Hong Kong Med J 2023;29:Epub 7 Aug 2025
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PERSPECTIVE
A call for interdisciplinary bereavement care in
miscarriage and stillbirth: a stepped-care model approach
Celia HY Chan, PhD, MSW1,2,3; Sherman S Zhang, MSW2; Chris NL Ng, MSS2; Ernest HY Ng, FRCOG, FHKAM (Obstetrics and Gynaecology)3; Raymond HW Li, FRCOG, FHKAM (Obstetrics and Gynaecology)3; LM Yeung, MPH, BNur4; Kathy SF Wong, MPhil5
1 Department of Social Work, Melbourne School of Health Sciences, Faculty of Medicine, Dentistry and Health Sciences, The University of Melbourne, Melbourne, Australia
2 Department of Social Work and Social Administration, The University of Hong Kong, Hong Kong SAR, China
3 Department of Obstetrics and Gynaecology, The University of Hong Kong, Hong Kong SAR, China
4 Department of Obstetrics and Gynaecology, Queen Mary Hospital, Hong Kong SAR, China
5 Family Wellness Centre, Hong Kong Young Women’s Christian Association, Hong Kong SAR, China
Corresponding author: Prof Celia HY Chan (celia.chan@unimelb.edu.au)
Background
Bereavement following pregnancy loss, such as miscarriage or stillbirth, profoundly affects individuals
and families due to its sudden and traumatic nature.
The emotional toll can manifest as grief, depression,
anxiety, and post-traumatic stress disorder (PTSD),
often exacerbated by uncertainty and a lack of
preparedness. While healthcare primarily addresses
the medical and surgical aspects of management,
psychosocial support remains insufficient, leaving
many individuals and families feeling isolated.
Integrated perinatal bereavement care is needed
across hospital and community settings. This article
advocates for an interdisciplinary, stepped-care
model to provide tailored emotional, psychological,
and practical support. Embedding this framework
within healthcare systems can effectively address
the physical and psychosocial needs of bereaved
individuals and families, promoting healing and
overall well-being.
Definition and prevalence of miscarriage and
stillbirth
Miscarriage, defined as the spontaneous loss of
pregnancy before a specific gestational threshold,
affects 15% to 20% of pregnancies globally,1 with an
estimated 23 million cases annually, equating to 44
cases per minute.2 While the American College of
Obstetricians and Gynecologists and the European
Society of Human Reproduction and Embryology
classify early pregnancy loss as occurring within the
first 12 6/7 weeks of gestation,3 4 the World Health
Organization includes fetal weight criteria.5 In Hong
Kong, the Hospital Authority and the Hong Kong
SAR Government define miscarriage as pregnancy
loss before 24 weeks of gestation.6 According to
the Department of Health,7 nearly 10 000 cases of spontaneous abortion, medical abortion, and other
abortive outcomes were reported in 2023.
Stillbirth, defined as fetal death beyond a
certain gestational age, affects approximately 1.9
million pregnancies each year, occurring at a global
rate of 2.3 per 1000 births.8 The World Health
Organization defines stillbirth as fetal death at 28
weeks or later (or a weight of ≥1000 g if gestational
age is unknown), whereas the United States sets the
threshold at 20 weeks.9 In Hong Kong, stillbirth is
defined as fetal death at 24 weeks or later. A 20-year
retrospective study analysing 128 967 deliveries
between 2000 and 2019 recorded 429 stillbirths,
with the perinatal mortality rate declining by 16.7%,
from 5.52 per 1000 in 2000-2009 to 4.59 per 1000 in
2010-2019. The singleton stillbirth rate also slightly
decreased from 3.27 to 2.91 per 1000 births.10 These
reductions are attributed to advancements in early
prenatal screening and diagnosis of congenital and
genetic conditions.
Psychological impact and psychiatric
morbidity after pregnancy loss
Women who experience pregnancy loss are highly
susceptible to the onset of psychiatric morbidities,
including depression, anxiety, and PTSD.11 12 13 14
Depression is particularly prevalent, with a systematic
review reporting prevalence rates ranging from 5.4%
(minor depression as defined by the Diagnostic and
Statistical Manual of Mental Disorders [DSM], fourth
edition) to 18.6% (depressive disorders as defined by
the International Classification of Diseases, Tenth
Revision).13 For most women, depressive symptoms
peak in the initial months following pregnancy loss
and tend to decline over time. However, some women
may also experience significant anxiety symptoms,
including generalised anxiety and panic attacks, or develop PTSD, particularly when the pregnancy loss
is experienced as sudden, traumatic, or medically
complex. When compounded by profound grief,
these psychiatric responses can result in long-term
mental health challenges, including chronic
depression, suicidal ideation, and prolonged grief
disorder. Some women continue to experience these
symptoms even years after their loss.15
Grief following pregnancy loss is distinct and
often marginalised, lacking public acknowledgement
or support. This is particularly evident in cultures
such as Chinese society, where early-stage
pregnancies are commonly concealed.16 Such cultural
taboos can lead to isolated mourning, hindering
emotional expression and processing of grief. This
disenfranchisement intensifies the psychological
burden, highlighting the need for specialised mental
health interventions tailored to women coping
with pregnancy loss.17 Some individuals may even
develop prolonged grief reactions or persistent
complex bereavement disorder.15 These conditions
are characterised by intense and prolonged grief
symptoms, impairments in daily functioning, and
difficulties adapting to the loss, further complicating
the emotional distress experienced by bereaved
parents.
Clinical practice guidelines on management
of pregnancy loss in various countries
Recent advances in bereavement care for pregnancy
loss emphasise the integration of counselling
and psychotherapy to address emotional needs.
Guidelines from leading organisations such as the
National Institute for Health and Care Excellence
(United Kingdom)18 and The Royal Australian
and New Zealand College of Obstetricians and
Gynaecologists (Australia)19 advocate for counselling,
stigma reduction, respectful maternity care, and
planning for future pregnancy. The RESPECT Study
(Randomised Evaluation of Sexual health Promotion
Effectiveness informing Care and Treatment)
reinforces the global consensus on bereavement
care.20 Prioritising counselling and psychotherapy
as integral components of bereavement care enables
healthcare providers to offer tailored support to
bereaved individuals.
Perinatal bereavement care: the Hong Kong
context
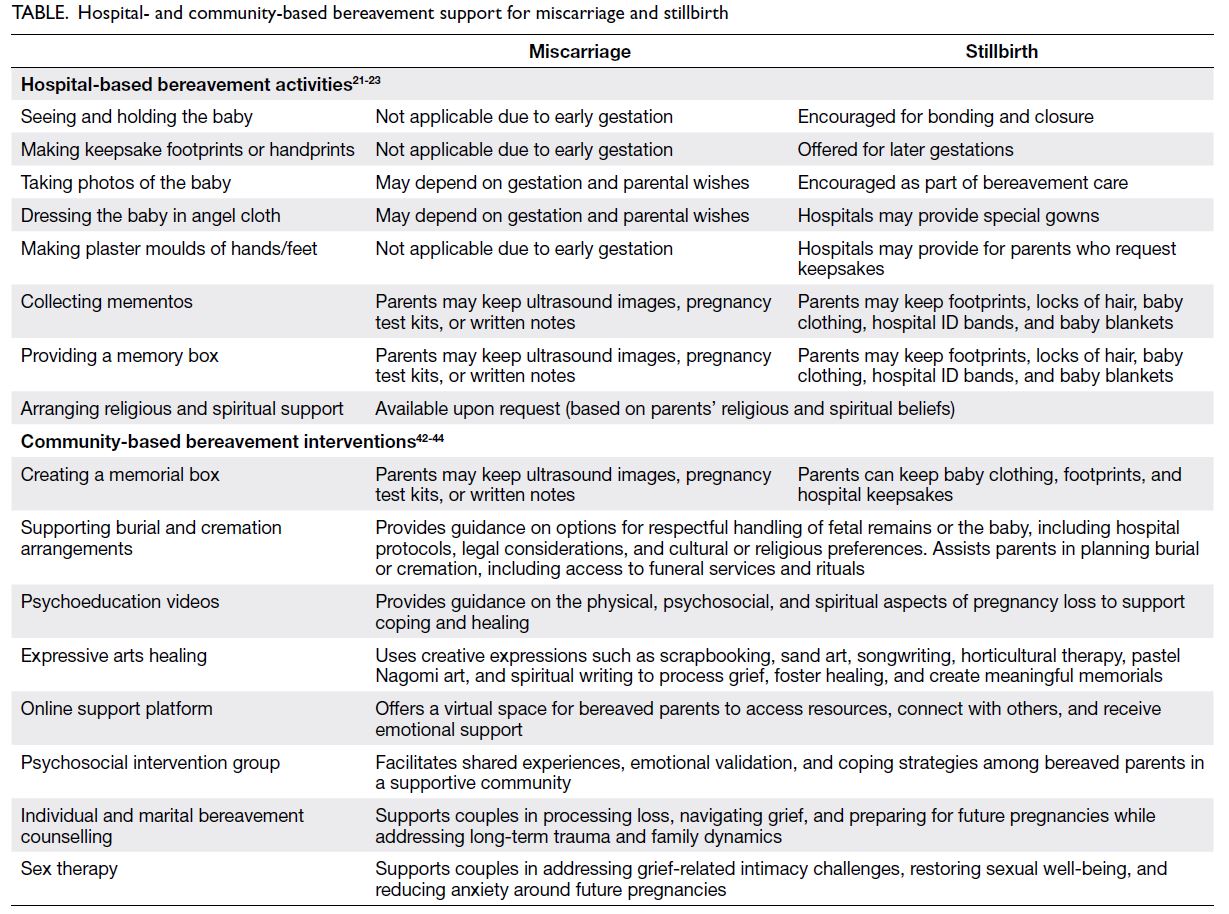
Perinatal bereavement care offers emotional,
psychological, and practical support to help families
cope with grief following miscarriage, stillbirth,
or neonatal death. Timely support is crucial
for parents coping with pregnancy loss. While
medical care primarily addresses complications
and interventions such as medication or surgery,
healthcare professionals can also play a role in
facilitating meaningful memorial experiences, such as seeing and holding the baby, creating keepsakes,
or capturing memories through photography. These
practices help parents process grief and create lasting
remembrances. Additional perinatal mourning
resources are detailed in the Table.21 22 23
The Hong Kong SAR Government has made
substantial progress in improving fetal burial and
cremation services. Previously, fetuses miscarried
before 24 weeks of gestation were classified as
medical waste, limiting options for grieving parents.
In 2017, the Government amended relevant
regulations to permit cremation for these fetuses,
and six private cemeteries now offer services for
storing the remains.24 The Hospital Authority
has also updated its guidelines to promote the
compassionate handling of fetal remains; however,
legal and logistical challenges remain.
However, ongoing bereavement support often
diminishes following hospital discharge, leaving
parents feeling isolated and uncertain about how to
seek emotional support or counselling. Integrating
comprehensive bereavement care is essential to
ensure continuous access to emotional support,
counselling, and resources for navigating long-term
grief.
A call for a stepped-care model in perinatal
bereavement care
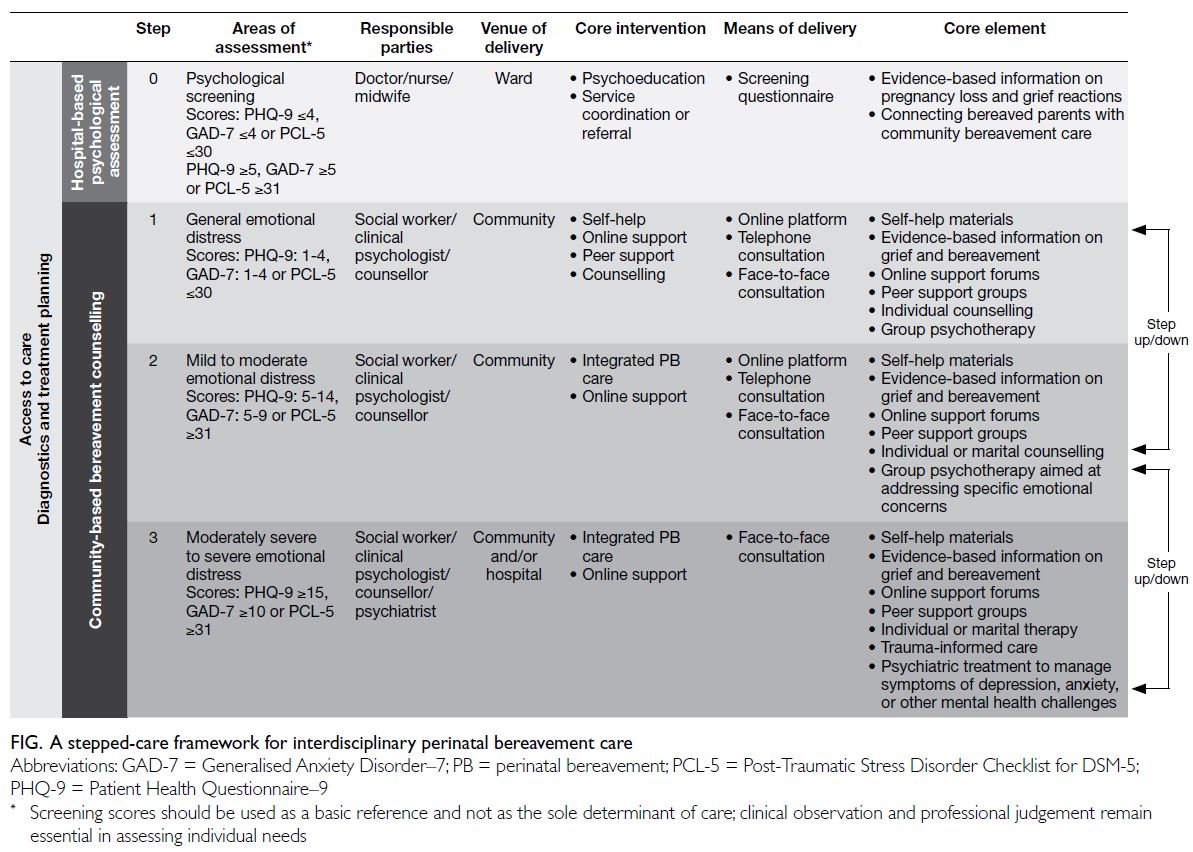
In recent years, stepped-care models have been
widely adopted across global and local public health
and mental health systems due to their tiered
approach to care delivery, which has demonstrated
positive outcomes and helped alleviate healthcare
burdens.25 26 27 28 Newman proposed a cost-effective
method for identifying at-risk individuals and
delivering stepped interventions based on
standardised psychometric assessments.29 This
model begins with less intrusive, lower-cost options
and escalates care as needed for individuals with
greater mental health needs. Stepped care also
accommodates a spectrum of interventions, from
low-intensity self-help to specialised high-intensity
therapies, ensuring timely and appropriate care.30
Perinatal bereavement care supports parents
through the complexities of loss by providing clear,
empathetic information about its causes, physical
recovery, and emotional responses. Sensitive
communication is crucial for addressing parents’
emotional needs during this distressing time. A
systematic review and meta-analysis found that
stepped-care interventions were significantly more
effective than usual care in reducing depression.31
Incorporating a stepped-care model into
bereavement support offers a structured framework,
with varying levels of intervention tailored to the
degree of psychosocial distress among bereaved
parents. Comprehensive screening facilitates
assessment of distress severity, guiding parents towards the most appropriate level of support. This
model fosters emotional healing and resilience,
ensuring that bereaved parents receive the right care
at the right time.
Step 0: Hospital-based psychological
screening and follow-up
The provision of follow-up care through detailed
information about the causes of loss, associated
symptoms, recovery, and future pregnancy
prospects empowers individuals to prioritise their
health, make informed decisions, and navigate their
grief. Discussions with bereaved parents should
address the risks and benefits of future pregnancies,
considering their physical and emotional readiness
along with medical causes. This dialogue should
also include available support services, such as
preconception counselling and specialised high-risk
pregnancy care.
Standardised psychological screening
enables consistent assessment, effective triage, and
appropriate referrals. A scoping review identified 93 studies involving 6248 women who had terminated
pregnancies due to fetal anomalies, with the most
commonly used psychological tools being the
Perinatal Grief Scale (22%) and the Impact of Event
Scale–Revised (18%).32 Additional measures, such
as the Hospital Anxiety and Depression Scale,33
the Patient Health Questionnaire–9 (PHQ-9),21
the Generalised Anxiety Disorder–7 (GAD-7),22
and the Post-Traumatic Stress Disorder Checklist
for DSM-5 (PCL-5),23 have been utilised to assess
emotional distress, anxiety, depression, and trauma-related
symptoms. In Hong Kong, the 12-item
General Health Questionnaire combined with the
Structured Clinical Interview for DSM-IV Axis I
Disorders identified psychiatric morbidity following
miscarriage.14 34
Although grief is a natural emotional response
to pregnancy loss, depression, generalised anxiety,
and post-traumatic stress are clinically actionable
screening parameters due to their prevalence,
impact, and established treatment pathways.35
Unlike grief which can vary in duration and intensity, conditions such as depression, anxiety, and PTSD
may become pathological, substantially impairing
daily functioning, increasing the risk of suicidal
ideation, and influencing future reproductive
decision making.
Given time constraints, clinician workload and
resource limitations, comprehensive psychological
assessments may be impractical. A brief yet reliable
screening tool is therefore more feasible for early
identification and intervention. The PHQ-9, GAD-7,
and PCL-5 have been validated and utilised across
diverse and general populations and offer a practical
approach to mental health screening.36 37 38 39 40 41 The
abovementioned Step 0 is conducted using these
tools to assess depressive symptoms, generalised
anxiety, and post-traumatic stress. Individuals with
minimal distress (scores: PHQ-9 ≤4, GAD-7 ≤4, and
PCL-5 ≤30) may not require immediate intervention,
whereas those with elevated distress (scores: PHQ-9
≥5, GAD-7 ≥5, or PCL-5 ≥31) should receive further
psychological support and appropriate referrals.
This structured screening process facilitates early
identification of individuals in need of additional psychosocial support. The Figure illustrates the
stepped-care framework, integrating psychological
assessment into medical treatment to ensure that
bereaved parents receive services tailored to their
needs.
Steps 1 to 3: Community-based psychosocial
support
Grief and emotional distress following pregnancy loss
can vary, necessitating tailored support. Accessible,
community-based care ensures that bereaved
parents receive appropriate psychosocial assistance.
Beyond medical and psychological interventions,
connecting bereaved parents with non-governmental
organisations and community resources is essential.
These organisations provide guidance on burial
or cremation arrangements, funeral services, and
bereavement support, helping families to navigate
their grief beyond the hospital setting (Table42 43 44). A
stepped-care model based on PHQ-9, GAD-7, and
PCL-5 scores enables structured intervention at
varying levels of emotional distress, ensuring that
individuals receive care aligned with their needs.
Step 1: General emotional distress
For individuals experiencing general emotional
distress (scores: PHQ-9: 1-4, GAD-7: 1-4, or PCL-5
≤30), low-intensity support is recommended.
Although clinical intervention may not be necessary,
emotional validation, short-term counselling, online
forums, self-help materials, and peer support can
offer reassurance. Psychoeducational workshops on
grief and coping may also be helpful. A brief follow-up
via telephone or through primary care helps
ensure timely support if distress increases.
Step 2: Mild to moderate emotional distress
For individuals experiencing mild to moderate
emotional distress (scores: PHQ-9: 5-14, GAD-7:
5-9, or PCL-5 ≥31), structured psychosocial care
is beneficial. Support may include individual or
group therapy, bereavement counselling, expressive
activities, and self-help tools such as journaling,
art therapy, and mindfulness. Online mental health
resources with guided self-help tools can also be
valuable. Periodic reassessment ensures ongoing
care and timely referrals if distress escalates, enabling
appropriate intervention based on evolving needs.
Step 3: Moderately severe to severe emotional
distress
For individuals experiencing moderate to severe
emotional distress (scores: PHQ-9: ≥15, GAD-7:
≥10, or PCL-5 ≥31), a multidisciplinary approach
is required. Psychological symptoms at this severity
may impair daily functioning, strain relationships, or
affect decision making regarding future pregnancies.
Support may include individual therapy, trauma-informed
care, family counselling, and psychiatric
evaluation. Immediate intervention is crucial for
those at risk of prolonged grief disorder, severe
depression, or suicidal ideation. Close monitoring
and coordinated care among hospital-based
professionals, community grief services, and
primary care providers help ensure continuity and
timely support.
Capacity building for healthcare
professionals
Enhancing healthcare professionals’ capacity for
perinatal bereavement care requires structured
strategies. Key approaches include developing
patient-centred bereavement care plans, training
staff in grief support, and establishing dedicated
teams. The integration of psychosocial assessments,
mental health referrals, and staff support fosters
compassionate care. Sensitivity, empathy, and
ongoing training improve service quality. Strategies
to provide follow-up care, referrals, and clear
information empower families in decision making.
By recognising the long-term impact of grief, sustained support can ensure continuity of care,
thereby strengthening bereavement services within
Hong Kong’s healthcare system.
Conclusion
Ensuring continuity of care is essential in supporting
families affected by pregnancy loss. Integrated
bereavement care, delivered with empathy,
acknowledges the profound impact on bereaved
parents. A holistic approach addressing diverse
emotional and practical needs is vital, supported by
a structured care model grounded in evidence-based
practices. Collaborations among medical doctors,
psychiatrists, midwives, clinical psychologists, social
workers, and counsellors are key, encompassing
counselling and access to resources such as support
groups. Prioritising continuity and interdisciplinary
teamwork fosters healing and recovery from the
profound grief of pregnancy loss.
Author contributions
Concept or design: CHY Chan.
Acquisition of data: CHY Chan, SS Zhang, CNL Ng.
Drafting of the manuscript: CHY Chan, SS Zhang.
Critical revision of the manuscript for important intellectual content: CHY Chan, CNL Ng, EHY Ng, RHW Li, LM Yeung, KSF Wong.
Acquisition of data: CHY Chan, SS Zhang, CNL Ng.
Drafting of the manuscript: CHY Chan, SS Zhang.
Critical revision of the manuscript for important intellectual content: CHY Chan, CNL Ng, EHY Ng, RHW Li, LM Yeung, KSF Wong.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
The stepped-care model used in this study was developed
under the Jockey Club Perinatal Bereavement Care Project,
a community-based initiative supported by the Hong Kong
Jockey Club Charities Trust (Ref No.: 2021-0395). The funder
had no role in the study design, data collection/analysis/interpretation, or manuscript preparation.
References
1. Tong F, Wang Y, Gao Q, et al. The epidemiology of
pregnancy loss: global burden, variable risk factors, and
predictions. Hum Reprod 2024;39:834-48. Crossref
2. Quenby S, Gallos ID, Dhillon-Smith RK, et al. Miscarriage
matters: the epidemiological, physical, psychological,
and economic costs of early pregnancy loss. Lancet
2021;397:1658-67. Crossref
3. American College of Obstetricians and Gynecologists’
Committee on Practice Bulletins—Gynecology. ACOG
Practice Bulletin No. 200: early pregnancy loss. Obstet
Gynecol 2018;132:e197-207. Crossref
4. Kolte AM, Bernardi LA, Christiansen OB, et al. Terminology
for pregnancy loss prior to viability: a consensus statement
from the ESHRE early pregnancy special interest group.
Hum Reprod 2015;30:495-8. Crossref
5. World Health Organization. Definitions and Indicators in Family Planning Maternal & Child Health and
Reproductive Health used in the WHO Regional Office for
Europe. Copenhagen: WHO Regional Office for Europe;
2000.
6. Hong Kong SAR Government. Employment Ordinance (Cap 57). Available from: https://www.elegislation.gov.hk/hk/cap57!en?INDEX_CS=N. Accessed 12 Jul 2025.
7. Department of Health, Hong Kong SAR Government.
Tables on health status and health services 2023. Available
from: https://www.dh.gov.hk/english/pub_rec/pub_rec_ar/pdf/2324/supplementary_table2023.pdf . Accessed 12 Jul 2024.
8. World Health Organization. Stillbirth rate (per 1000 total
births): latest data. Available from: https://platform.who.int/data/maternal-newborn-child-adolescent-ageing/indicator-explorer-new/MCA/stillbirth-rate-(per-1000-total-births). Accessed 12 Jul 2025.
9. Smith LK, Morisaki N, Morken NH, et al. An international
comparison of death classification at 22 to 25 weeks’
gestational age. Pediatrics 2018;142:e20173324. Crossref
10. Wong ST, Tse WT, Lau SL, Sahota DS, Leung TY. Stillbirth
rate in singleton pregnancies: a 20-year retrospective study
from a public obstetric unit in Hong Kong. Hong Kong
Med J 2022;28:285-93. Crossref
11. Farren J, Jalmbrant M, Ameye L, et al. Post-traumatic
stress, anxiety and depression following miscarriage or
ectopic pregnancy: a prospective cohort study. BMJ Open
2016;6:e011864. Crossref
12. Xiao M, Huang S, Hu Y, Zhang L, Tang G, Lei J. Prevalence
of postpartum post-traumatic stress disorder and its
determinants in Mainland China: a systematic review and
meta-analysis. Arch Psychiatr Nurs 2023;44:76-85. Crossref
13. Mergl R, Quaatz SM, Lemke V, Allgaier AK. Prevalence
of depression and depressive symptoms in women with
previous miscarriages or stillbirths—a systematic review.
J Psychiatr Res 2024;169:84-96. Crossref
14. Sham AK, Yiu MG, Ho WY. Psychiatric morbidity
following miscarriage in Hong Kong. Gen Hosp Psychiatry
2010;32:284-93. Crossref
15. Bodunde EO, Buckley D, O’Neill E, et al. Pregnancy and
birth complications and long-term maternal mental health
outcomes: a systematic review and meta-analysis. BJOG
2025;132:131-42. Crossref
16. Sun JC, Rei W, Chang MY, Sheu SJ. Care and management
of stillborn babies from the parents’ perspective: a
phenomenological study. J Clin Nurs 2022;31:860-8. Crossref
17. Shaohua L, Shorey S. Psychosocial interventions on
psychological outcomes of parents with perinatal loss:
a systematic review and meta-analysis. Int J Nurs Stud
2021;117:103871. Crossref
18. National Institute for Health and Care Excellence.
Ectopic pregnancy and miscarriage: diagnosis and initial
management. 2019. Available from: https://www.nice.org.uk/guidance/ng126. Accessed 12 Jul 2025.
19. Australian Pregnancy Care Guidelines. Australian Living
Evidence Collaboration; 2025.
20. Shakespeare C, Merriel A, Bakhbakhi D, et al. The
RESPECT Study for consensus on global bereavement care
after stillbirth. Int J Gynecol Obstet 2020;149:137-47. Crossref
21. Kroenke K, Spitzer RL, Williams JBW. Patient Health
Questionnaire–9 (PHQ-9) [database record]. American
Psychological Association PsycTests; 1999. Crossref
22. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092-7. Crossref
23. Weathers FW, Litz BT, Palmieri PA, Keane TM, Marx BP,
Schnurr PP. PTSD Checklist for DSM-5 (PCL-5). United
States: National Center for PTSD; 2013.
24. Health Bureau, Hong Kong SAR Government.
LCQ16: Handling of abortuses [press release]. 28 June
2017. Available from: https://www.info.gov.hk/gia/general/201706/28/P2017062800450.htm. Accessed 12 Jul 2025.
25. Wang Y, Hu M, Zhu D, Ding R, He P. Effectiveness of
collaborative care for depression and HbA1c in patients
with depression and diabetes: a systematic review and
meta-analysis. Int J Integr Care 2022;22:12. Crossref
26. Bower P, Gilbody S, Richards D, Fletcher J, Sutton A.
Collaborative care for depression in primary care. Making
sense of a complex intervention: systematic review and
meta-regression. Br J Psychiatry 2006;189:484-93. Crossref
27. Lee WK, Lo A, Chong G, et al. New service model for
common mental disorders in Hong Kong: a retrospective
outcome study. East Asian Arch Psychiatry 2019;29:75-80. Crossref
28. Tang A, Liang HJ, Ungvari GS, Tang WK. Screening for
psychiatric morbidity in the postpartum period: clinical
presentation and outcome at one-year follow-up. J
Womens Health Care 2014;3:147. Crossref
29. Newman MG. Recommendations for a cost-offset model
of psychotherapy allocation using generalized anxiety
disorder as an example. J Consult Clin Psychol 2000;68:549-55. Crossref
30. National Institute for Health and Care Excellence.
Depression in adults: treatment and management.
Available from: https://www.nice.org.uk/guidance/ng222. Accessed 12 Jul 2025.
31. van Straten A, Hill J, Richards DA, Cuijpers P. Stepped care
treatment delivery for depression: a systematic review and
meta-analysis. Psychol Med 2015;45:231-46. Crossref
32. Slade L, Obst K, Deussen A, Dodd J. The tools used to assess
psychological symptoms in women and their partners after
termination of pregnancy for fetal anomaly: a scoping
review. Eur J Obstet Gynecol Reprod Biol 2023:288:44-8. Crossref
33. Zigmond AS, Snaith RP. The Hospital Anxiety and
Depression Scale. Acta Psychiatr Scand 1983;67:361-70. Crossref
34. Lok IH, Lee DT, Yip SK, Shek D, Tam WH, Chung TK.
Screening for post-miscarriage psychiatric morbidity. Am
J Obstet Gynecol 2004;191:546-50. Crossref
35. Farren J, Jalmbrant M, Ameye L, et al. Post-traumatic
stress, anxiety and depression following miscarriage or
ectopic pregnancy: a prospective cohort study. BMJ Open
2016;6:e011864. Crossref
36. Levis B, Benedetti A, Thombs BD; DEPRESsion Screening
Data (DEPRESSD) Collaboration. Accuracy of Patient
Health Questionnaire–9 (PHQ-9) for screening to detect
major depression: individual participant data meta-analysis.
BMJ 2019;365:l1476. Crossref
37. Kroenke K. PHQ-9: global uptake of a depression scale.
World Psychiatry 2021;20:135-6. Crossref
38. Saunders R, Moinian D, Stott J, et al. Measurement
invariance of the PHQ-9 and GAD-7 across males and
females seeking treatment for common mental health
disorders. BMC Psychiatry 2023;23:298. Crossref
39. Kroenke K, Spitzer RL, Williams JB, Löwe B. The Patient
Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry
2010;32:345-59. Crossref
40. Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL.
The Posttraumatic Stress Disorder Checklist for DSM-5
(PCL-5): development and initial psychometric evaluation.
J Trauma Stress 2015;28:489-98. Crossref
41. Horesh D, Nukrian M, Bialik Y. To lose an unborn child:
post-traumatic stress disorder and major depressive
disorder following pregnancy loss among Israeli women.
Gen Hosp Psychiatry 2018;53:95-100. Crossref
42. Caritas Family Service. Jockey Club Perinatal Bereavement
Care Project Grace Port–Caritas Miscarriage Support Centre. 2025. Available from: https://family.caritas.org.hk/. Accessed 17 Feb 2025.
43. Department of Social Work and Social Administration,
The University of Hong Kong. Jockey Club Perinatal
Bereavement Care Project Department of Social Work and
Social Administration, The University of Hong Kong. 2025.
Available from: https://www.jcperinatal-bc.hk/. Accessed 17 Feb 2025.
44. Hong Kong Young Women’s Christian Association. Jockey
Club Perinatal Bereavement Care Project Hong Kong
Young Women’s Christian Association. 2025. Available
from: https://fwcyyc.ywca.org.hk. Accessed 17 Feb 2025.