Hong Kong Med J 2023 Dec;29(6):556 | Epub 21 Nov 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Non-ketotic hyperglycaemic hemichorea: a rare complication of uncontrolled diabetes mellitus
PL Lam, MB, BS; PP Iu, FRCR, FHKAM (Radiology); Danny HY Cho, FRCR, FHKAM (Radiology)
Department of Diagnostic and Interventional Radiology, Kwong Wah Hospital, Hong Kong SAR, China
Corresponding author: Dr PL Lam (lpl404@ha.org.hk)
Case 1
A 65-year-old man with a 1-month history of left
upper and lower limb chorea was admitted to the
medical ward of our institution in February 2021.
Blood tests revealed new-onset diabetes mellitus
with markedly elevated fasting glucose level of
28.5 mmol/L. Urinalysis for ketones was negative.
Urgent non-contrast computed tomography (CT)
of the brain showed subtle hyperdensity at the right
putamen without mass effect or surrounding oedema
(Fig 1). The patient was started on subcutaneous
insulin, and upon normalisation of blood glucose
level, his hemichorea subsided without additional
antichorea medications. Follow-up non-contrast
magnetic resonance imaging of the brain performed
2 months later revealed T1-weighted hyperintensity
in the right putamen, without restricted diffusion
(Fig 2). Imaging findings were in keeping with non-ketotic
hyperglycaemic hemichorea (NHH). The
patient was prescribed a biphasic insulin regimen
upon discharge.
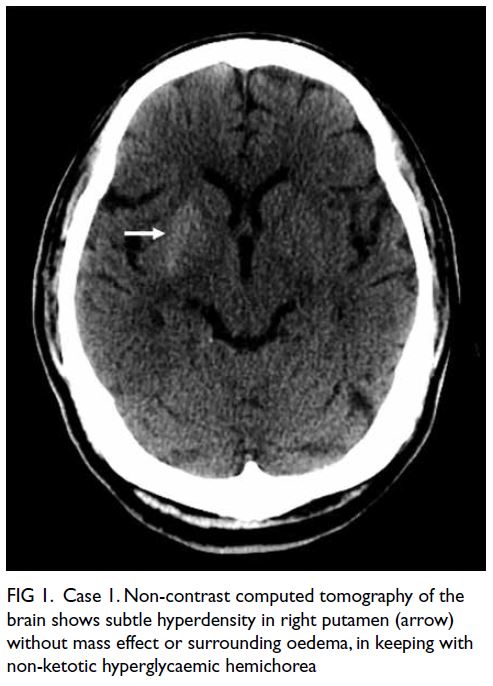
Figure 1. Case 1. Non-contrast computed tomography of the brain shows subtle hyperdensity in right putamen (arrow) without mass effect or surrounding oedema, in keeping with non-ketotic hyperglycaemic hemichorea
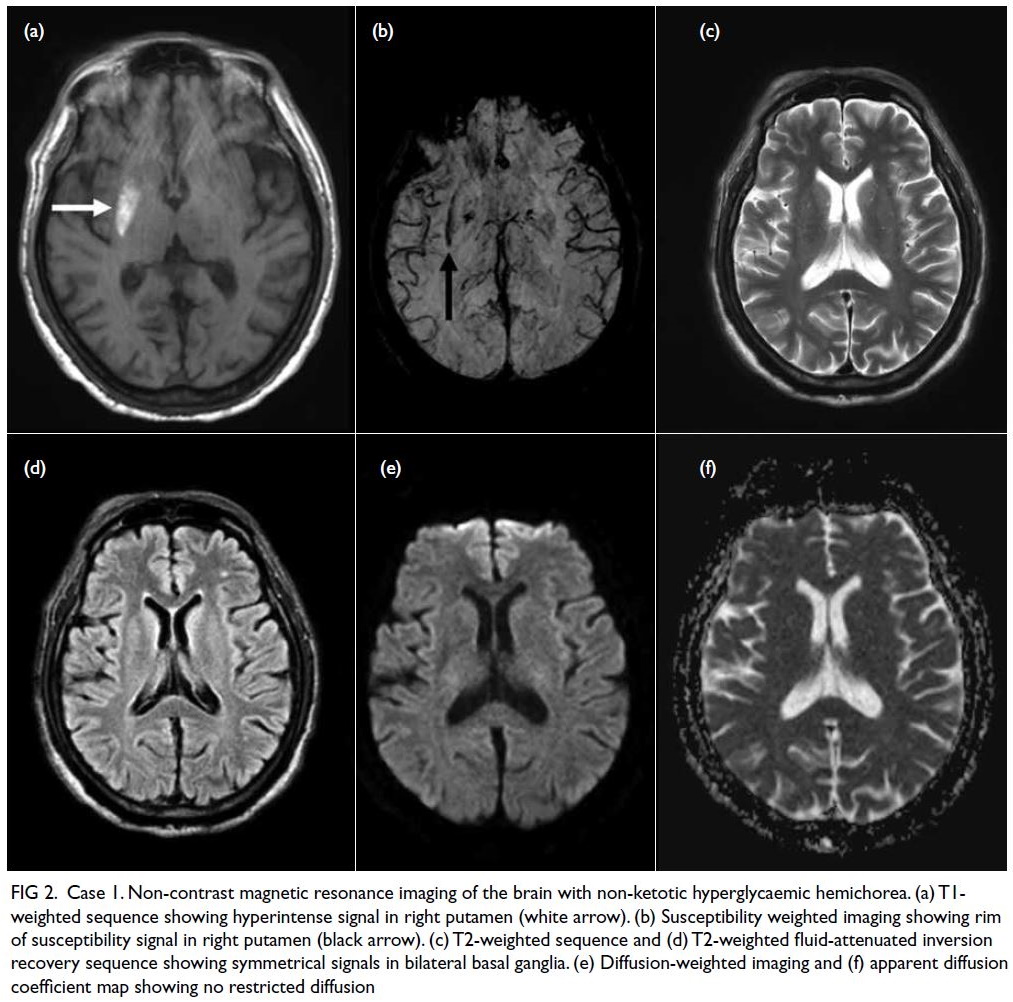
Figure 2. Case 1. Non-contrast magnetic resonance imaging of the brain with non-ketotic hyperglycaemic hemichorea. (a) T1-weighted sequence showing hyperintense signal in right putamen (white arrow). (b) Susceptibility weighted imaging showing rim of susceptibility signal in right putamen (black arrow). (c) T2-weighted sequence and (d) T2-weighted fluid-attenuated inversion recovery sequence showing symmetrical signals in bilateral basal ganglia. (e) Diffusion-weighted imaging and (f) apparent diffusion coefficient map showing no restricted diffusion
Case 2
An 87-year-old man with a 2-day history of left
upper limb chorea was hospitalised in April 2022. He
had known diabetes mellitus but was noncompliant
with oral hypoglycaemic therapy. Blood tests
revealed markedly elevated random glucose level of
30.8 mmol/L. Urgent non-contrast CT of the brain
showed asymmetric subtle hyperdensity in bilateral
putamen and caudate nuclei, more extensive on
the right, but without mass effect or surrounding
oedema (Fig 3). Findings were compatible with NHH.
The patient resumed metformin, with gliclazide and
subcutaneous insulin injection added for optimal
control. Upon normalisation of blood glucose
level, his hemichorea resolved without antichorea
medications.

Figure 3. Case 2. Non-contrast computed tomography of the brain showing asymmetric subtle hyperdensity in bilateral putamen (a) [arrows] and bilateral caudate nuclei (b) [arrowheads], more extensive on the right, without mass effect or surrounding oedema, in keeping with non-ketotic hyperglycaemic hemichorea
Discussion
Unilateral or asymmetric basal ganglia hyperdensity
in brain CT of patients with focal neurological
symptoms can be alarming, and intracerebral
haemorrhage may be suspected. Nonetheless NHH,
a rare complication of uncontrolled diabetes, should
not be overlooked.
Case reports of NHH have been documented
as early as 1960.1 Previously reported cases were
frequent in Asian elderly women with uncontrolled
diabetes. In most patients, unilateral chorea was
observed, although bilateral involvement could
be present.2 3 4 Of note, the aetiology of hemichorea
is diverse, and other causes include infarct,
haemorrhage and neoplasm. Imaging of the brain is
therefore crucial.
Non-contrast CT of the brain of NHH
typically shows subtle hyperdensity in contralateral
putamen and/or caudate nucleus, although bilateral
involvement is also seen. There will be no mass effect
or perilesional oedema, and this differentiates NHH
from haemorrhage or tumour.2 3 4
Similarly, magnetic resonance imaging of the
brain typically shows corresponding signal changes
in striatal regions contralateral to the symptomatic
side. There will be T1-weighted hyperintense signal.
Differentials of increased basal ganglia T1-weighted
signal are diverse. They include toxin-related causes
such as methanol poisoning or hepatic-related causes
such as acquired hepatocerebral degeneration, but
they commonly show bilateral and symmetrical
involvement.5 T2-weighted or fluid-attenuated inversion recovery signals can be variable. Of note,
restricted diffusion is not expected in NHH,2 3 4 and
this differentiates it from acute ischaemic stroke.
The pathophysiology of NHH is not fully
understood. Proposed mechanisms include depleted
gamma-aminobutyric acid and disrupted blood-brain
barrier at the corpus striatum.2 3 4 Recognising this
rare complication of uncontrolled diabetes mellitus
enables prompt medical intervention. Neurological
symptoms of NHH usually show substantial
improvement after normalisation of blood glucose
level without additional intervention.2 3 4
Author contributions
All authors contributed to the concept and design of the
study, acquisition of data, analysis and interpretation of
data, drafting of the manuscript, and critical revision of the
manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved
the final version for publication, and take responsibility for its
accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patients were treated in accordance with the Declaration
of Helsinki. They provided informed consent for all treatments
and procedures, and consent for publication.
References
1. Bedwell SF. Some observations on hemiballismus.
Neurology 1960;10:619-22. Crossref
2. Zheng W, Chen L, Chen JH, et al. Hemichorea associated
with non-ketotic hyperglycemia: a case report and
literature review. Front Neurol 2020;11:96. Crossref
3. Narayanan S. Hyperglycemia-induced hemiballismus
hemichorea: a case report and brief review of the literature.
J Emerg Med 2012;43:442-4. Crossref
4. Cherian A, Thomas B, Baheti NN, Chemmanam T,
Kesavadas C. Concepts and controversies in nonketotic
hyperglycemia-induced hemichorea: further evidence
from susceptibility-weighted MR imaging. J Magn Reson
Imaging 2009;29:699-703. Crossref
5. Hegde AN, Mohan S, Lath N, Lim CC. Differential
diagnosis for bilateral abnormalities of the basal ganglia
and thalamus. Radiographics 2011;31:5-30. Crossref

