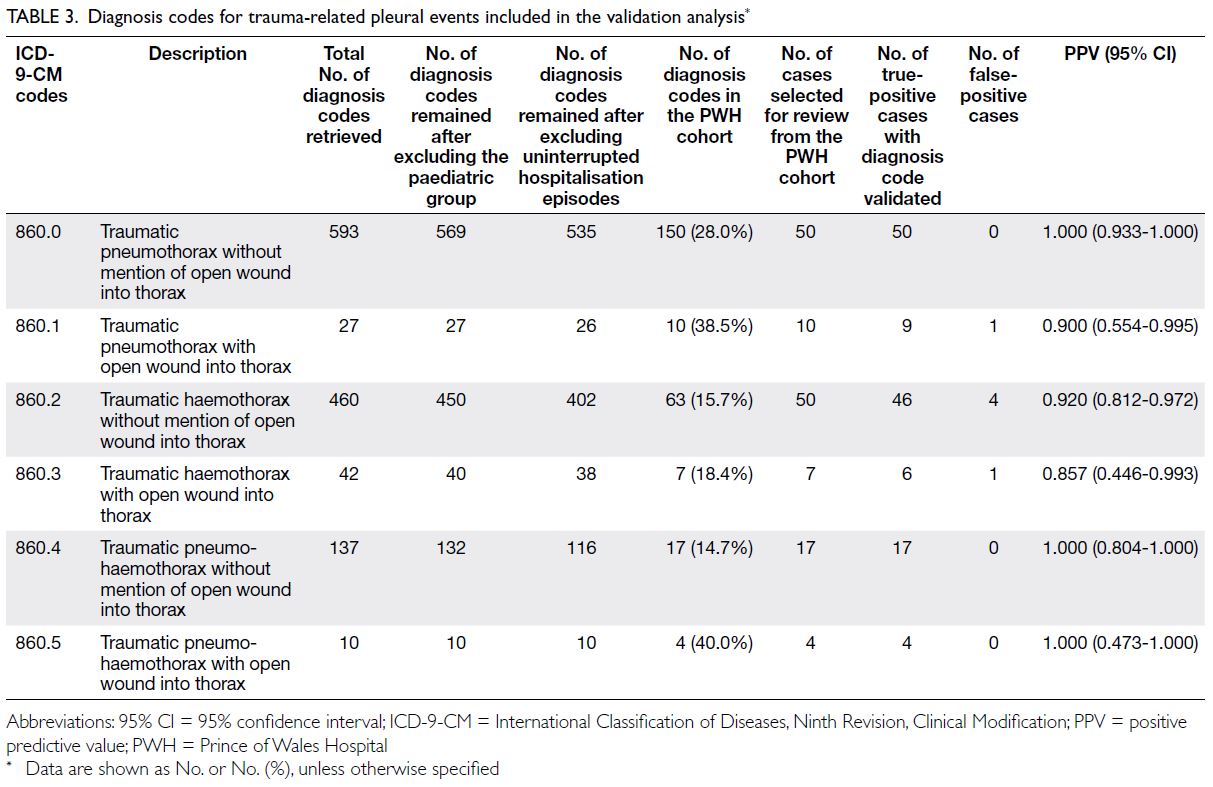
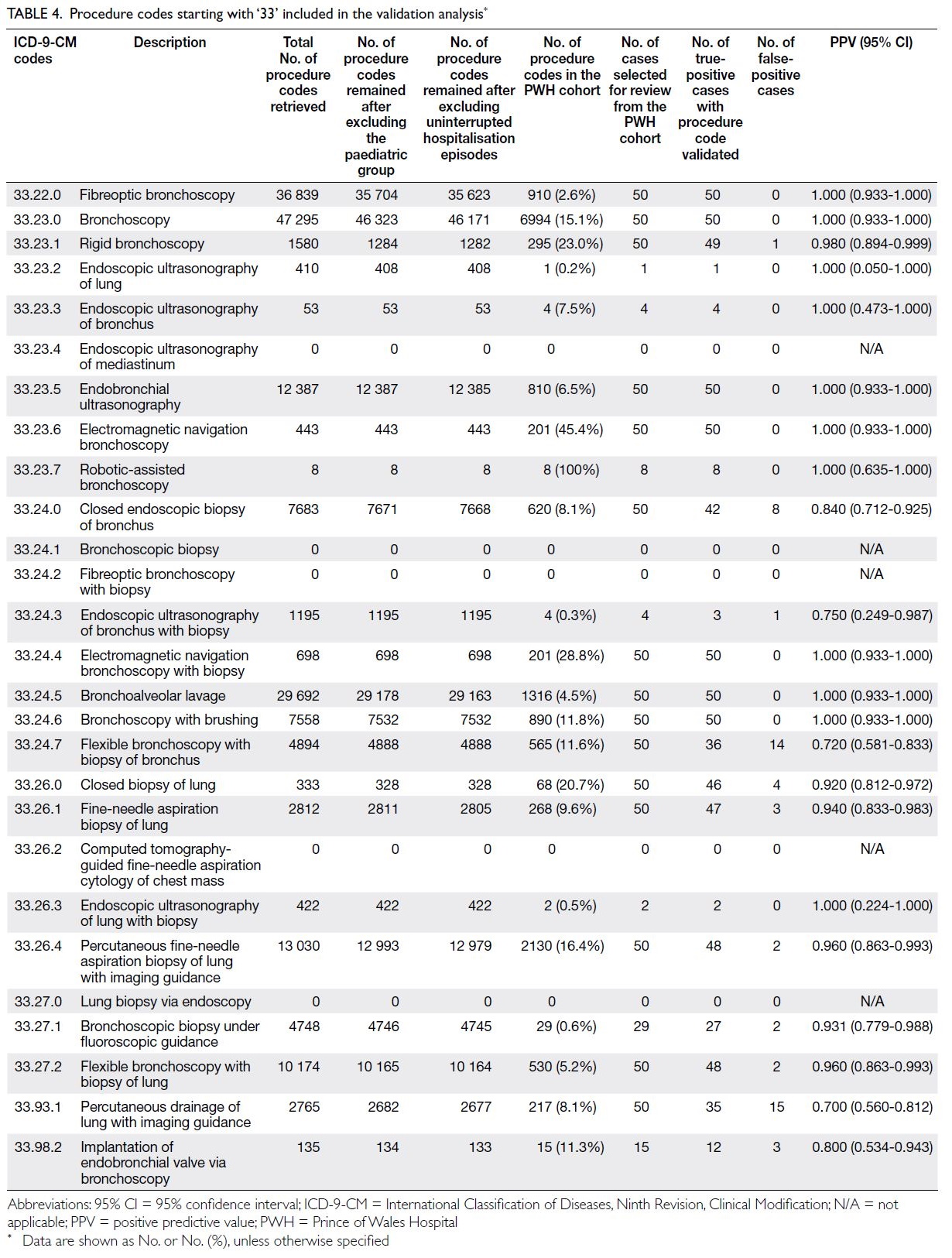
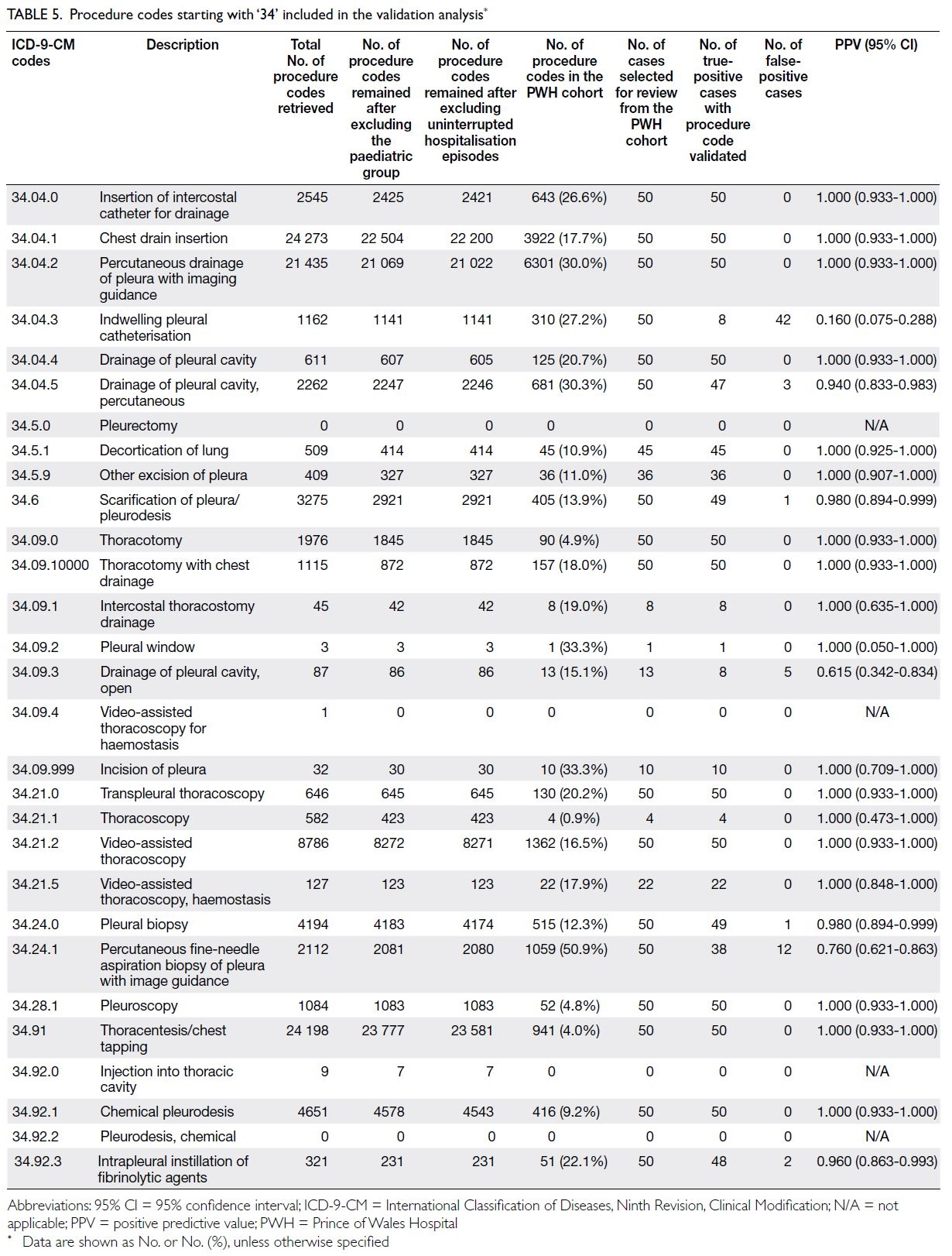
Tables 1, 2, and 3 list the diagnosis codes included in the
validation analysis for non-traumatic pneumothorax
(Table 1), non-traumatic pleural effusion (Table 2)
and trauma-related pleural events (Table 3), while
Tables 4 and 5 present the procedure codes starting
with ‘33’ and ‘34’, respectively; the breakdown of
hospitalisation episodes retrieved using these codes,
and the numbers remaining after screening, are also
shown.
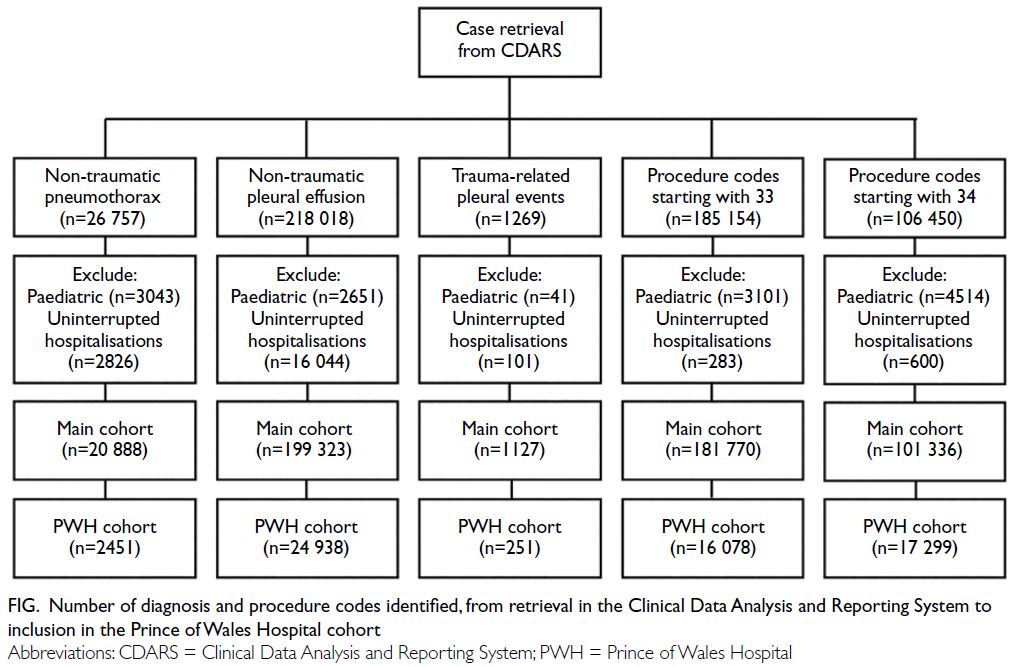
Figure. Number of diagnosis and procedure codes identified, from retrieval in the Clinical Data Analysis and Reporting System to inclusion in the Prince of Wales Hospital cohort
The overall PPVs (95% CIs) for pneumothorax,
pleural effusion, trauma-related pleural events, and
all diagnosis codes were 0.853 (0.787-0.904), 0.928
(0.903-0.948), 0.957 (0.907-0.981), and 0.919 (0.898-0.936), respectively. The overall PPVs (95% CIs)
for procedure codes starting with 33, starting with
34, and for all procedure codes were 0.932 (0.913-0.948), 0.933 (0.916-0.948), and 0.933 (0.920-0.944),
respectively.
The PPVs for diagnosis codes related to
pneumothorax, pleural effusion, and trauma-related
pleural events were all equal to or greater
than 0.700, with ranges of 0.700-1.000, 0.833-1.000,
and 0.857-1.000, respectively. The lowest PPV
(95% CI) was observed for postoperative
pneumothorax (procedure code 512.1.2) at 0.700
(0.560-0.812). The highest PPVs were seen for
iatrogenic pneumothorax (procedure code 512.1.0)
and postoperative haemothorax (procedure code
511.8.7), both at 1.000, with 95% CIs of 0.933-1.000
and 0.762-1.000, respectively. The reasons for false-positive
diagnosis codes are summarised in online supplementary Tables 1 to 3, with inappropriate
coding of alternative diseases being the most
common cause.
The PPVs for procedure codes starting with 33
ranged from 0.700 to 1.000. Procedure codes starting
with 34 met the PPV benchmark, except for 34.04.3
(indwelling pleural catheterisation) and 34.09.3
(drainage of the pleural cavity, open). The reasons
for false-positive procedure codes are listed in online supplementary Tables 4 and 5, with inappropriate
coding of alternative but similar procedures being
the most common cause. The low PPV for procedure code 34.04.3 (indwelling pleural catheterisation)
arose from its misuse to represent non-tunnelled
pleural catheter insertion, or to document the
presence of an indwelling pleural catheter (IPC)
inserted during prior hospitalisations. Procedure
code 34.09.3 (drainage of the pleural cavity, open)
failed to meet the PPV benchmark because it was
misused to represent closed pleural drainage by
drain insertion, rather than an open procedure.
Discussion
This study is the first to validate diagnosis and
procedure codes for pleural diseases using a
healthcare database in Hong Kong. All diagnosis
codes for pleural diseases and the majority of
procedure codes for relevant respiratory procedures
met the PPV benchmark of 0.700 or higher. Only
procedure codes 34.04.3 (indwelling pleural
catheterisation) and 34.09.3 (drainage of the pleural
cavity, open) failed to meet the validation criteria.
In 2008, the Hong Kong Thoracic Society
reported the burden of lung disease in Hong Kong
using local data from various governmental sources; however, pleural diseases were not included in the
report.9 Over the subsequent decade, the incidence
rates of individual pleural diseases were studied in
Hong Kong. However, these studies were limited
in scope as they focused on single pleural diseases
(eg, empyema,10 11 12 malignant mesothelioma,13 and
spontaneous pneumothorax14) or were restricted to single-centre settings.10 11
There is a pressing need for contemporary,
population-based epidemiological data covering
various pleural diseases in Hong Kong. A recent
local survey highlighted heterogeneous practices
in the management of pleural diseases among medical clinicians and reflected a lack of awareness
and dedicated service infrastructure for pleural
diseases.15 Given the rapid advancements in
diagnostic strategies and therapeutic options for
pleural diseases,16 an accurate and up-to-date
assessment of their clinical burden is crucial. Such
data provide a foundation for guiding future research,
benchmarking healthcare standards in Hong Kong
against those of other countries, informing the
allocation of future healthcare resources for pleural
diseases, and estimating the workload of healthcare
professionals managing these conditions. All such
service developments should be based on an accurate
estimation of the current burden and projected
future demand. The use of existing healthcare
databases offers a practical approach; however,
relevant diagnosis and procedure codes must first be
validated. A similar research pathway was followed
by Arnold et al,17 who validated diagnosis codes prior
to assessing the epidemiology of pleural empyema in
English hospitals.17 18
Nearly all PPVs of the diagnosis and
procedure codes studied exceeded the benchmark
of 0.700. Notably, PPVs for procedure codes were
generally higher than those for diagnosis codes.
This is because diagnosis codes can be carried over from previous hospitalisation episodes, enabling
attending physicians to select active or inactive
diagnosis codes regardless of their relevance
to the current episode. In contrast, procedure
codes cannot be carried over and must be entered
manually to reflect procedures performed during
the corresponding hospitalisation episode. This
requirement contributes to the higher accuracy for
procedure codes.
The PPV for procedure code 34.04.3 (indwelling
pleural catheterisation) was unexpectedly low due
to misuse. The absence of a specific diagnosis code
indicating the presence of an IPC, combined with the
inclusion of the term ‘pleural’ in the code description,
contributed to its incorrect use, particularly
during searches for non-tunnelled pleural catheter
insertion. Updated diagnosis codes to indicate the
status ‘presence of IPC’, or a new procedure code
for ‘pleural fluid drainage using an existing IPC’,
would accurately reflect the clinical scenario. Once
available, such codes should be validated before any
analyses of IPC use in territory-wide healthcare
databases. Alternatively, establishing a clinical
registry for IPC use could facilitate more accurate
tracking of patients with both malignant and benign
causes of pleural effusion.
Some diagnosis codes (eg, hydrothorax related
to dialysis [511.8.3] and hydrothorax as complication
of peritoneal dialysis [551.8.8]) and procedure codes
(eg, video-assisted thoracoscopy for haemostasis
[34.09.4] and injection into thoracic cavity [34.92.0])
were used in other hospitals but not at PWH;
therefore, they could not be validated in this study.
Within the PWH cohort, alternative diagnosis or
procedure codes were used and validated. However,
the number of hospitalisation episodes associated
with these codes was small, and their impact would
be minimal in a territory-wide healthcare data
analysis where similar codes are grouped together.
Duplication of subcodes for similar diagnoses
or procedures was also noted. Several diagnoses and
procedures were represented by different codes,
including:
Researchers should be reminded to search all
relevant diagnosis and procedure codes to minimise
the risk of missing data for specific diseases or
procedures during code searches. In the long term,
reconciling similar codes may help reduce ambiguity
and improve data consistency.
Strengths and limitations
This study has several strengths, notably its status
as the first validation study conducted using
a large healthcare database in Hong Kong. It
successfully validated codes for a wide range of
pleural diseases and respiratory procedures, thereby
laying the foundation for future epidemiological
research. However, several limitations should be
acknowledged. Not all codes could be adequately
validated due to their small case volumes in the PWH
cohort. For example, codes for Meigs’ syndrome
(220.4), traumatic pneumothorax with open wound
into thorax (860.1), and traumatic haemothorax with open wound into thorax (860.3) had small numbers
even in the overall cohort, and some codes were
duplicated. As such, future research incorporating
patient searches based on these diagnosis and
procedure codes should take these limitations
into account. The single-centre nature of the study
represents a further limitation, as disease patterns
and coding practices may vary across district general
hospitals.
Conclusion
This is the first validation study of diagnosis codes
for pleural diseases and procedure codes for
relevant respiratory procedures using a territory-wide
healthcare database in Hong Kong. All
diagnosis codes and the majority of procedure
codes demonstrated high PPVs, indicating accurate
coding. Given the emergence of new respiratory
procedures, diagnosis and procedure codes should
be regularly updated. The removal or consolidation
of duplicated subcodes within the Hospital Authority
system is also necessary to facilitate accurate future
research and analysis using clinical codes. Further
evaluation and harmonisation of coding practices
across different hospitals would be beneficial. These
measures will pave the way for future territory-wide
studies and enable monitoring of the overall burden
of pleural diseases in Hong Kong.
Author contributions
Concept or design: KKP Chan.
Acquisition of data: KKP Chan, TCC Ng, CY Sze, KC Ling.
Analysis or interpretation of data: KKP Chan, TCC Ng, CY Sze, KC Ling.
Drafting of the manuscript: KKP Chan.
Critical revision of the manuscript for important intellectual content: KKP Chan, TCC Ng, C Chan, CHY Lau, SWT Ho, JKC Ng, RLP Lo, WH Yip, JCL Ngai, KW To, FWS Ko, DSC Hui.
Acquisition of data: KKP Chan, TCC Ng, CY Sze, KC Ling.
Analysis or interpretation of data: KKP Chan, TCC Ng, CY Sze, KC Ling.
Drafting of the manuscript: KKP Chan.
Critical revision of the manuscript for important intellectual content: KKP Chan, TCC Ng, C Chan, CHY Lau, SWT Ho, JKC Ng, RLP Lo, WH Yip, JCL Ngai, KW To, FWS Ko, DSC Hui.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank Prof Terry CF Yip from the Department of Medicine and Therapeutics of The Chinese University of
Hong Kong for providing statistical support.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This research was approved by the Joint Chinese University of
Hong Kong–New Territories East Cluster Clinical Research Ethics Committee, Hong Kong (Ref No.: 2022.031). The
requirement for patient consent was waived by the Committee
due to the retrospective nature of the study.
Supplementary material
The supplementary material was provided by the authors and
some information may not have been peer reviewed. Accepted
supplementary material will be published as submitted by the
authors, without any editing or formatting. Any opinions or
recommendations discussed are solely those of the author(s)
and are not endorsed by the Hong Kong Academy of Medicine
and the Hong Kong Medical Association. The Hong Kong
Academy of Medicine and the Hong Kong Medical Association
disclaim all liability and responsibility arising from any reliance
placed on the content.
References
1. Bodtger U, Hallifax RJ. Epidemiology: why is pleural disease
becoming more common? In: Maskell NA, Laursen CB,
Lee YCG, et al, editors. Pleural Disease. Vol 87. Schweiz,
Switzerland: European Respiratory Society; 2020: 1-12. Crossref
2. Hallifax RJ, Goldacre R, Landray MJ, Rahman NM,
Goldacre MJ. Trends in the incidence and recurrence of
inpatient-treated spontaneous pneumothorax, 1968-2016.
JAMA 2018;320:1471-80. Crossref
3. Light RW. Pleural effusions. Med Clin North Am 2011;95:1055-70. Crossref
4. Taghizadeh N, Fortin M, Tremblay A. US hospitalizations
for malignant pleural effusions: data from the 2012
National Inpatient Sample. Chest 2017;151:845-54. Crossref
5. Tian P, Qiu R, Wang M, et al. Prevalence, causes, and health
care burden of pleural effusions among hospitalized adults
in China. JAMA Netw Open 2021;4:e2120306. Crossref
6. Kwok WC, Tam TC, Sing CW, Chan EW, Cheung CL.
Validation of diagnostic coding for bronchiectasis in
an electronic health record system in Hong Kong.
Pharmacoepidemiol Drug Saf 2023;32:1077-82. Crossref
7. Ye Y, Hubbard R, Li GH, et al. Validation of diagnostic coding for interstitial lung diseases in an electronic health
record system in Hong Kong. Pharmacoepidemiol Drug
Saf 2022;31:519-23. Crossref
8. Kwok WC, Tam TC, Sing CW, Chan EW, Cheung CL.
Validation of diagnostic coding for asthma in an electronic
health record system in Hong Kong. J Asthma Allergy
2023;16:315-21. Crossref
9. Chan-Yeung M, Lai CK, Chan KS, et al. The burden of
lung disease in Hong Kong: a report from the Hong Kong
Thoracic Society. Respirology 2008;13 Suppl 4:S133-65. Crossref
10. Chan KP, Ng SS, Ling KC, et al. Phenotyping empyema by
pleural fluid culture results and macroscopic appearance:
an 8-year retrospective study. ERJ Open Res 2023;9:00534-2022. Crossref
11. Tsang KY, Leung WS, Chan VL, Lin AW, Chu CM.
Complicated parapneumonic effusion and empyema
thoracis: microbiology and predictors of adverse outcomes.
Hong Kong Med J 2007;13:178-86.
12. Chan KP, Ma TF, Sridhar S, Lam DC, Ip MS, Ho PL. Changes
in etiology and clinical outcomes of pleural empyema
during the COVID-19 pandemic. Microorganisms
2023;11:303. Crossref
13. Chang KC, Leung CC, Tam CM, Yu WC, Hui DS, Lam WK.
Malignant mesothelioma in Hong Kong. Respir Med
2006;100:75-82. Crossref
14. Chan JW, Ko FW, Ng CK, et al. Management and prevention
of spontaneous pneumothorax using pleurodesis in Hong
Kong. Int J Tuberc Lung Dis 2011;15:385-90.
15. Lui MM, Yeung YC, Ngai JC, et al. Implementation of
evidence on management of pleural diseases: insights from
a territory-wide survey of clinicians in Hong Kong. BMC
Pulm Med 2022;22:386. Crossref
16. Lui MM, Lee YC. Twenty-five years of respirology:
advances in pleural disease. Respirology 2020;25:38-40. Crossref
17. Arnold DT, Hamilton FW, Morris TT, et al. Epidemiology
of pleural empyema in English hospitals and the impact of
influenza. Eur Respir J 2021;57:2003546. Crossref
18. Hamilton F, Arnold D. Accuracy of clinical coding of
pleural empyema: a validation study. J Eval Clin Pract
2020;26:79-80. Crossref