Hong Kong Med J 2025;31:Epub 31 Jul 2025
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Updated recommendations on knee osteoarthritis management: The Hong Kong College of Orthopaedic Surgeons position statement
WP Yau, FHKCOS, FRCSEd (Orth)
Department of Orthopaedics and Traumatology, Queen Mary Hospital and The University of Hong Kong, Hong Kong SAR, China
Corresponding author: Prof WP Yau (peterwpy@gmail.com)
Abstract
Introduction: To inform the public and medical
practitioners about the effectiveness of various
management regimens for knee osteoarthritis
(knee OA), the Hong Kong College of Orthopaedic
Surgeons (HKCOS) published a position statement
in 2022. This study aimed to present the findings from
expert consensus surveys conducted in 2022 and
2024, which form the basis of the recommendations
in the position statement.
Methods: Fellows of the HKCOS, who were listed
in the Specialist Register (Orthopaedics and
Traumatology) of the Hong Kong Medical Council,
were invited via email to participate in online surveys
in 2022 and 2024. The surveys collected opinions
on 26 interventions for the treatment of knee OA.
Expert panellists were instructed to provide their
recommendation for each intervention using one of
three options: ‘Recommend’, ‘Do not recommend’
or ‘Abstain’. A consensus of opinion was defined as
a minimum of 70% agreement among the expert
panellists.
Results: A total of 106 expert panellists participated
in the 2022 survey, and 28 participated in the 2024
survey. Consensus was reached among the expert
panellists for 14 interventions in 2022 and 13
interventions in 2024. In both surveys, the expert panel reached consensus in recommending the
following treatments for knee OA: patient education,
land-based exercise, water-based exercise, selfmanagement
programme, weight reduction, use
of a cane, oral paracetamol, topical non-steroidal
anti-inflammatory drugs, oral non-steroidal antiinflammatory
drugs, high tibial osteotomy, and joint
replacement surgery. Conversely, the expert panel
reached consensus in recommending against the use
of lateral wedge insoles and denervation therapy.
Conclusion: Findings from both the 2022 and 2024
surveys demonstrated consistent expert consensus
on key recommended and non-recommended
interventions for knee OA. The recommendations
provide evidence-based guidance to the public and
medical practitioners regarding the effectiveness of
various management strategies for knee OA.
New knowledge added by this study
- The Hong Kong College of Orthopaedic Surgeons (HKCOS) published a position statement on the management of knee osteoarthritis (knee OA).
- Two consecutive surveys conducted in 2022 and 2024 demonstrated consistent expert opinions among orthopaedic specialists in Hong Kong regarding the recommended management for knee OA.
- The results of these cross-sectional surveys and the recommendations made in the HKCOS position statement on the management of knee OA provide evidence-based guidance to the public and medical practitioners on the effectiveness of different management regimens for knee OA.
Introduction
The Hong Kong College of Orthopaedic Surgeons
(HKCOS) is the official professional body responsible
for organising the training of orthopaedic surgeons
and conducting specialist examinations in
orthopaedics in Hong Kong. The College also plays
a key role in setting standards of care in orthopaedic
surgery, which includes, but is not limited to, the
investigation, preservation, and restoration of the form and function of the extremities, spine, and
associated structures. The aim is to bring relief to
patients of all ages affected by injury or disease of
the musculoskeletal system.1
Knee osteoarthritis (knee OA) is common
among middle-aged and older individuals. Its
incidence and severity increase with age.2 Hong
Kong, one of the cities with the highest life
expectancy globally,3 faces a growing demand for knee OA treatment.4 In the public healthcare sector,
patients often experience a long waiting time for
medical consultation, physiotherapy, and surgical
interventions related to knee OA.4 With an ageing
population, the number of individuals affected by
knee OA is expected to further increase over the
next two to three decades,5 highlighting the urgent
need for effective management strategies in Hong
Kong.
To provide evidence-based guidance for
the public and healthcare professionals on the
management of knee OA, the HKCOS published
a position statement in August 2022 (Table 1).6
This position statement was developed based on a
consensus survey conducted in June 2022, along
with a review of high-quality evidence in the
literature. A total of 26 treatment recommendations
were formulated, reflecting the consensus of
expert orthopaedic surgeons in Hong Kong. The
methodology used to develop this position statement
is available on the College’s website.6
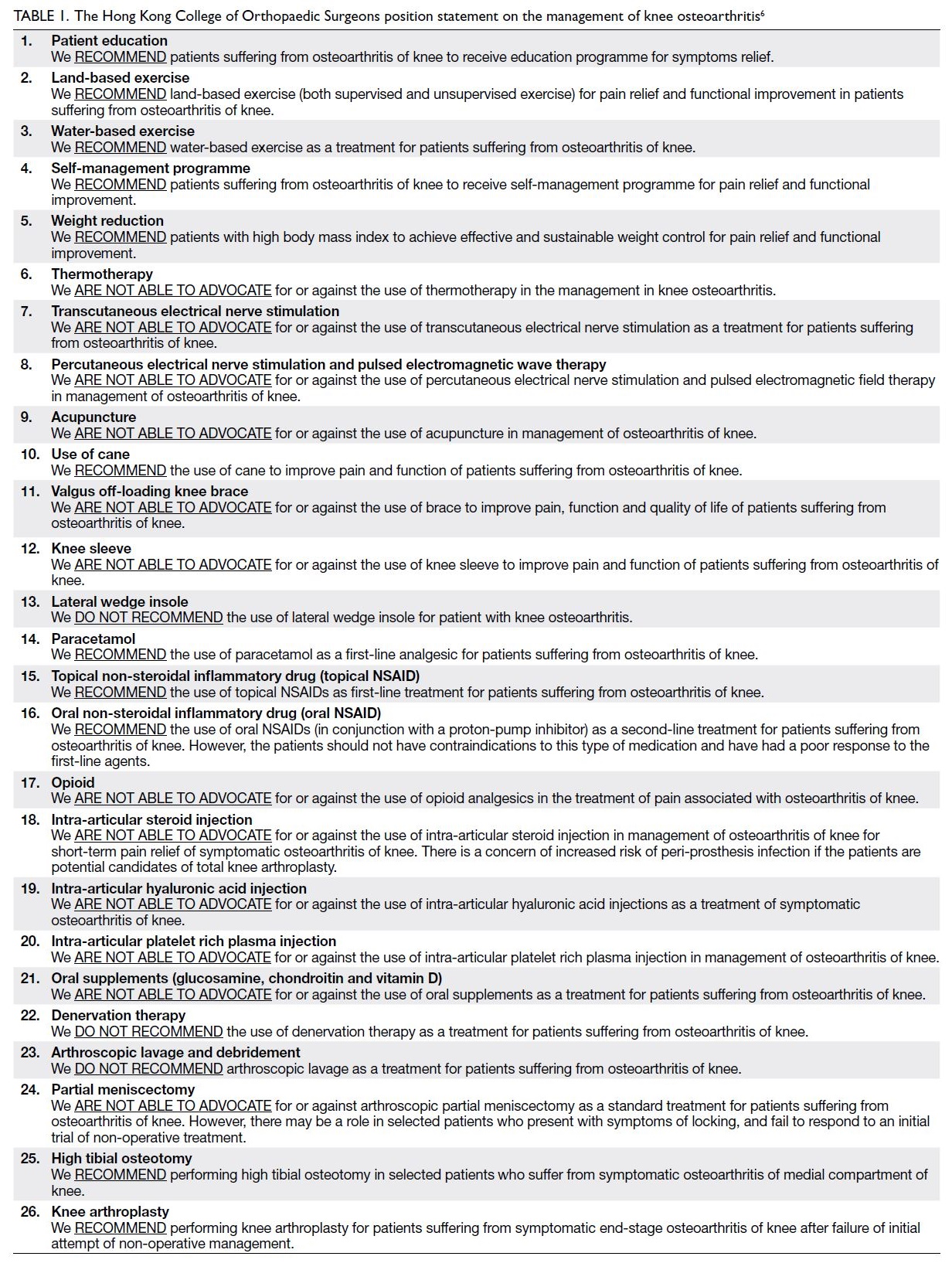
Table 1. The Hong Kong College of Orthopaedic Surgeons position statement on the management of knee osteoarthritis6
To gather updated expert opinions on the
management of knee OA, the College conducted a
second survey in January 2024. This article presents
the findings from the 2022 and 2024 surveys.
Methods
This study was conducted under the supervision
and ethical oversight of the Council of HKCOS.
The requirement to obtain informed consent from
participants was waived by the Council. Two cross-sectional
surveys were conducted online in June
2022 and January 2024, respectively. The same online
questionnaire was used for both study periods to
ensure consistency in data collection.
The online questionnaire was developed by the
HKCOS Osteoarthritis of the Knee Working Group
(HKCOS-OAKWG).6 A total of 26 interventions for
knee OA were selected based on the practices of
orthopaedic surgeons in Hong Kong and guidelines
from international recognised organisations.7 8 An
independent literature review was conducted, and
the quality of evidence was graded according to
the Oxford Centre for Evidence-Based Medicine
levels of evidence.9 Available Level 1 and Level 2 evidence up to March 2022 was summarised for each
intervention.
Fellows of the HKCOS listed in the Specialist
Register (Orthopaedics and Traumatology) of the
Hong Kong Medical Council were invited via email
to participate in the surveys. Each survey remained
open for 4 weeks. The surveys collected opinions on
the 26 interventions. For each item, the questionnaire
provided: (1) a brief description of the intervention;
(2) a concise summary of the supporting Level
1 and Level 2 evidence; and (3) a single question
asking whether the expert would recommend the
intervention. Expert panellists were instructed to
select one of three response options: ‘Recommend’,
‘Do not recommend’, or ‘Abstain’.
Statistics
Descriptive statistics were reported for the two
cross-sectional surveys conducted in 2022 and
2024. These included the number of expert
panellists who participated in each survey with their
recommendations regarding the 26 interventions for
knee OA. The number of panellists who participated
in both the 2022 and 2024 surveys was also recorded.
The experience of the expert panel was described
based on the number of years each panellist had been
registered as a specialist with the Hong Kong Medical
Council. Consensus was defined as a minimum of
70% agreement among the expert panellists. The
resulting recommendations formed the basis of the
HKCOS position statement. No analytical statistical
tests were performed.
Results
Composition of the expert panels
A total of 106 expert panellists participated in
the 2022 survey, while 28 participated in the 2024 survey. At the time of survey distribution in June
2022 and January 2024, the College had 528 and 567
fellows, respectively. In June 2022, the numbers of
active fellows, overseas fellows, and inactive fellows
were 495, 4, and 27, respectively. The corresponding
numbers in January 2024 were 526, 7, and 34.10 The
response rates for the surveys were 20% in 2022 and
5% in 2024, respectively. Twenty expert panellists
participated in both the 2022 and 2024 surveys.
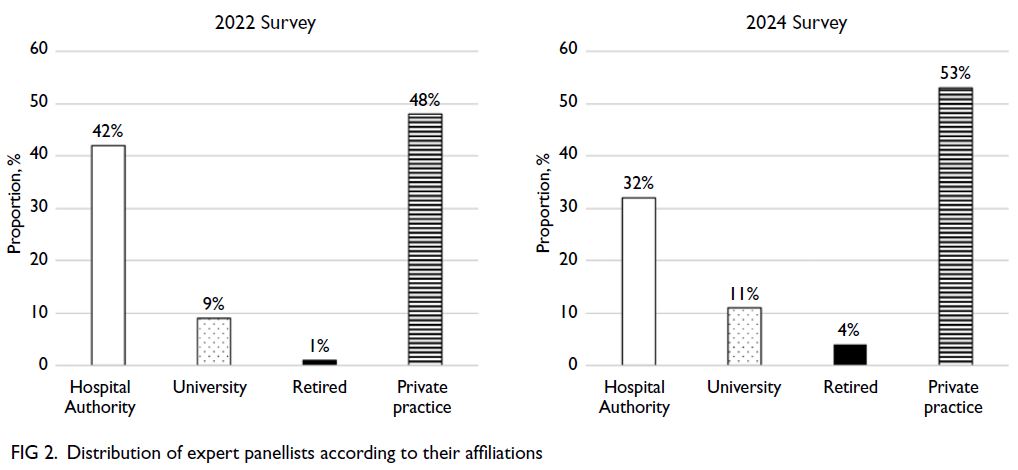
The mean duration of experience as registered
orthopaedic specialists with the Hong Kong Medical
Council (±standard deviation) was 15.6±9 years for
the 2022 cohort and 19.2±7 years for the 2024 cohort
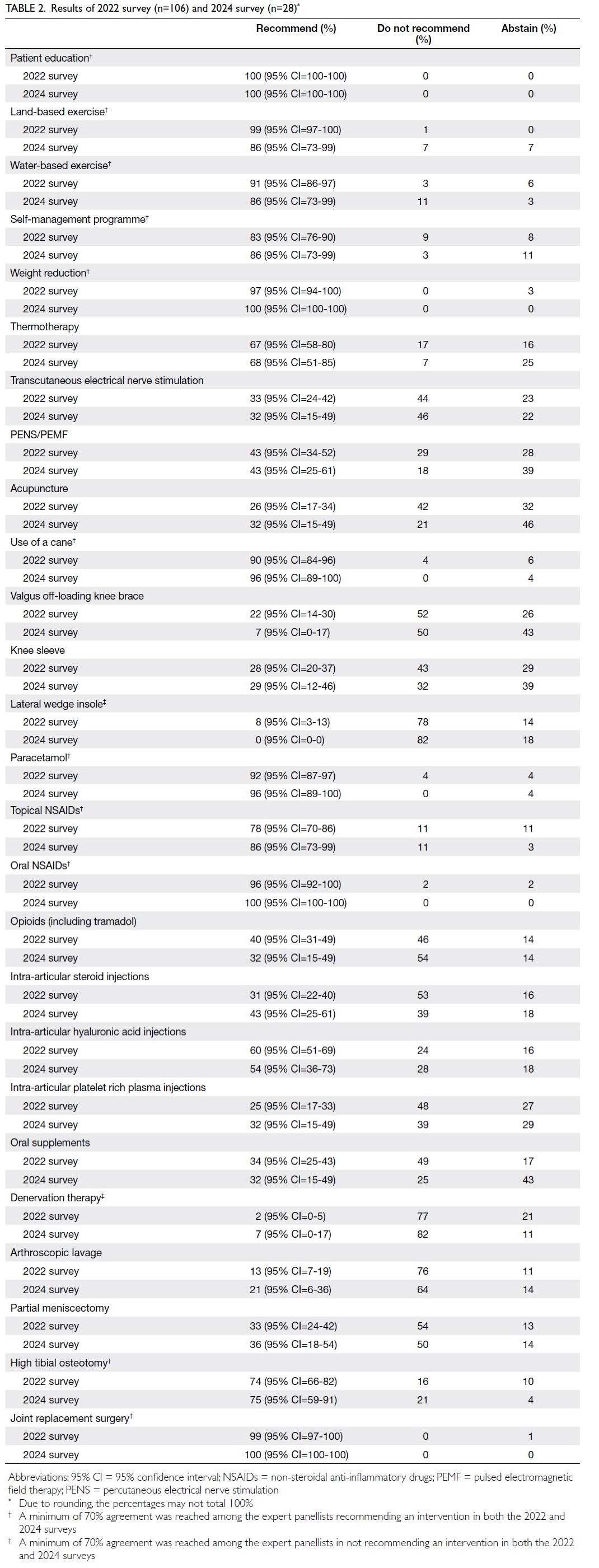
(Fig 1). The distribution of expert panellists according to their affiliations is presented in Figure 2.
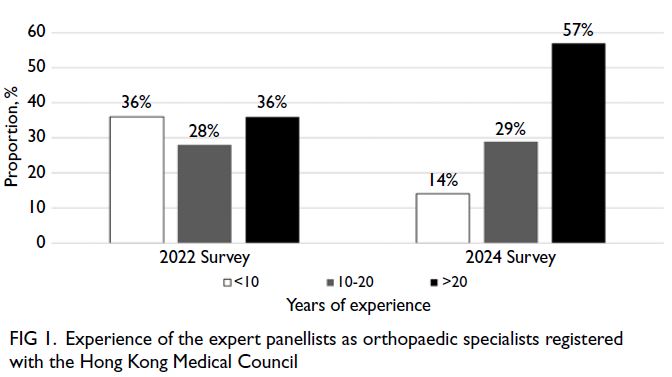
Figure 1. Experience of the expert panellists as orthopaedic specialists registered with the Hong Kong Medical Council
Recommendations of the expert panels
The results of the expert recommendations from the 2022 and 2024 surveys are summarised in Table 2.
Consensus was reached among the expert panellists
for 14 interventions in 2022 and 13 interventions in
2024. As consensus had already been achieved for
most treatment options in the first-round survey,
no changes were made to the HKCOS position
statement on the management of knee OA, and the
content of the second survey remained unchanged.
In both surveys, a supermajority of panellists (≥70%)
recommended 11 interventions: patient education;
land-based exercise; water-based exercise; self-management
programme; weight reduction; use of
a cane; oral paracetamol; topical non-steroidal anti-inflammatory
drugs (NSAIDs); oral NSAIDs; high
tibial osteotomy; and joint replacement surgery.
Conversely, at least 70% of respondents in both
surveys did not recommend the use of lateral wedge
insoles or denervation therapy. Consensus was
not achieved for 12 interventions in 2022 and 13
interventions in 2024.
Discussion
A consensus of 70% or greater agreement was reached
among the expert panellists for 14 interventions in
the 2022 survey and 13 interventions in the 2024
survey. Consensus remained consistent across
both cross-sectional surveys for 13 interventions,
including: recommendations in favour of patient
education, land-based and water-based exercise,
self-management programmes, weight reduction,
use of a cane, oral paracetamol, topical and oral
NSAIDs, high tibial osteotomy and joint replacement
surgery, as well as recommendations against the
use of lateral wedge insoles and denervation
therapy.
There are two primary objectives in the
management of knee OA: (1) control of disease
progression; and (2) control of symptoms. Regarding
disease control, it is rare to reverse the underlying
pathological changes, such as joint space narrowing
and varus malalignment of the lower limb, through
non-operative treatment once the condition is
established. The aim of management is to slow the progression of osteoarthritis by promptly identifying
and treating ‘joint-threatening’ pathologies (such
as symptomatic loose bodies, full-thickness, full-width
root tears of the meniscus, and spontaneous
osteonecrosis of the knee)6 11 and by controlling
risk factors associated with disease progression (eg,
through weight reduction and prevention of knee
injury).12 Regarding symptom control, most non-operative treatments focus on pain management13
and improving quality of life.14 Pain is the most
common presenting symptom in knee OA.15 However,
there is only a weak correlation between radiological
abnormalities and patient-reported symptoms.16
The severity of pain experienced is influenced
by sensitisation mechanisms—including both
peripheral and central sensitisation—rather than by
anatomical changes in the arthritic joint alone.15 It
is increasingly recognised that inflammation plays a
prominent role in the pathogenesis and symptoms
of OA.17 Inflammatory cytokines (eg, interleukin 6
and tumour necrosis factor alpha) and inflammatory
mediators (eg, prostaglandin and bradykinin)
contribute to peripheral sensitisation of nociceptors
in the subchondral plate and joint capsule by
activating G protein–coupled receptors, ionotropic
receptors, and tyrosine kinase receptors located
on nerve terminals and cell bodies.18 Accordingly,
most treatments for knee OA aim to control
inflammation in order to alleviate symptoms.7 The
cell bodies of nociceptors are located in the dorsal
root ganglia of the spinal cord, where nociceptive
input is transmitted to the brain and brainstem
via the spinothalamic tract, spinoreticular tract,
spinomesencephalic tract, and spinohypothalamic
tract.13 Persistent nociceptive stimulation leads to
central sensitisation, characterised by hyperactivity
and hyperexcitability of neurons in the brain and
spinal cord.19 Inflammation also contributes to
central sensitisation by increasing the production of
neurotransmitters and neuromodulators, including
glutamate and substance P.18 Furthermore, there
is a loss of inhibitory control due to a reduction in
inhibitory neurotransmitters, primarily gamma-aminobutyric
acid (GABA), resulting in heightened
pain sensitivity.18 The perception of nociceptive
stimuli as pain is further influenced by psychological
factors (such as depression, anxiety, and poor
coping skills) and social factors (such as workers’
compensation claims and lack of social support).
The interaction among biological, psychological, and
social factors is described by the biopsychosocial
model, which is considered important in the
development of chronic pain.19 As a result, education,
self-management programmes, and cognitive
behavioural therapy are also important treatment
strategies for knee OA.7
Surgical treatments, such as joint replacement
surgery and high tibial osteotomy, are typically
reserved for patients with end-stage knee arthritis
or those with persistent symptoms despite adequate
non-operative management.14
Patient education
Most patient education programmes provide guidance on: (1) the nature, presenting symptoms,
and treatment options for knee OA; (2) the importance of adherence to treatment and the
adoption of preventive lifestyle behaviours; and (3)
the expected natural disease course and treatment
outcomes.20 Patient education operates through a
theory of planned behaviour-based intervention.20
By modifying patients’ attitudes and the subjective
norms of family members, both symptoms and
quality of life can be improved, even in the absence
of changes in physical condition.20
Exercise, weight reduction, use of a cane, and
self-management programmes
There is high-quality evidence in the literature
supporting the effectiveness of exercise—both
land-based and water-based—along with weight
reduction, use of a cane, and self-management
programmes in reducing pain and improving quality
of life in patients with knee OA.21
Exercise alleviates symptoms of knee OA by
increasing lower limb muscle strength and improving
overall physical fitness.21 Improved muscle strength
alters joint biomechanics, thereby reducing joint
loading and pain. Aerobic exercise increases peak
oxygen uptake by muscles and enhances the patient’s
overall fitness, facilitating the performance of daily
activities and enhancing functional ability.21 Exercise
should be performed regularly, with sufficient—but
not excessive—intensity.14 Recommended land-based
activities include lower limb strengthening
exercises, static cycling, walking programmes, Tai
Chi, and Baduanjin,21 while water-based activities
include swimming and pool therapy.22
Obesity is a known risk factor for the
development of knee OA12 and the subsequent
need for joint replacement surgery.23 Beyond
increased mechanical loading, obesity is
associated with metabolic syndrome—a cluster of
metabolic disorders including abdominal obesity,
hyperlipidaemia, hypertension, and elevated fasting
serum glucose.24 Metabolic syndrome is increasingly
recognised as an important risk factor for OA due to
its association with systemic inflammation.25 Among
obese individuals with OA, disability may be reduced
with weight loss exceeding 5%.26 Evidence supports
the use of intensive low-energy diet programmes
for achieving weight loss and reducing pain in this
population.27
The use of a cane reduces weight-bearing
on the arthritic joint, thereby alleviating pain. A
randomised controlled trial has demonstrated
significant improvements in pain and function
among patients who use a cane for walking.28
Self-management programmes have been
shown to reduce pain and improve function in
patients with knee OA.29 30 31 In addition to education
and exercise, these programmes equip patients
with a range of coping and management strategies,
including pain coping techniques,29 joint protection and injury prevention strategies,30 and stress management skills.31
Topical non-steroidal anti-inflammatory
drugs, oral non-steroidal anti-inflammatory drugs, and paracetamol
Pain may arise when nociceptors in the knee joint
are stimulated.13 Although articular cartilage and
the meniscus are commonly damaged in knee OA,
they are aneural and therefore not direct sources
of pain. In contrast, nociceptors are present in
the subchondral bone, periosteum, joint capsule,
and infrapatellar fat pad.13 In a healthy joint, these
nociceptors are not stimulated during physiological
loading, meaning that individuals without OA do
not experience pain during daily activities such
as walking, squatting, or running. Inflammatory
cytokines, including interleukin 6, tumour necrosis
factor alpha, and other pro-inflammatory molecules
(eg, prostaglandin and bradykinin), increase in
response to joint injury or during OA flare-ups. These
molecules bind to nociceptors on the cell surface,
inducing hypersensitivity and hyperexcitability.
Consequently, pain may be experienced even during
normal joint loading in previously painless knees—a
phenomenon known as peripheral sensitisation.18
Non-steroidal anti-inflammatory drugs are effective
in alleviating pain in knee OA32 by reducing intra-articular
and circulating levels of inflammatory
molecules, including prostaglandins.
While oral NSAIDs are effective in relieving
OA-related pain, their side-effects warrant caution.33
Systemic NSAIDs should be used judiciously in
older patients and in individuals with peptic ulcer
disease, renal impairment, or a history of asthma
or ischaemic heart disease.34 Topical NSAIDs, by
contrast, have demonstrated efficacy in reducing
knee pain while offering a much safer side-effect
profile.35 As such, topical NSAIDs should be
considered before initiating oral formulations.34
Paracetamol has been shown to improve
pain and function in patients with knee OA.36 It is
considered a safe medication, even in patients at
higher risk of complications.7 However, overdose
can result in hepatotoxicity and death, necessitating
proper patient education regarding safe dosing
practices.8
Joint replacement surgery and high tibial
osteotomy
Both joint replacement surgery and high tibial
osteotomy are salvage operations for symptomatic
end-stage knee arthritis following unsuccessful
non-operative treatment. Both procedures have
demonstrated effectiveness in relieving pain in
patients with knee OA.37 38 Joint replacement surgery
has been shown to improve function regardless of the extent of joint involvement.39 In contrast, high
tibial osteotomy is effective for symptom relief only
in a selected group of patients whose symptomatic
OA is confined to the medial compartment of the
knee.38
Comparison of our recommendations and
international guidelines
The recommendations of the HKCOS position
statement on the management of knee OA,6 alongside
those of the National Institute for Health and
Care Excellence (NICE) guideline,14 the American
Academy of Orthopaedic Surgeons (AAOS)
guideline,7 and the Osteoarthritis Research Society International (OARSI) guideline,33 are summarised in Table 3.
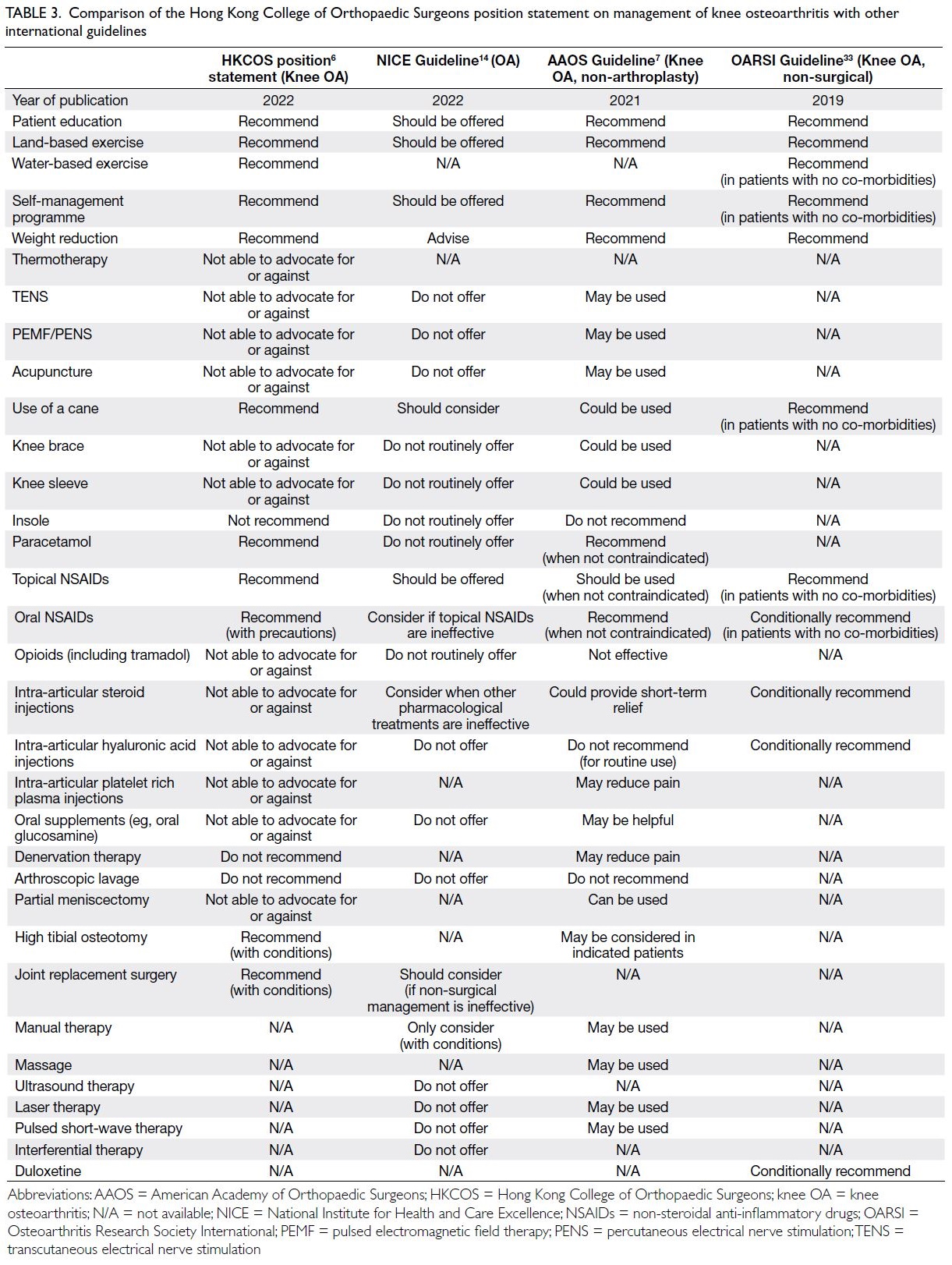
Table 3. Comparison of the Hong Kong College of Orthopaedic Surgeons position statement on management of knee osteoarthritis with other international guidelines
All of these guidelines recommend patient
education, exercise, self-management programmes,
weight reduction, and the use of a cane as
appropriate management strategies for patients with
knee OA.6 7 14 33 With respect to knee biomechanical
interventions, such as knee braces and sleeves,
the AAOS guideline is unique in suggesting that
these “may be used” in knee OA.7 Concerning foot
biomechanical interventions, the HKCOS, NICE,
and AAOS guidelines advise against the use of lateral
wedge insoles.6 7 14
For pharmacological treatment, all reviewed
guidelines recommend the use of NSAIDs, either in
topical or oral formulations.6 7 14 33 However, owing to the increased risk of adverse effects associated with
oral NSAIDs in patients with co-morbidities, both
HKCOS and NICE recommend topical NSAIDs
as first-line treatment, reserving oral NSAIDs for
second-line use.6 14
There is variation in guidance concerning the
use of oral paracetamol. While HKCOS and AAOS
support its use as a first-line treatment in knee OA,6 7
NICE and OARSI do not recommend its routine
use.14 33 None of these guidelines recommend opioids
for the treatment of knee OA.6 7 14 33 Regarding
intra-articular steroid injections, the NICE, AAOS,
and OARSI guidelines either recommend or
conditionally recommend their use for short-term
symptom relief.7 14 33
In contrast, intra-articular hyaluronic acid
injections are not recommended in the NICE and
AAOS guidelines.7 14 The only reviewed guideline
that conditionally supports their use is the OARSI
guideline.33
Based on the comparison outlined above,
substantial differences are observed among the
various guidelines (Table 3), despite all having
evaluated the same set of treatment options for
knee OA and drawing upon similar English-language
literature. These differences may reflect
variations in cultural context and healthcare systems
across different geographical regions. Hong Kong is distinct from North America, Europe, and the
United Kingdom due to the considerable influence
of traditional Chinese medicine (TCM) within its
healthcare system. Many patients in Hong Kong
seeking orthopaedic care for knee OA—whether
through the Hospital Authority or private healthcare
providers—also receive TCM treatment. Some
doctors registered with the Medical Council of
Hong Kong have received training in TCM, and
basic education in TCM is included in the Bachelor
of Medicine and Bachelor of Surgery curriculum
in Hong Kong. It is thus crucial for the HKCOS to
develop a position statement tailored to the local
population. The comparison of various guidelines
highlights differences between the HKCOS position
statement and guidelines issued by other reputable
international organisations. The recommendations
put forward by HKCOS may be better suited to
the needs of patients in Hong Kong. This position
statement also serves a valuable reference for
healthcare systems in which TCM plays a prominent
role, including those in Mainland China, Taiwan,
Korea, and Japan.
Limitations
The present study has several limitations. First, its
descriptive design precluded the use of analytical
statistics; as a result, we were unable to identify
whether there were significant shifts in opinion
regarding interventions for knee OA within the
Hong Kong orthopaedic community between 2022
and 2024. Second, only 19% of the expert panellists
who participated in the 2022 survey also took part
in the 2024 study. Consequently, we could not assess
potential changes in opinion among those who did
not respond in 2024. Third, the overall response rate
for the 2024 survey was low, which may limit the
representativeness of the findings and reduce their
generalisability to the wider orthopaedic specialist
population in Hong Kong. Lastly, the threshold for
consensus, defined as a minimum of 70% agreement
among the expert panellists, was arbitrary and may
not be universally accepted.
Conclusion
Findings from both the 2022 and 2024 surveys
demonstrated consistent expert consensus on key
recommended and non-recommended interventions
for knee OA. The recommendations provide
evidence-based guidance to the public and medical
practitioners regarding the effectiveness of various
management strategies for knee OA.
Author contributions
The author solely contributed to the concept or design of the
study, acquisition of the data, analysis or interpretation of the
data, drafting of the manuscript, and critical revision of the
manuscript for important intellectual content.
The author had full access to the data, contributed to the study, approved the final version for publication, and takes responsibility for its accuracy and integrity.
Conflicts of interest
The author has disclosed no conflicts of interest.
Acknowledgement
The author would like to acknowledge the contributions of the
following Fellows of the Hong Kong College of Orthopaedic
Surgeons, who served as members of the expert panel
and provided recommendations on interventions for the
management of knee osteoarthritis in the survey conducted
in 2022 (in alphabetical order):
Chan Baldwin, Chan Ka-wah, Chan Sai-keung, Chan Shiuwai, Chan Tsang-tung, Chan Tze-wang, Chan Wai-kwan Vincent, Chan Wai-lam, Chan Wai-sing, Chang His-tse Joseph Jeremy, Chang Shao, Chang Yun-po Robert, Cheng Hung-on, Cheong Peng-meng, Cheung Chi-nok, Cheung Ho-man, Cheung Man-hong, Cheung Pui-yin Jason, Cheung Wai-yuen, Cheung Wang-yan Warren, Cheung Yim-ling Amy, Chien Ping Eric, Chiu Chi-kit, Chiu Kwong-yuen Peter, Choi Shing-hing, Choi Sum-hung, Chow Kai-pun, Chu Kai-man, Chun Siu-yeung, Chung Kwong-yin, Chung Man-ting Marvin, Fan Chi-ho Jason, Fang Christian Xinshuo, Fu Chun-him Henry, Fu Wai-kee, Fung Kwai-yau, Hau Vincent, Ho Ki-wai, Ho Sheung-tung, Hung Leong-pan, Kwok Hau-yan, Lai Kam-keung, Lau Chi-yuen, Lau Chi-yuk, Lau Hoi-kuen, Lau Tak-wing, Lau Yip-kwong Francis, Law Sheung-wai, Law Ying-kan, Lee Qunn-jid, Lee Sung-yee, Lee Yeung-fai, Leung Ka-hei, Leung Yum-kwong, Ling Ka-kin Samuel, Loong Tak-wan, Lui Ming-yan, Man Lok-pong, Ng Fu-yuen, Ng Cheukkee Kenneth, Ng Pak-lin Eugene, Ng Wai-kit Raymond, Ng Weng-io, Ngai Wai-kee, Ong Tim-yun Michael, Sin Cheuk-hang, Siu Kam-to, Sun Lun-kit, Sun Kin-wai Kelvin, Tam Ka-ki, Tam Kwok-wai Kelvin, Tang Yan-ho Bruce, Tang Yuk-kwan, Tong Hoi-yiu Sara, Tse Lung-fung, Tsoi Chi-wah Danny, Tung Kam-lung, Wong Hok-leung, Wong Kwok-shing Patrick, Wong Man-kwan, Wong Nang-man Raymond, Wong Sze-hung, Wu Daniel Yiang, Wu Tsz-kit, Yang Isaac Bruce, Yeung Lok-yin Michael, Yeung Sze-tsun Eric, Yeung Yip-kan, Yuen Shiu-him Jonathan, Yung Shing-yat Colin.
Chan Baldwin, Chan Ka-wah, Chan Sai-keung, Chan Shiuwai, Chan Tsang-tung, Chan Tze-wang, Chan Wai-kwan Vincent, Chan Wai-lam, Chan Wai-sing, Chang His-tse Joseph Jeremy, Chang Shao, Chang Yun-po Robert, Cheng Hung-on, Cheong Peng-meng, Cheung Chi-nok, Cheung Ho-man, Cheung Man-hong, Cheung Pui-yin Jason, Cheung Wai-yuen, Cheung Wang-yan Warren, Cheung Yim-ling Amy, Chien Ping Eric, Chiu Chi-kit, Chiu Kwong-yuen Peter, Choi Shing-hing, Choi Sum-hung, Chow Kai-pun, Chu Kai-man, Chun Siu-yeung, Chung Kwong-yin, Chung Man-ting Marvin, Fan Chi-ho Jason, Fang Christian Xinshuo, Fu Chun-him Henry, Fu Wai-kee, Fung Kwai-yau, Hau Vincent, Ho Ki-wai, Ho Sheung-tung, Hung Leong-pan, Kwok Hau-yan, Lai Kam-keung, Lau Chi-yuen, Lau Chi-yuk, Lau Hoi-kuen, Lau Tak-wing, Lau Yip-kwong Francis, Law Sheung-wai, Law Ying-kan, Lee Qunn-jid, Lee Sung-yee, Lee Yeung-fai, Leung Ka-hei, Leung Yum-kwong, Ling Ka-kin Samuel, Loong Tak-wan, Lui Ming-yan, Man Lok-pong, Ng Fu-yuen, Ng Cheukkee Kenneth, Ng Pak-lin Eugene, Ng Wai-kit Raymond, Ng Weng-io, Ngai Wai-kee, Ong Tim-yun Michael, Sin Cheuk-hang, Siu Kam-to, Sun Lun-kit, Sun Kin-wai Kelvin, Tam Ka-ki, Tam Kwok-wai Kelvin, Tang Yan-ho Bruce, Tang Yuk-kwan, Tong Hoi-yiu Sara, Tse Lung-fung, Tsoi Chi-wah Danny, Tung Kam-lung, Wong Hok-leung, Wong Kwok-shing Patrick, Wong Man-kwan, Wong Nang-man Raymond, Wong Sze-hung, Wu Daniel Yiang, Wu Tsz-kit, Yang Isaac Bruce, Yeung Lok-yin Michael, Yeung Sze-tsun Eric, Yeung Yip-kan, Yuen Shiu-him Jonathan, Yung Shing-yat Colin.
The author would like to acknowledge the contributions of the
following Fellows of the Hong Kong College of Orthopaedic
Surgeons, who served as members of the expert panel
that provided recommendations on interventions for the
management of knee osteoarthritis in the 2024 survey (in
alphabetical order):
Chan Shiu-wai, Chan Wai-lam, Cheung Chi-nok, Cheung Wang-yan Warren, Chiu Kwong-yuen Peter, Choi Shing-hing, Fu Chun-him Henry, Ho Sheung-tung, Lam Chi-keung Johnson, Lau Pui-yau, Lee Qunn-jid, Leung Ka-hei, Liem Man-shing, Ng Fu-yuen, Wong Hok-leung, Yeung Sai-hung.
Chan Shiu-wai, Chan Wai-lam, Cheung Chi-nok, Cheung Wang-yan Warren, Chiu Kwong-yuen Peter, Choi Shing-hing, Fu Chun-him Henry, Ho Sheung-tung, Lam Chi-keung Johnson, Lau Pui-yau, Lee Qunn-jid, Leung Ka-hei, Liem Man-shing, Ng Fu-yuen, Wong Hok-leung, Yeung Sai-hung.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This research was approved by the Council of the Hong
Kong College of Orthopaedic Surgeons. The requirement for
informed consent was waived by the Council.
References
1. The Hong Kong College of Orthopaedic Surgeons.
Constitution. Available from: https://www.hkcos.org.hk/aboutus_constitution.asp. Accessed 4 Jul 2022.
2. Tang X, Wang SF, Zhan SY, et al. The prevalence of
symptomatic knee osteoarthritis in China. Results from the
China health and retirement longitudinal study. Arthritis
Rheumatol 2016;68:648-53. Crossref
3. Woo J. Age and Ageing journal 50th anniversary
commentary series. Healthcare for older people in Asia.
Age Ageing 2022;51:afab189. Crossref
4. Hospital Authority, Hong Kong SAR Government. Elective
total joint replacement surgery. 2023. Available from:
www.ha.org.hk/visitor/ha_visitor_index.asp?Parent_ID=214172&Content_ID=221223#. Accessed 26 Feb 2024.
5. GBD 2021 Osteoarthritis Collaborators. Global, regional,
and national burden of osteoarthritis, 1990-2020 and
projections to 2050: a systematic analysis for the Global
Burden of Disease Study 2021. Lancet Rheumatol
2023;5:e508-22. Crossref
6. Yau WP, Chiu CK, Cheung S, Cheung A. The Hong Kong
College of Orthopaedic Surgeons position statement in
management of osteoarthritis of knee. Available from:
https://www.hkcos.org.hk/Position_Statement/HKCOS_Position_Statement_in_Management_of_Osteoarthritis_of_Knee.pdf . Accessed 26 Feb 2024.
7. American Academy of Orthopaedic Surgeons.
Management of osteoarthritis of the knee (nonarthroplasty).
Evidence-based clinical practice guideline.
Available from: https://www.aaos.org/globalassets/quality-and-practice-resources/osteoarthritis-of-the-knee/oak3cpg.pdf. Accessed 26 Feb 2024.
8. McAlindon TE, Bannuru RR, Sullivan MC, et al. OARSI
guidelines for the non-surgical management of knee
osteoarthritis. Osteoarthritis Cartilage 2014;22:363-88. Crossref
9. Oxford Centre for Evidence-Based Medicine. OCEBM
levels of evidence. Available from: http://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence. Accessed 26 Feb 2024.
10. The Hong Kong College of Orthopaedic Surgeons.
Statistics. Number of Fellows. Available from: https://www.hkcos.org.hk/aboutus_statistics.asp. Accessed 16 Sep 2024.
11. Driban JB, Harkey MS, Barbe MF, et al. Risk factors and
the natural history of accelerated knee osteoarthritis:
a narrative review. BMC Musculoskeletal Disord
2020;21:332. Crossref
12. Glyn-Jones S, Palmer AJ, Agricola R, et al. Osteoarthritis. Lancet 2015;386:376-87. Crossref
13. Gwilym SE, Pollard TC, Carr AJ. Understanding pain in
osteoarthritis. J Bone Joint Surg Br 2008;90:280-7. Crossref
14. National Institute for Health and Care Excellence.
Osteoarthritis in over 16s: diagnosis and management.
Available from: http://www.nice.org.uk/guidance/ng226. Accessed 26 Feb 2024.
15. Lane NE, Brandt K, Hawker G, et al. OARSI-FDA initiative:
defining the disease state of osteoarthritis. Osteoarthritis
Cartilage 2011;19:478-82. Crossref
16. Courties A, Kouki I, Soliman N, Mathieu S, Sellam J.
Osteoarthritis year in review 2024: epidemiology and
therapy. Osteoarthritis Cartilage 2024;32:1397-404. Crossref
17. Jenei-Lanzl Z, Zaucke F. Osteoarthritis year in review
2024: biology. Osteoarthritis Cartilage 2025;33:58-66. Crossref
18. Matsuda M, Huh Y, Ji RR. Roles of inflammation,
neurogenic inflammation, and neuroinflammation in pain.
J Anesth 2019;33:131-9. Crossref
19. Cohen SP, Vase L, Hooten WM. Chronic pain: an update
on burden, best practices, and new advances. Lancet
2021;397:2082-97. Crossref
20. Saffari M, Emami Meybodi MK, Sanaeinasab H, Karami A,
Pakpour AH, Koenig HG. A theory of planned behavior–based intervention to improve quality of life in patients
with knee/hip osteoarthritis: a randomized controlled trial.
Clin Rheumatol 2018;37:2505-15. Crossref
21. Fransen M, McConnell S, Harmer AR, Van der Esch M,
Simic M, Bennell KL. Exercise for osteoarthritis of the
knee. Cochrane Database Syst Rev 2015;2015:CD004376. Crossref
22. Silva LE, Valim V, Pessanha AP, et al. Hydrotherapy versus
conventional land-based exercise for the management
of patients with osteoarthritis of the knee: a randomized
clinical trial. Phys Ther 2008;88:12-21. Crossref
23. Chen L, Yao F, Wang T, et al. Horizontal fissuring at the
osteochondral interface: a novel and unique pathological
feature in patients with obesity-related osteoarthritis. Ann
Rheum Dis 2020;79:811-8. Crossref
24. Courties A, Gualillo O, Berenbaum F, Sellam J. Metabolic
stress-induced joint inflammation and osteoarthritis.
Osteoarthritis Cartilage 2015;23:1955-65. Crossref
25. Puenpatom RA, Victor TW. Increased prevalence of
metabolic syndrome in individuals with osteoarthritis: an
analysis of NHANES III data. Postgrad Med 2009;121:9-20. Crossref
26. Christensen R, Bartels EM, Astrup A, Bliddal H. Effect of
weight reduction in obese patients diagnosed with knee
osteoarthritis: a systematic review and meta-analysis. Ann
Rheum Dis 2007;66:433-9. Crossref
27. Bliddal H, Leeds AR, Stigsgaard L, Astrup A, Christensen R.
Weight loss as treatment for knee osteoarthritis in obese
patients: 1-year results from a randomised controlled trial.
Ann Rheum Dis 2011;70:1798-803. Crossref
28. Jones A, Silva PG, Silva AC, et al. Impact of cane use on pain,
function, general health and energy expenditure during
gait in patients with knee osteoarthritis: a randomised
controlled trial. Ann Rheum Dis 2012;71:172-9. Crossref
29. Somers TJ, Blumenthal JA, Guilak F, et al. Pain coping skills
and lifestyle behavioural weight management in patients
with knee osteoarthritis: a randomized controlled study.
Pain 2012;153:1199-209. Crossref
30. Hurley MV, Walsh NE, Mitchell HL, et al. Clinical
effectiveness of a rehabilitation program integrating
exercise, self-management, and active coping strategies
for chronic knee pain: a cluster randomized trial. Arthritis
Rheum 2007;57:1211-9. Crossref
31. Helminen EE, Sinikallio SH, Valjakka AL, Väisänen-Rouvali RH, Arokoski JP. Effectiveness of a cognitive-behaviour
group intervention for knee osteoarthritis pain:
a randomized controlled trial. Clin Rehabil 2015;29:868-81. Crossref
32. Schnitzer TJ, Kivitz A, Frayssinet H, Duquesroix B. Efficacy
and safety of naproxcinod in the treatment of patients
with osteoarthritis of the knee: a 13-week prospective,
randomized, multicenter study. Osteoarthritis Cartilage
2010;18:629-39. Crossref
33. Bannuru RR, Osani MC, Vaysbrot EE, et al. OARSI
guidelines for the non-surgical management of knee, hip,
and polyarticular osteoarthritis. Osteoarthritis Cartilage
2019;27:1578-89. Crossref
34. Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American
College of Rheumatology/Arthritis Foundation guideline
for the management of osteoarthritis of the hand, hip, and
knee. Arthritis Rheumatol 2020;72:220-3. Crossref
35. Dehghan M, Asgharian S, Khalesi E, Ahmadi A, Lorigooini Z.
Comparative study of the effect of Thymus daenensis gel
5% and diclofenac in patients with knee osteoarthritis.
Biomedicine (Taipei) 2019;9:9. Crossref
36. Prior MJ, Harrison DD, Frustaci ME. A randomized,
double-blind, placebo-controlled 12-week trial of
acetaminophen extended release for the treatment of
signs and symptoms of osteoarthritis. Curr Med Res Opin
2014;30:2377-87. Crossref
37. Heath EL, Ackerman IN, Cashman K, Lorimer M, Graves SE, Harris IA. Patient-reported outcomes after hip and knee arthroplasty: results from a large national registry. Bone Jt
Open 2021;2:422-32. Crossref
38. van Outeren MV, Waarsing JH, Brouwer RW, Verhaar JA,
Reijman M, Bierma-Zeinstra SM. Is a high tibial osteotomy
(HTO) superior to non-surgical treatment in patients
with varus malaligned medial knee osteoarthritis
(OA)? A propensity matched study using 2 randomized
controlled trial (RCT) datasets. Osteoarthritis Cartilage
2017;25:1988-93. Crossref
39. Wilson HA, Middleton R, Abram SG, et al. Patient
relevant outcomes of unicompartmental versus total knee
replacement: systematic review and meta-analysis. BMJ
2019;364:I352. Crossref