Hong Kong Med J 2024 Feb;30(1):66–8 | Epub 8 Jan 2024
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Common carotid artery pseudoaneurysm secondary to erosion by an oesophageal stent: a case report
SC Tam, FRCSEd, FHKAM (Surgery); Albert CW Ting, MS, FRCS; Stephen WK Cheng, MS, FRCSEd
Department of Surgery, Queen Mary Hospital, Hong Kong SAR, China
Corresponding author: Dr SC Tam (tsc587@ha.org.hk)
Case presentation
A 59-year-old woman had inoperable carcinoma
of the upper oesophagus and had undergone
chemoradiotherapy and immunotherapy. A covered
oesophageal stent (Niti-S, 20 mm in diameter,
80 mm in length; Taewoong Medical, South
Korea) was inserted in August 2021 to manage a
tracheoesophageal fistula. The proximal end of the
stent was located just distal to the cricopharyngeal
constriction. Five months after stent placement,
the patient developed erosions at the proximal and
distal ends of the stent into the trachea and bronchi,
respectively. A covered tracheal stent (AERO, 18
mm in diameter, 40 mm in length; Merit Medical,
South Jordan [UT], US) and a distal extension with a
covered oesophageal stent (Niti-S) were inserted on
two separate occasions.
The patient presented to the emergency
department 7 months after initial oesophageal stent
insertion with haemoptysis. Her haemoglobin level
had fallen to 6.3 g/dL and she developed hypotension
and desaturation requiring intubation and admission
to the intensive care unit. Upper endoscopy revealed
blood clots over the proximal part of the oesophagus but no active bleeding following clot removal.
Computed tomography showed no contrast
extravasation. The upper end of the oesophageal
stent was close to the left common carotid artery. A
small suspicious outpouching of the artery was also
seen at that location (Fig 1a and 1b).
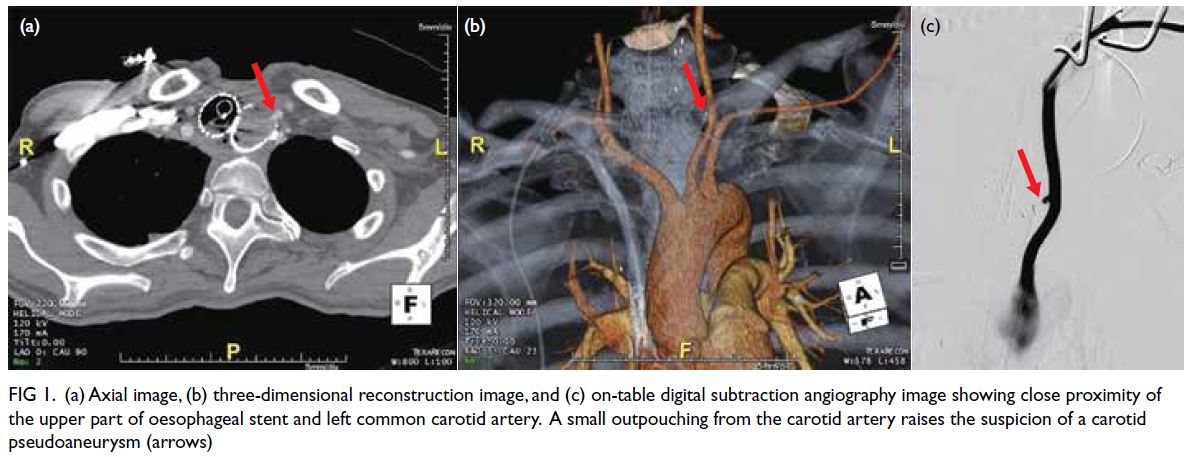
Figure 1. (a) Axial image, (b) three-dimensional reconstruction image, and (c) on-table digital subtraction angiography image showing close proximity of the upper part of oesophageal stent and left common carotid artery. A small outpouching from the carotid artery raises the suspicion of a carotid pseudoaneurysm (red arrows)
Surgery was performed under general
anaesthesia via a left neck incision. Retrograde
puncture of the left common carotid artery was
performed and an 8-Fr vascular sheath (AVANTI+;
Cordis, Miami Lakes [FL], US) was placed.
Digital subtraction angiogram revealed a small
pseudoaneurysm confirming our clinical suspicion
(Fig 1c). Oesophageal stent erosion was suspected
to be the cause due to its proximity. Complete
exclusion of the pseudoaneurysm was achieved (Fig 2) using a covered vascular stent (Covera Plus, 8 mm
in diameter, 60 mm in length; Becton, Dickinson and
Company, Franklin Lakes [NJ], US).
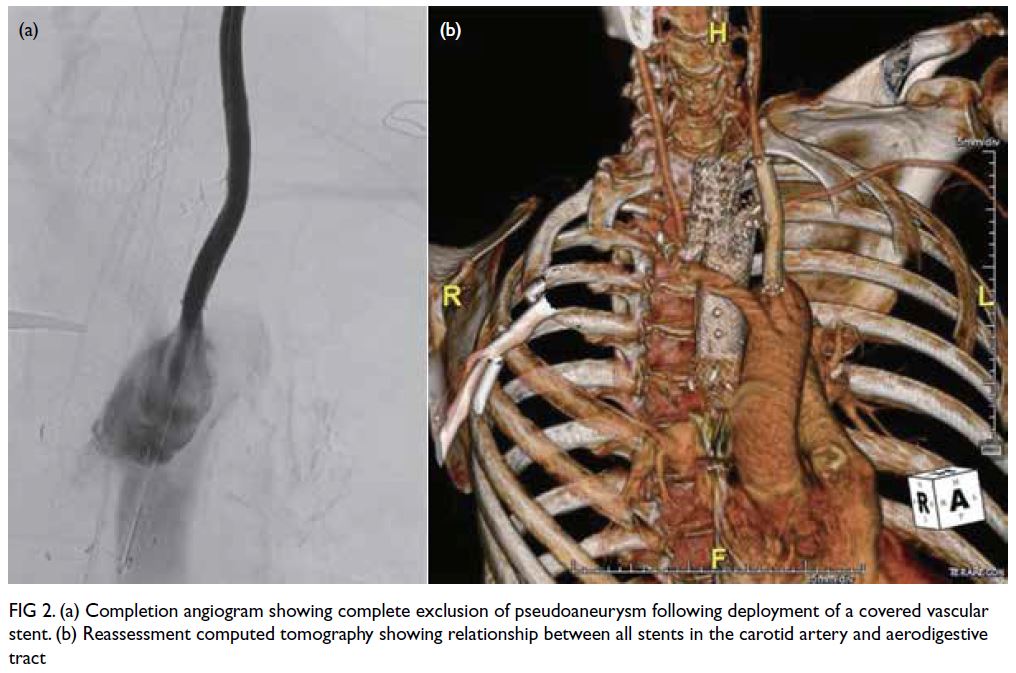
Figure 2. (a) Completion angiogram showing complete exclusion of pseudoaneurysm following deployment of a covered vascular stent. (b) Reassessment computed tomography showing relationship between all stents in the carotid artery and aerodigestive tract
Postoperatively, the patient’s condition
improved with no rebleeding. She refused further
surgery to repair the fistula via a manubrial
resection. Further covered tracheal stenting
(Dumon Y, 15 mm in diameter; Boston Medical Products Inc, Shrewsbury [MA], US) was performed
to exclude residual tracheoesophageal fistula and
prevent aspiration pneumonia. The patient was
prescribed long-term moxifloxacin because of the
potential communication with the aerodigestive
tract and contamination. She was well 6 weeks
later. Reassessment computed tomography showed
a patent carotid stent with no features of stent
infection and no residual pseudoaneurysm.
Discussion
Upper gastrointestinal bleeding is a frequent
presentation following oesophageal stenting.
Endoscopy has both diagnostic and therapeutic roles
in common bleeding pathologies such as tumour
and peptic ulcer. The presence of a stent often makes
identification of a bleeding site difficult. Diagnosing
fistulation with major arteries requires a high level
of suspicion, especially if the bleeding is extensive.
Although it is tempting to remove a blood clot
during endoscopy, care should be exercised to avoid
rupture of any underlying pseudoaneurysm with
consequent torrential bleeding. Endoscopic biopsy
of tissue around the oesophageal stent can also lead
to pseudoaneurysm rupture as reported in an early
case report by Kohl et al.1
Computed tomography is often useful to show
the site of bleeding and corresponding anatomical
relationship. Nonetheless a negative imaging may provide false reassurance. The pseudoaneurysm may
be small because of impingement by the pointed
oesophageal stent struts. This can be missed if the
slice thickness of scan is not thin enough. Three-dimensional
reconstruction images may provide
more information. An on-table angiogram should be
considered when the diagnosis is in doubt.
Fistulation of the carotid artery by a metallic
oesophageal stent is rare and was first reported in
2001.1 Four previously reported cases were found
in the literature.1 2 3 4 Among these cases, three adult
patients had complications of previous treatments
for carcinoma in the head and neck region, where
two had oesophageal stricture1 3 and one had a
tracheoesophageal fistula2; another 4-year-old
paediatric patient had an oesophageal stent inserted
for anastomotic stricture following surgical repair of
oesophageal atresia.4
In Kohl et al’s report,1 resection was
performed with a bypass using homograft made
from the ascending aorta to the carotid bifurcation.
Asymptomatic blockage of the graft was found soon
after the procedure. The patient died of rebleeding 2
months later. Ali et al2 used endovascular coiling of
pseudoaneurysm and stenting with a self-expandable
nitinol stent. The patient had a rebleed 2 weeks later
that required placement of a covered vascular stent.
Staged open ligation of the common carotid artery
was performed as a definitive treatment.2
A complete endovascular approach has been
reported more recently. One patient received
stenting to control bleeding and a staged operation to
sacrifice the common carotid artery by endovascular
coiling, but the long-term outcome was not
reported.3 The paediatric patient was successfully
treated with repeated coiling of the pseudoaneurysm
and stenting with a bare-metal stent. He remained
asymptomatic at a follow-up 1 year later.4
Endovascular treatment acted as a bridge
to definitive management if quick open access is
difficult due to anatomical constraints, as in our
patient. Balloon occlusion test and cerebral perfusion
scan can confirm adequate collateral supply before
carrying out a second-stage operation to sacrifice
the common carotid artery.2 3
The two major concerns with this temporising
treatment are the risks of rebleeding and endograft
infection. Definitive management should include
surgical separation of the fistula. The oesophageal
defect can be repaired primarily with or without
reinforcement using diaphragm, intercostal muscle,
serratus muscle, or omentum. Oesophagectomy or
diversion are the other options if primary repair is
not possible.
The diseased artery can be too friable for primary
repair. Open ligation and endovascular coiling of
the proximal carotid artery can be considered to
prevent rebleeding provided an adequate collateral
supply to the brain is confirmed.2 3 Revascularisation
can be performed if required using bypass grafts
from the aorta or subclavian artery. Operative risks
include stroke, graft thrombosis and graft infection,
especially when the surgical field is contaminated.
Similar fistulation between an aberrant
right subclavian artery and oesophagus has been
reported following oesophageal stent placement due
to the anatomical relationship. Experience shows
that most cases required immediate open surgery
followed by tamponade using a hydrostatic dilator
or Sengstaken–Blakemore tube. Surgery can be
performed via a median sternotomy, thoracotomy or
a manubrial resection. In patients with endovascular
stenting as a temporising measure, the stent should
be removed at the time of surgery to prevent
oesophageal pressure necrosis due to a ‘sandwich
effect’ with the oesophageal stent.5
For patients in whom definitive treatment is not possible, removal of an oesophageal stent
can promote fistula healing. Proximal extension
of a covered oesophageal stent may also minimise
contamination from the aerodigestive tract. Long-term
prophylactic antibiotics should be given but
efficacy is not guaranteed. Alternatively, sacrificing
unilateral carotid artery via an endovascular
technique such as coils or plugs may prevent
rebleeding. There is nonetheless no long-term
evidence to support this technique.
Author contributions
All authors contributed to the concept or design of the study,
acquisition of the data, analysis or interpretation of the
data, drafting of the manuscript, and critical revision of the
manuscript for important intellectual content. All authors
had full access to the data, contributed to the study, approved
the final version for publication, and take responsibility for its
accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of
Helsinki and provided written informed consent for all treatment
and procedures and for publication of this case report.
References
1. Kohl O, Rauber K, Doppl W. Perforation of an esophageal stent into the common carotid artery. Gastrointest Endosc 2001;53:374-8. Crossref
2. Ali AT, Kokoska MS, Erdem E, Eidt JF. Esophageal stent
erosion into the common carotid artery. Vasc Endovascular
Surg 2007;41:80-2. Crossref
3. Yadam S, Rali P, Balaan M, Lega M. A case of carotid-esophageal fistula masquerading as an upper gastrointestinal bleed. Am J Respir Crit Care Med 2016;194:e2-3. Crossref
4. Fachin CG, Demartini Z Jr, Pinto AS, et al. Carotidesophageal
fistula treated by endovascular approach. Vasc
Endovascular Surg 2021;55:419-21. Crossref
5. Merlo A, Farber M, Ohana E, Pascarella L, Crowner J,
Long J. Aberrant right subclavian artery to esophageal
fistula: a rare case and its management. Ann Thorac Surg 2020;110:e85-6. Crossref

