Hong Kong Med J 2024 Apr;30(2):164–6 | Epub 11 Apr 2024
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Acute chorioamnionitis following amnioreduction for polyhydramnios in placental chorioangioma complicating pregnancy: a case report
Janice TC Leung, MB, ChB; WY Lok, MSc, FHKAM (Obstetrics and Gynaecology); William WK To, MD, FRCOG; CW Kong, MSc, FHKAM (Obstetrics and Gynaecology)
Department of Obstetrics and Gynaecology, United Christian Hospital, Hong Kong SAR, China
Corresponding author: Dr CW Kong (melizakong@gmail.com)
Case presentation
In October 2022, a 29-year-old nulliparous woman at
30 weeks of gestation was found to have a larger-than-dates
uterus with symphysial fundal height of 38 cm.
Her previous antenatal course had been uneventful
with scan at 20 weeks of gestation showing normal
fetal morphology and liquor volume. Ultrasound
revealed polyhydramnios with amniotic fluid index
(AFI) of up to 42 cm but normal fetal growth and
morphology. An echogenic lesion measuring
4.7×5.6×4.5 cm3 was seen in the placenta. The lesion
had feeding vessels visible on colour flow Doppler and pulsatile flow on pulsed wave Doppler (Fig 1).
There were no signs of fetal anaemia or hydrops
fetalis. The diagnosis of placental chorioangioma
was made. A standard 75-g oral glucose tolerance
test was performed due to polyhydramnios and
revealed mild gestational diabetes mellitus with
normal fasting level (4.7 mmol/L) and marginally
raised 2-hour post-loading level of 8.6 mmol/L
(normal range for pregnancy, <8.5).
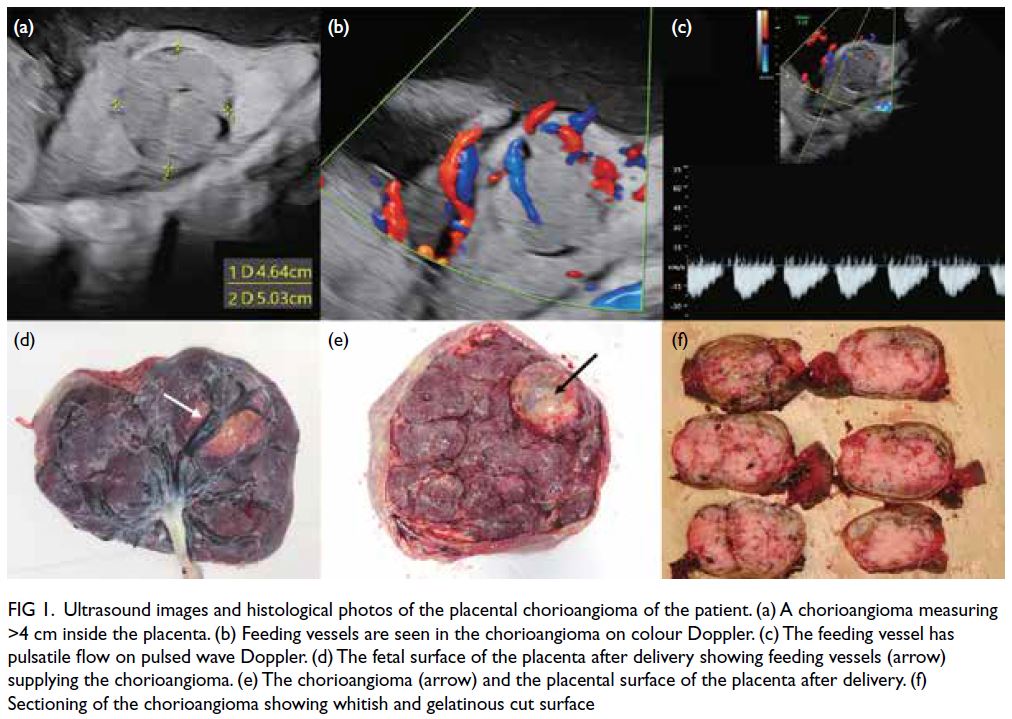
Figure 1. Ultrasound images and histological photos of the placental chorioangioma of the patient. (a) A chorioangioma measuring >4 cm inside the placenta. (b) Feeding vessels are seen in the chorioangioma on colour Doppler. (c) The feeding vessel has pulsatile flow on pulsed wave Doppler. (d) The fetal surface of the placenta after delivery showing feeding vessels (arrow) supplying the chorioangioma. (e) The chorioangioma (arrow) and the placental surface of the placenta after delivery. (f) Sectioning of the chorioangioma showing whitish and gelatinous cut surface
In view of the severe maternal pressure
symptoms with shortness of breath, amnioreduction
was performed at 31 weeks of gestation under aseptic technique with continuous ultrasound guidance
using a 22-gauge spinal needle connected to low-pressure
wall suction. A total of 2280-mL amniotic
fluid was drained over 3 hours with post-procedure
AFI reduced to 16 cm. In view of the potential risk
of preterm labour, a course of betamethasone (12 mg
every 24 hours for two doses) was administered
intramuscularly prior to amnioreduction to enhance
fetal lung maturity. Results of chromosomal
microarray studies of the amniotic fluid were normal.
One week later, the polyhydramnios recurred with
AFI measuring 40 cm. Amnioreduction was repeated
at 32 weeks of gestation with 2600-mL amniotic
fluid drained over 2.5 hours and AFI reduced to 18
cm. Prophylactic antibiotics were not given prior to
either procedure.
Three days after amnioreduction, the
patient developed signs of sepsis with fever, fetal
tachycardia, and abdominal tenderness. Maternal
white cell count and C-reactive protein level were
elevated. The clinical picture was compatible with acute chorioamnionitis and intravenous antibiotics
were commenced. Emergency caesarean section was
performed and a baby weighing 2080 g was born
with good Apgar score. Septic workup including
blood culture, high vaginal swabs, amniotic fluid and
placental swabs did not yield any bacterial growth.
Both the mother and the baby subsequently recovered
well. Histological examination of the placenta
confirmed the diagnosis of chorioangioma (Fig 2).
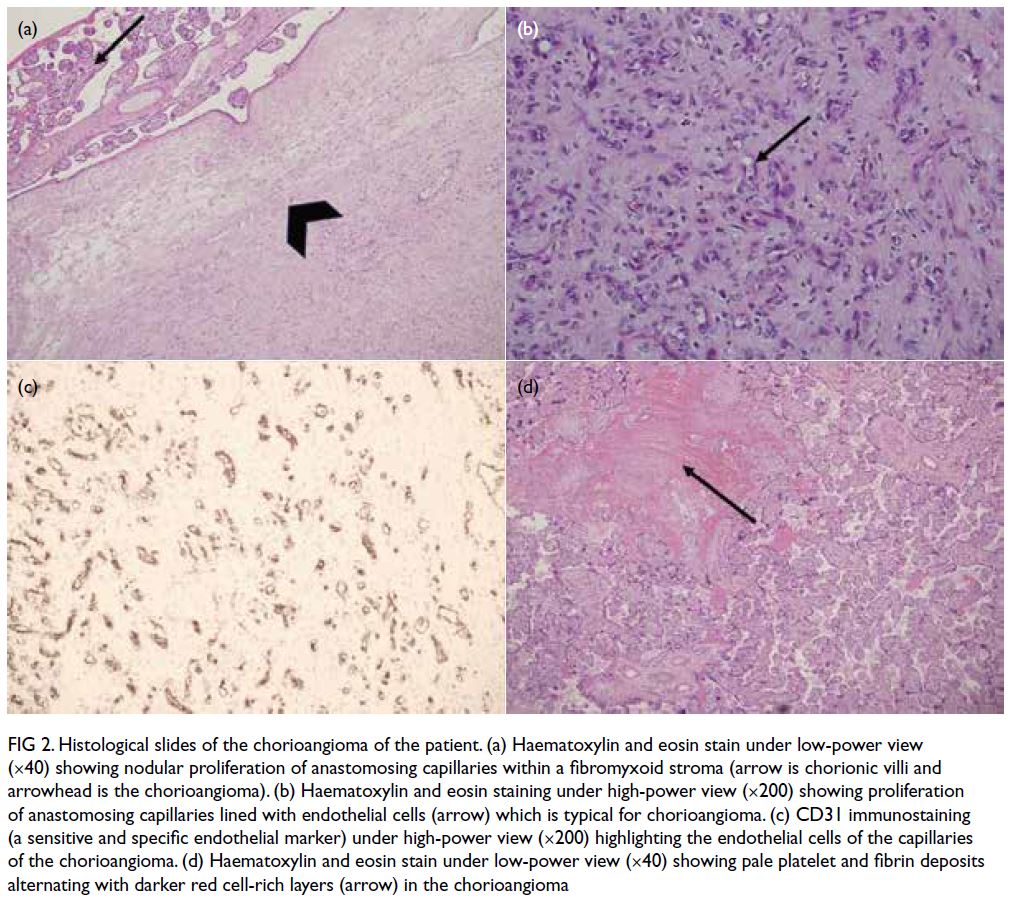
Figure 2. Histological slides of the chorioangioma of the patient. (a) Haematoxylin and eosin stain under low-power view (×40) showing nodular proliferation of anastomosing capillaries within a fibromyxoid stroma (arrow is chorionic villi and arrowhead is the chorioangioma). (b) Haematoxylin and eosin staining under high-power view (×200) showing proliferation of anastomosing capillaries lined with endothelial cells (arrow) which is typical for chorioangioma. (c) CD31 immunostaining (a sensitive and specific endothelial marker) under high-power view (×200) highlighting the endothelial cells of the capillaries of the chorioangioma. (d) Haematoxylin and eosin stain under low-power view (×40) showing pale platelet and fibrin deposits alternating with darker red cell-rich layers (arrow) in the chorioangioma
Discussion
There are numerous causes for polyhydramnios in
singleton pregnancies including gestational diabetes,
chromosomal abnormalities, fetal structural
abnormalities such as bowel atresia, and placental
causes such as chorioangioma. As mild gestational
diabetes should not lead to severe polyhydramnios,
the most likely primary diagnosis in our patient
was chorioangioma. The pathophysiology of
polyhydramnios in placental chorioangioma is not completely known. One of the proposed mechanisms
is transudation of fluid from the surface of the
chorioangioma adjacent to the placental surface. The
incidence of placental chorioangioma is estimated to
be around 1%. As chorioangiomas >4 cm can lead to
complications including polyhydramnios, preterm
delivery, intrauterine growth restriction, hydrops
fetalis and even fetal demise, close ultrasound
surveillance, intrauterine interventions or even
early delivery may be necessary.1 Careful ultrasound
examination of the placenta is warranted for all cases
of gross polyhydramnios.
Amnioreduction has been commonly
performed to relieve polyhydramnios in both
singleton and multiple pregnancies. Traditionally,
amniodrainage would be performed using an 18-to 22-gauge spinal needle with the amniotic fluid
removed manually using a three-way tap and 50-mL
syringe. The use of wall suction and a vacuum bottle
aspiration system connected to a needle has been
proposed in recent years to speed up the procedure
and reduce operator fatigue.2
Different complications including preterm
labour, prelabour rupture of membranes and
placental abruption have been reported following
amnioreduction. There is no consensus or guideline
for the most appropriate size of needle or the rate
at which amniotic fluid can be safely removed.
Rapid drainage using an 18- or 20-gauge needle
connected to the vacuum system with the fastest rate
of drainage up to 178 mL/min has been advocated
by Leung et al2 since 2004. The overall complication
rate for this rapid drainage, including placental
abruption, prelabour rupture of membranes and fetal
bradycardia in singleton and multiple pregnancies,
was 3.1%.2 Placental abruption has been reported
following amnioreduction for polyhydramnios
specifically caused by chorioangioma. One patient
has been reported in whom two episodes of
amnioreduction were performed a few days apart
using an 18-gauge needle connected to a vacuum
system.3 With an average drainage rate of 100 mL/min,
2500 mL and 2700 mL of amniotic fluid was removed.
Placental abruption occurred 12 hours after the
second amnioreduction. The authors concluded
that caution should be exercised when performing
large-volume or rapid amnioreductions in idiopathic
or chorioangioma-associated polyhydramnios.3 We
used a small needle (22-gauge) to drain the amniotic
fluid slowly at a rate of 12.7 mL/min in our first
amnioreduction and 17.3 mL/min in the second
amnioreduction in an attempt to lower the risk of
placental abruption and preterm prelabour rupture
of membranes.
Erfani et al4 recently evaluated the
complications following amnioreduction in
singleton pregnancies without other interventions
by combining their findings with those of six other studies. The incidence of preterm labour
was 50.5% (48/95) and that of placental abruption
was 1.3% (4/315), although there was no acute
chorioamnionitis in a total of 244 patients.4 This
implies that the role of prophylactic antibiotics is
dubious. Nonetheless not all studies specified the
duration of the amnioreductions. Only one case of
acute chorioamnionitis following amnioreduction
has been reported.5 That patient had a twin
pregnancy with polyhydramnios not caused by
twin-twin transfusion syndrome. Amnioreduction
was performed at 31 weeks of gestation using an 18-gauge needle with a total of 1950-mL amniotic fluid
removed at a rate of 65 mL/min. She developed acute
chorioamnionitis 18 hours following the procedure.5
Although it is logical to deduce that the risk of
chorioamnionitis will increase with the length of
procedure for amnioreduction, there are no relevant
studies available in the literature to support this
association due to the rarity of this complication.
As far as we are aware, this is the second case
reported in the literature of acute chorioamnionitis
following amnioreduction. As caesarean section was
performed immediately under antibiotic cover when
the patient developed signs of sepsis, the septic
workup did not yield any bacterial growth.
It is crucial to maintain a high index of
suspicion and search for placental chorioangioma
in a fetus where there is no obvious cause for
polyhydramnios to ensure prompt diagnosis and
proper management. Amnioreduction carries risks
of complications, including placental abruption
and acute chorioamnionitis, and the optimal rate of
drainage remains controversial.
Author contributions
Concept or design: JTC Leung, CW Kong.
Acquisition of data: JTC Leung.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: JTC Leung, CW Kong.
Critical revision of the manuscript for important intellectual content: WWK To, CW Kong.
Acquisition of data: JTC Leung.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: JTC Leung, CW Kong.
Critical revision of the manuscript for important intellectual content: WWK To, CW Kong.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank Dr CL Ho from the Department of Pathology of United Christian Hospital for the histological slides of the chorioangioma of the patient.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of
Helsinki. Written consent was obtained from the patient for
publication of this article and the accompanying images.
References
1. Buca D, Iacovella C, Khalil A, et al. Perinatal outcome of
pregnancies complicated by placental chorioangioma:
systematic review and meta-analysis. Ultrasound Obstet
Gynecol 2020;55:441-9. Crossref
2. Leung WC, Jouannic JM, Hyett J, Rodeck C, Jauniaux E.
Procedure-related complications of rapid amniodrainage in the treatment of polyhydramnios. Ultrasound Obstet
Gynecol 2004;23:154-8. Crossref
3. Kim A, Economidis MA, Stohl HE. Placental abruption
after amnioreduction for polyhydramnios caused by
chorioangioma. BMJ Case Rep 2018;2018:bcr2017222399. Crossref
4. Erfani H, Diaz-Rodriguez GE, Aalipour S, et al.
Amnioreduction in cases of polyhydramnios: indications
and outcomes in singleton pregnancies without fetal
interventions. Eur J Obstet Gynecol Reprod Biol
2019;241:126-8. Crossref
5. Elliott JP, Sawyer AT, Radin TG, Strong RE. Large-volume
therapeutic amniocentesis in the treatment of hydramnios.
Obstet Gynecol 1994;84:1025-7.

