Hong Kong Med J 2024 Apr;30(2):90–3 | Epub 10 Apr 2024
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
EDITORIAL
Call to action: bridging gaps in lipid management
in Hong Kong
Bryan PY Yan, MD, FRCP1; Kui Kai Lau, DPhil, FRCP2; Andrea OY Luk, MD, FRCP3; Martin CS Wong, MD, MPH4,5
1 Department of Medicine and Therapeutics, The Chinese University of Hong Kong, Hong Kong SAR, China
2 Division of Neurology, Department of Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China
3 Department of Medicine and Therapeutics, The Chinese University of Hong Kong, Hong Kong SAR, China
4 The Jockey Club School of Public Health and Primary Care, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR, China
5 Editor-in-Chief, Hong Kong Medical Journal
Corresponding author: Dr Bryan PY Yan (bryan.yan@cuhk.edu.hk)
Atherosclerotic cardiovascular disease in Hong Kong
Cardiovascular disease is the third leading cause
of death in Hong Kong, contributing to 13% of
all deaths in 2020.1 According to the Hong Kong
Population Health Survey conducted between
2020 and 2022, the prevalence of high blood
cholesterol among individuals aged 15 to 84 years
in the Hong Kong general population increased
from 8.4% in 2003/20042 to 51.9% in 2022.3 Low-density
lipoprotein cholesterol (LDL-C) has been
recognised as one of the most important modifiable
risk factors for atherosclerotic cardiovascular
disease (ASCVD).4 Accordingly, optimal LDL-C
management is essential for reducing the incidence of
and mortality from ASCVD. Despite the availability
of effective and safe lipid-lowering therapies (LLTs)
and guidelines for managing elevated LDL-C and
other lipids, implementation remains a key challenge
in clinical practice.
Advancements in lipid-lowering therapies
A lower LDL-C level is highly beneficial because of
the direct correlation between the absolute reduction
in LDL-C level and reduced cardiovascular risk,
such that an incremental reduction in LDL-C level
leads to a proportional reduction in the number of
cardiovascular events.5 Statins are well-established
as effective LLTs; this recognition has been extended
to other non-statin therapies, including proprotein
convertase subtilisin/kexin type 9 inhibitors
(PCSK9is), ezetimibe, bempedoic acid, evinacumab,
and inclisiran.6 7 Clinical trials have demonstrated
that PCSK9is effectively lower LDL-C levels, thereby
surpassing previous recommendations (high risk:
<2.6 mmol/dL; very high risk: <1.8 mmol/dL) to
offer additional cardiovascular benefits to patients
(particularly those with high or very high ASCVD
risk) who failed to meet their target LDL-C goal despite maximally tolerated high-intensity statin therapy.6 8
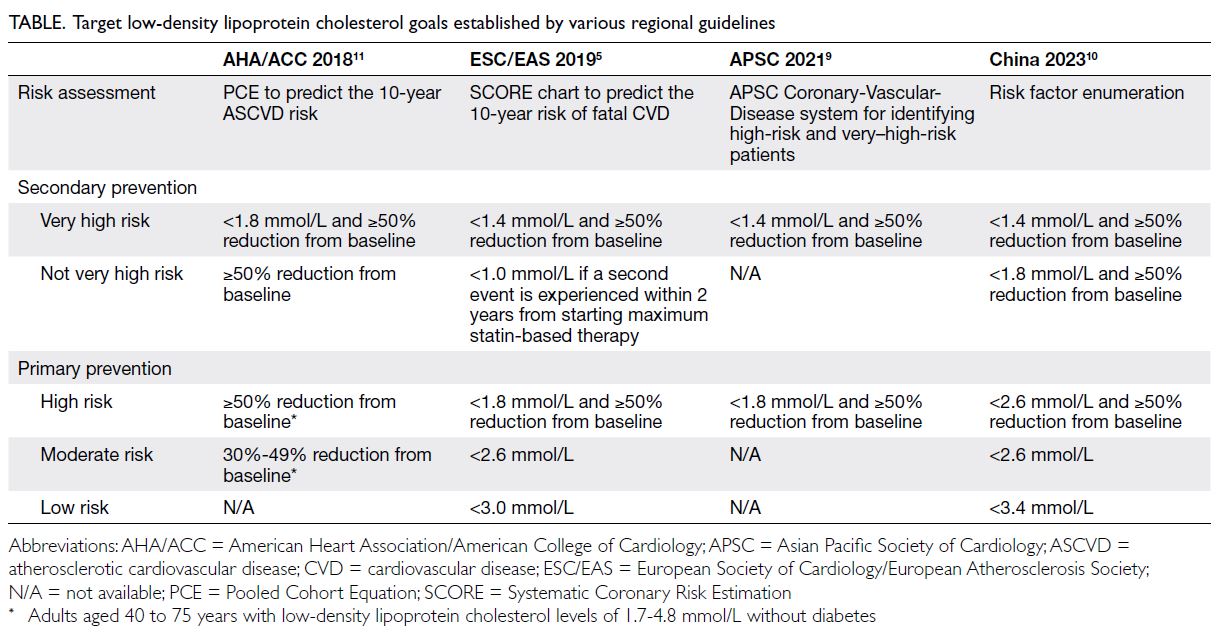
Adapting the latest evidence into current guidelines
The European Society of Cardiology and European
Atherosclerosis Society (ESC/EAS) revised their
guidelines in 2019 to integrate recent evidence
concerning ASCVD prevention.5 These updates
include a more aggressive approach with new LDL-C
targets across all cardiovascular risk categories,
as well as recommendations for lipid-lowering
strategies. Since these updates, other cardiology
societies (Table)1 5 10 11 and medical associations12 13
have also begun to recommend achieving the lowest
possible LDL-C levels, especially for patients with
very high ASCVD risk.
The 2019 ESC/EAS guidelines recommend
the following LDL-C targets for the prevention
of ASCVD in very high- and high-risk patients:
<1.4 mmol/L and <1.8 mmol/L (and 50% reduction
from baseline), respectively.5 Consistent with these
recommendations, the 2024 American Diabetes
Association guidelines recommend that patients
with diabetes aged 40 to 70 years receive moderate-intensity
statins, and such patients with one or
more ASCVD risk factors receive high-intensity
statins, to achieve LDL-C level <1.8 mmol/L and ≥50%
reduction from baseline.12 Statin therapy should
also be considered for young adults aged 20 to 39
years, depending on their existing risk factors.12
The American Heart Association/American Stroke
Association guidelines recommend a target LDL-C level of <1.8 mmol/L for patients who have experienced
transient ischaemic attack/ischaemic stroke with
atherosclerotic disease.13
If there is inadequate LDL-C reduction with
maximally tolerated statins, the addition of non-statin
options (eg, PCSK9is or ezetimibe) can be
considered according to the extent of reduction
required to reach the LDL-C goal.5 7 9 10 11 12 13
Low-density lipoprotein cholesterol target achievement remains challenging in Hong Kong
Low-density lipoprotein cholesterol management in
Hong Kong has gradually improved, but considerable
gaps in care persist. A territory-wide study conducted
between 2016 and 2021 revealed poor achievement
of LDL-C target goals among patients hospitalised
for acute coronary syndrome.14 The study showed low
rates of prescription for high-intensity statins (53%)
and combination LLTs (1.3%-3.8%) at discharge; LLT
and statin treatments were rarely intensified after
discharge.14 Notably, approximately 22% of patients
did not undergo follow-up lipid profile assessment
after discharge.14 This lack of follow-up has been
identified as an independent risk factor for all-cause
death and cardiovascular-related death.14
A separate study involving over 700 000
patients revealed gross underutilisation of statins
among patients with diabetes in Hong Kong,
such that most of this population failed to meet
LDL-C targets.15 Importantly, women and younger
individuals were particularly undertreated,
highlighting the need to address these age and sex
disparities in lipid management.15 Consistent with current evidence,5 a large cohort of local patients with ischaemic stroke (with or without significant large artery atherosclerosis) demonstrated that
the achievement of a target LDL level <1.8 mmol/L was
associated with a reduced risk of subsequent major
adverse cardiovascular events.16
Outdated recommendations in local settings
can hinder optimal lipid management. As a result,
physicians may fail to initiate appropriate LLT,
prioritise regular monitoring, or provide appropriate
follow-up care to assess treatment efficacy. Patients
may not recognise the dangers of elevated LDL-C
levels or understand the importance of lifestyle
modification and medication adherence, leading to
suboptimal outcomes.
Call to action: bridging gaps in lipid management
The International Atherosclerosis Society issued a call to action for improvements in lipid
management, based on a multinational survey that
involved 1758 physicians comprising cardiologists,
endocrinologists, neurologists/stroke specialists,
nephrologists, and general medicine practitioners
from Japan, Germany, Colombia and the Philippines;
the survey was designed to identify knowledge gaps
in clinical practice.17 The results highlighted three
major gaps in beliefs and behaviour across the four
countries: (1) physicians lacked clear guidance
concerning the management of higher-risk patients
who may benefit from aggressive LLT; (2) although
most physicians believed that they followed guideline
recommendations, only half knew the LDL-C target
for high-risk patients, and more than one-third had
no opinion concerning the safety of low LDL-C levels;
and (3) physicians were unsure of the potential effects
of statins on cognitive, renal, and hepatic functions, as well as the increased risk of haemorrhagic stroke
associated with low LDL-C levels.17 Taken together,
these findings highlighted key areas for enhanced
education and research efforts to bridge gaps in
lipid management.17 Physicians’ limited familiarity
with the rapidly changing guidelines hinders optimal
LDL-C management.
The Hong Kong Cardiovascular Task Force
published a consensus statement regarding ASCVD
prevention in 2016, based on the 2011 ESC/EAS
guidelines and the 2013 American Heart Association/American College of Cardiology guidelines.18
Although the consensus is valuable, it primarily
constitutes expert opinion and lacks endorsement
from any medical societies. Additionally, although
various international societies have established
guidelines for optimal lipid management, differences
among these recommendations (eg, pharmacological
treatment, lifestyle modification, and therapeutic
targets) may lead to confusion and uncertainty
among primary care physicians regarding the best
approach.19
Efforts to bridge current gaps in lipid
management in Hong Kong will require identifying
local therapeutic limitations and barriers to
optimising lipid management among physicians
and patients. Based on knowledge of these issues,
a consensus among local experts (ie, cardiologists,
endocrinologists, neurologists, nephrologists,
internists, general practitioners, nutritionists,
and other healthcare specialists) can be achieved
to provide practical recommendations that are
consistent with international guidelines and
adapted to local clinical practice.11 Considering the
complexities and time involved in developing local
guidelines, a practical course of action would involve
local medical societies across various specialties
collaborating to issue a joint statement that
recommends the adoption of appropriate guidelines,
thereby ensuring a more cohesive and unified
approach to lipid management in Hong Kong.
Local recommendations should also address
pertinent issues, such as greater adherence to
established guidelines—specifically, by encouraging
the prompt initiation and intensification of statin
therapy in eligible patients. Because the overall
ASCVD risk assessment is the basis for treatment
decisions in patients with dyslipidaemia,5 7 9
appropriate tools—adapted to the local population—should be used in routine clinical practice to ensure
that patients are adequately assessed and managed.
Additionally, the benefits of long-term adherence
to LLT should be consistently and effectively
communicated to patients.
Author contributions
All authors contributed to the development of the manuscript, approved the final version for publication, and take full responsibility for its accuracy and integrity.
Conflicts of interest
KK Lau has received grants from the Croucher Foundation,
Research Fund Secretariat of the Food and Health Bureau,
Innovation and Technology Bureau, Research Grants
Council, Amgen, Boehringer Ingelheim, Eisai, and Pfizer, as
well as consultation fees from Amgen, Boehringer Ingelheim,
Daiichi Sankyo, and Sanofi, all unrelated to the submitted
work. AOY Luk has served as a member of advisory panels
for Amgen, AstraZeneca, Boehringer Ingelheim, and Sanofi
and has received research support from Amgen, Asia
Diabetes Foundation, Bayer, Biogen, Boehringer Ingelheim,
Lee’s Pharmaceutical, MSD, Novo Nordisk, Roche, Sanofi,
Sugardown Ltd., and Takeda, unrelated to the submitted
work. As editors of the journal, BPY Yan, KK Lau and MCS
Wong were not involved in the peer review process.
Acknowledgement
Medical writing support was provided by Veronica Yap and Analyn Lizaso of Weber Shandwick Health HK.
Funding/support
This editorial received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. Centre for Health Protection, Department of Health, Hong
Kong SAR Government. Heart diseases. Available from:
https://www.chp.gov.hk/en/healthtopics/content/25/57.html. Accessed 23 Jan 2024.
2. Centre for Health Protection, Department of Health, Hong
Kong SAR Government and Department of Community
Medicine, University of Hong Kong. Population Health
Survey 2003/2004. Available from: https://www.chp.gov.hk/files/pdf/report_on_population_health_survey_2003_2004_en.pdf. Accessed 23 Jan 2024.
3. Non-Communicable Disease Branch, Centre for Health
Protection, Department of Health, Hong Kong SAR
Government. Population Health Survey 2020-22 (Part II).
Published April 2023. Available from: https://www.chp.gov.hk/files/pdf/dh_phs_2020-22_part_2_report_eng_rectified.pdf. Accessed 23 Jan 2024.
4. Borén J, Chapman MJ, Krauss RM, et al. Low-density
lipoproteins cause atherosclerotic cardiovascular disease:
pathophysiological, genetic, and therapeutic insights: a
consensus statement from the European Atherosclerosis
Society Consensus Panel. Eur Heart J 2020;41:2313-30. Crossref
5. Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS
Guidelines for the management of dyslipidaemias: lipid
modification to reduce cardiovascular risk. Eur Heart J
2020;41:111-88. Crossref
6. Furtado RH, Giugliano RP. What lessons have we learned
and what remains to be clarified for PCSK9 inhibitors?
A review of FOURIER and ODYSSEY outcomes trials.
Cardiol Ther 2020;9:59-73. Crossref
7. Lloyd-Jones DM, Morris PB, Ballantyne CM, et al. 2022
ACC Expert consensus decision pathway on the role of
nonstatin therapies for LDL-cholesterol lowering in the
management of atherosclerotic cardiovascular disease risk:
a report of the American College of Cardiology Solution
Set Oversight Committee. J Am Coll Cardiol 2022;80:1366-418. Crossref
8. Catapano AL, Graham I, De Backer G, et al. 2016 ESC/EAS Guidelines for the management of dyslipidaemias. Eur Heart J 2016;37:2999-3058. Crossref
9. Koh N, Ference BA, Nicholls SJ, et al. Asian Pacific
Society of Cardiology consensus recommendations on
dyslipidaemia. Eur Cardiol 2021;16:e54. Crossref
10. Li JJ, Zhao SP, Zhao D, et al. 2023 Chinese guideline for lipid management. Front Pharmacol 2023;14:1190934. Crossref
11. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College
of Cardiology/American Heart Association Task Force
on Clinical Practice Guidelines. J Am Coll Cardiol
2019;73:e285-350. Crossref
12. American Diabetes Association Professional Practice
Committee. 10. Cardiovascular disease and risk
management: standards of care in diabetes—2024.
Diabetes Care 2024;47(Suppl 1):S179-218. Crossref
13. Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021
Guideline for the prevention of stroke in patients with
stroke and transient ischemic attack: a guideline from
the American Heart Association/American Stroke
Association. Stroke 2021;52:e364-467. Crossref
14. Sun H, Lai A, Tan GM, Yan B. Therapeutic gaps in
low-density lipoprotein cholesterol management have
narrowed over time but remain wide: a Hong Kong–wide
study of 40,141 acute coronary syndrome patients from
2016 to 2021. Presented at the European Society of Cardiology Congress 2023; 2023 Aug
25-28; Amsterdam: Netherlands. Crossref
15. Wu H, Lau ES, Yang A, et al. Trends in diabetes-related
complications in Hong Kong, 2001-2016: a retrospective
cohort study. Cardiovasc Diabetol 2020;19:60. Crossref
16. Lau KK, Chua BJ, Ng A, et al. Low-density lipoprotein
cholesterol and risk of recurrent vascular events in Chinese
patients with ischemic stroke with and without significant
atherosclerosis. J Am Heart Assoc. 2021;10:e021855. Crossref
17. Barter PJ, Yamashita S, Laufs U, et al. Gaps in beliefs and
practice in dyslipidaemia management in Japan, Germany,
Colombia and the Philippines: insights from a web-based
physician survey. Lipids Health Dis 2020;19:131. Crossref
18. Cheung BM, Cheng CH, Lau CP, et al. 2016 consensus
statement on prevention of atherosclerotic cardiovascular
disease in the Hong Kong population. Hong Kong Med J
2017;23:191-201. Crossref
19. Singh M, McEvoy JW, Khan SU, et al. Comparison of
transatlantic approaches to lipid management: the AHA/ACC/Multisociety Guidelines vs the ESC/EAS Guidelines.
Mayo Clin Proc 2020;95:998-1014. Crossref