Hong Kong Med J 2023 Dec;29(6):489–97 | Epub 19 Dec 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Moral distress and psychological status among healthcare workers in a newly established paediatric intensive care unit
WL Cheung, MB, BS, MRCPCH1; KL Hon, MB, BS, MD1; Karen KY Leung, MB, BS, MRCPCH1; WF Hui, MB, ChB, MRCPCH1; Judith JM Wong, MBBChBAO, MRCPCH2; JH Lee, MB, BS, MRCPCH2; SC Kwok, BNur3; Patrick Ip, MB, BS, MD4
1 Department of Paediatrics and Adolescent Medicine, Hong Kong Children’s Hospital, Hong Kong SAR, China
2 Children’s Intensive Care Unit, Department of Paediatric Subspecialties, KK Women’s and Children’s Hospital, Singapore
3 Nursing Services Division, Hong Kong Children’s Hospital, Hong Kong SAR, China
4 Department of Paediatrics and Adolescent Medicine, The University of Hong Kong, Hong Kong SAR, China
Corresponding author: Dr KL Hon (ehon@hotmail.com)
Abstract
Introduction: Healthcare workers in intensive care
units often experience moral distress, depression,
and stress-related symptoms. These conditions
can lower staff retention and influence the quality
of patient care. This study aimed to evaluate the
prevalence of moral distress and psychological status
among healthcare workers in a newly established
paediatric intensive care unit (PICU) in Hong Kong.
Methods: A cross-sectional questionnaire survey
was conducted in the PICU of the Hong Kong
Children’s Hospital; healthcare workers (doctors,
nurses and allied health professionals) were invited
to participate. The Revised Moral Distress Scale
(MDS-R) Paediatric Version and Depression
Anxiety and Stress Scale–21 items were used to
assess moral distress and psychological status,
respectively. Demographic characteristics were
examined in relation to moral distress, depression,
anxiety, and stress scores to identify risk factors for
poor psychological outcomes. Correlations of moral
distress with depression, anxiety, and stress were
examined.
Results: Forty-six healthcare workers completed
the survey. The overall median MDS-R moral
distress score was 71. Nurses had a significantly
higher median moral distress score, compared with
doctors and allied health professionals (102 vs 47 vs
20). Nurses also had the highest median anxiety and
stress scores (11 and 20, respectively). Moral distress scores were correlated with depression (r=0.445;
P=0.002) and anxiety scores (r=0.417; P<0.05).
Healthcare workers intending to quit their jobs had
significantly higher moral distress scores (P<0.05).
Conclusions: Among PICU healthcare workers,
nurses had the highest level of moral distress. Moral
distress was associated with greater depression,
anxiety, and intention to quit. Healthcare workers
need support and a sustainable working environment
to cope with moral distress.
New knowledge added by this study
- Among paediatric intensive care unit healthcare workers, nurses had the highest moral distress scores.
- Moral distress was associated with greater depression, anxiety, and intention to quit.
- Healthcare workers need support and a sustainable working environment to cope with moral distress.
- Considering the high levels of moral distress experienced by nurses as well as the substantial moral distress in relation to end-of-life care, coping strategies should target nurses and focus on end-of-life education.
Introduction
Paediatric intensive care units (PICUs) are highly
specialised workplaces that support children with
critical illnesses and their caregivers. Advances in
paediatric critical care have significantly improved
survival among critically ill children, although this
improvement has also led to higher rates of morbidity,
more disabilities, and longer hospital stays.1 2 3 4 5 These changes have resulted in potentially conflicting views
regarding expectations and treatment goals among
healthcare workers and patients’ families, increasing
the incidence of moral distress among healthcare
workers.6
Moral distress is a term that refers to
experiences of frustration and failure arising from
healthcare workers’ attempts to fulfil their moral obligations to patients, families, and the public.7 8
In an intensive care setting, healthcare workers
frequently encounter ethical issues. Moral distress
arises when a healthcare worker has determined
the right course of action but cannot follow it
because of internal or external constraints (eg,
limited resources, institutional policies, or family
preferences).9 Moral distress has been identified
among healthcare workers in both adult ICUs and
PICUs.10 11 It is associated with greater experience
and lower staff retention.12
Depression and stress-related symptoms
are common in healthcare workers, particularly
among ICU staff.13 14 Studies have shown that
these symptoms can ultimately impair patient care
quality.15 16 Thus far, most literature regarding moral
distress has been published in Western countries;
the concept of moral distress is not well-known
outside of the Western world.17 To our knowledge,
there have been few analyses of moral distress and
psychological status among healthcare workers in
non-Western PICUs. Factors that can influence
the level and type of moral distress include cultural
backgrounds; beliefs of the patient, their family, and
the clinical team; and differences among healthcare
systems. Hong Kong is a multicultural city influenced
by both Eastern and Western cultures; challenges in
this setting may be unique. This study assessed moral
distress prevalence and psychological status among
PICU healthcare workers in Hong Kong.
Methods
Study population and study design
This prospective single-centre cross-sectional study
was conducted from June to July 2020 in the six-bed
tertiary PICU of the Hong Kong Children’s Hospital
(HKCH), which began operation at the end of March
2019. The HKCH is the only dedicated paediatric
oncology centre in the region, and most PICU
admissions (54%) during the study period involved
patients with cancer.
Study participants were healthcare workers
involved in direct clinical care within the HKCH
PICU, including doctors, nurses, and allied health
professionals (ie, physiotherapists, occupational
therapists, speech therapists, pharmacists, and
dietitians). Healthcare workers were excluded if
they had <3 months of critical care experience in the
PICU or were temporarily on leave from the PICU
during the study period. The survey was distributed
to all eligible healthcare workers in the HKCH PICU
during working hours within the study period.
Data collection and outcome measurement
The survey included two validated instruments
(Revised Moral Distress Scale [MDS-R] Paediatric
Version and Depression Anxiety and Stress Scale–21
items [DASS-21]) to measure levels of moral stress,
depression, anxiety, and stress in all participants.18 19
The participants’ demographic details were
also collected. The survey explored job-quitting
intentions related to moral distress or other reasons.
It was piloted with two HKCH PICU staff members;
questions were refined based on feedback from them.
The final survey was paper-based. An email was
sent to all participants before study commencement
with information regarding the aim and details
of the study. The survey was distributed by hand,
and all copies were collected in a sealed box after
completion. To ensure anonymity, the survey did not
contain any identifiers.
Moral distress, the main outcome of the study,
was measured using the validated paediatric version
of the MDS-R (online supplementary Appendix 1).18
It consists of 21 items describing predetermined
potentially morally distressing situations. There are
five predetermined categories of situations: end-of-life
care and quality of life, poor communication,
staffing and material resources, hierarchies of
decision making, and witnessing unethical behaviour.
Each item on the MDS-R is scored according to the
frequency and intensity that a healthcare worker
experienced, using a Likert scale that ranges from 0 to
4. If a specific situation has never been experienced,
participants are asked to indicate how disturbing
the situation would be if they encountered it in their
workplace. The frequency and intensity scores are
then multiplied to produce an overall score for each item. The total moral distress score is the sum of
the 21 overall scores for each item, ranging from 0
to 336. The English version of this instrument was
used.
Psychological status was assessed using the
DASS-21 (online supplementary Appendix 2).19 It is
a set of three self-reporting subscales that measure
participants’ emotional states: depression, anxiety,
and stress. Each scale contains seven items for each
emotional state. Each item is scored on a four-point
Likert scale ranging from 0 (‘Did not apply to
me at all’) to 3 (‘Applied to me very much or most
of the time’). The total score for each emotional
state is the sum of the subscale scores multiplied
by 2. Depression, anxiety, or stress was considered
present if the relevant scores exceeded the normal
cut-off. The emotional state was categorised as mild,
moderate, severe, or extremely severe, based on
published cut-offs. The English and Chinese versions
of this instrument were used; both language versions
have been validated.19 20
Data analysis
Outcome measures were demographic data and the
levels of moral distress, depression, anxiety, and stress.
Data were expressed using median (interquartile
range [IQR]) for continuous variables and count
(percentage) for categorical variables. Results of
the MDS-R and DASS-21 were compared among
doctors, nurses, and allied health professionals using
the Chi squared test, Kruskal-Wallis test, or Cohen’s
d. Correlations between participant variables and
outcome measures were evaluated using Spearman’s
rank correlation coefficient. P values <0.05 were
considered statistically significant. Statistical analysis
was performed using SPSS (Windows version 26.0;
IBM Corp, Armonk [NY], United States).
Results
In total, 46 of 56 healthcare workers in the PICU
completed the survey; the response rate was 82%.
On one survey, the moral distress section was
incomplete; that survey was excluded from the
analysis of moral distress.
Demographic characteristics
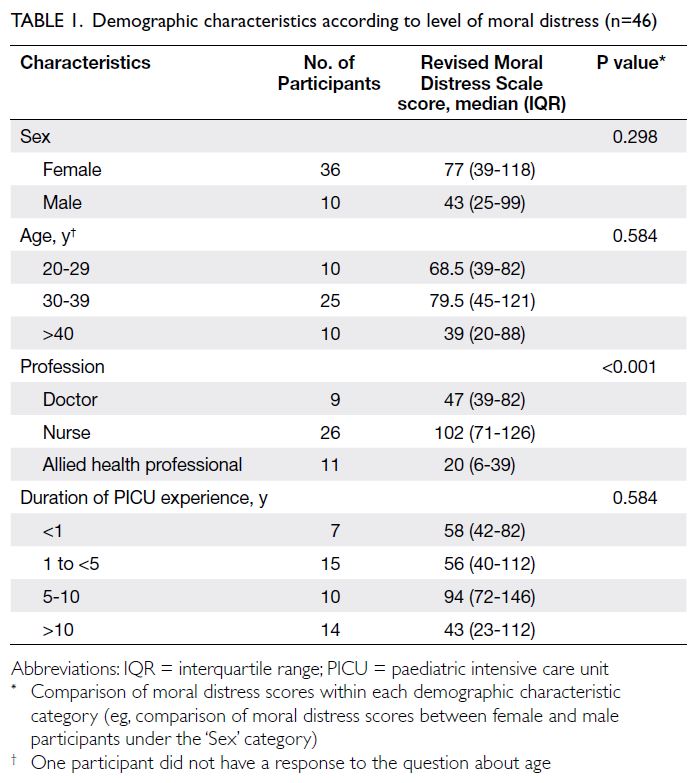
Most participants were women (n=36, 78%) and were aged ≥30 years (n=35, 76%). More than
half of the participants were nurses (n=26, 57%).
Approximately half of the participants (n=24,
52%) had >5 years of PICU experience. Detailed
participant characteristics are presented in Table 1.
Moral distress
The median MDS-R score was 71 (IQR=34-115). There was a significant difference in MDS-R score
among the three professions (P<0.001). Doctors and nurses had significantly higher MDS-R scores,
compared with allied health professionals (P<0.05).
Nurses had the highest median MDS-R score (102,
IQR=71-126), whereas allied health professionals
had the lowest (20, IQR=6-39). There were no
significant differences in MDS-R score according to
sex, age, or duration of PICU experience (Table 1).
Among the 21 items on the MDS-R, the most
morally distressing item was related to end-of-life
care and quality of life: ‘Honour the family’s wishes
to continue life support even though I believe it is
not in the child’s best interest’. This item also scored
highest in frequency and intensity among the 21
items. All three groups of health professionals
ranked this item as the most morally distressing
situation in the clinical setting. The second most
morally distressing item was also related to end-of-life
care and quality of life: ‘Initiate extensive life-saving
actions when I think they only prolong death’.
This item also consistently scored high in frequency
and intensity (Table 2). Situations involving poor
communication constituted the remaining three
most morally distressing items in this study. The top
five most morally distressing items, as well as the top
five items with the highest frequency and intensity,
are presented in Table 2.
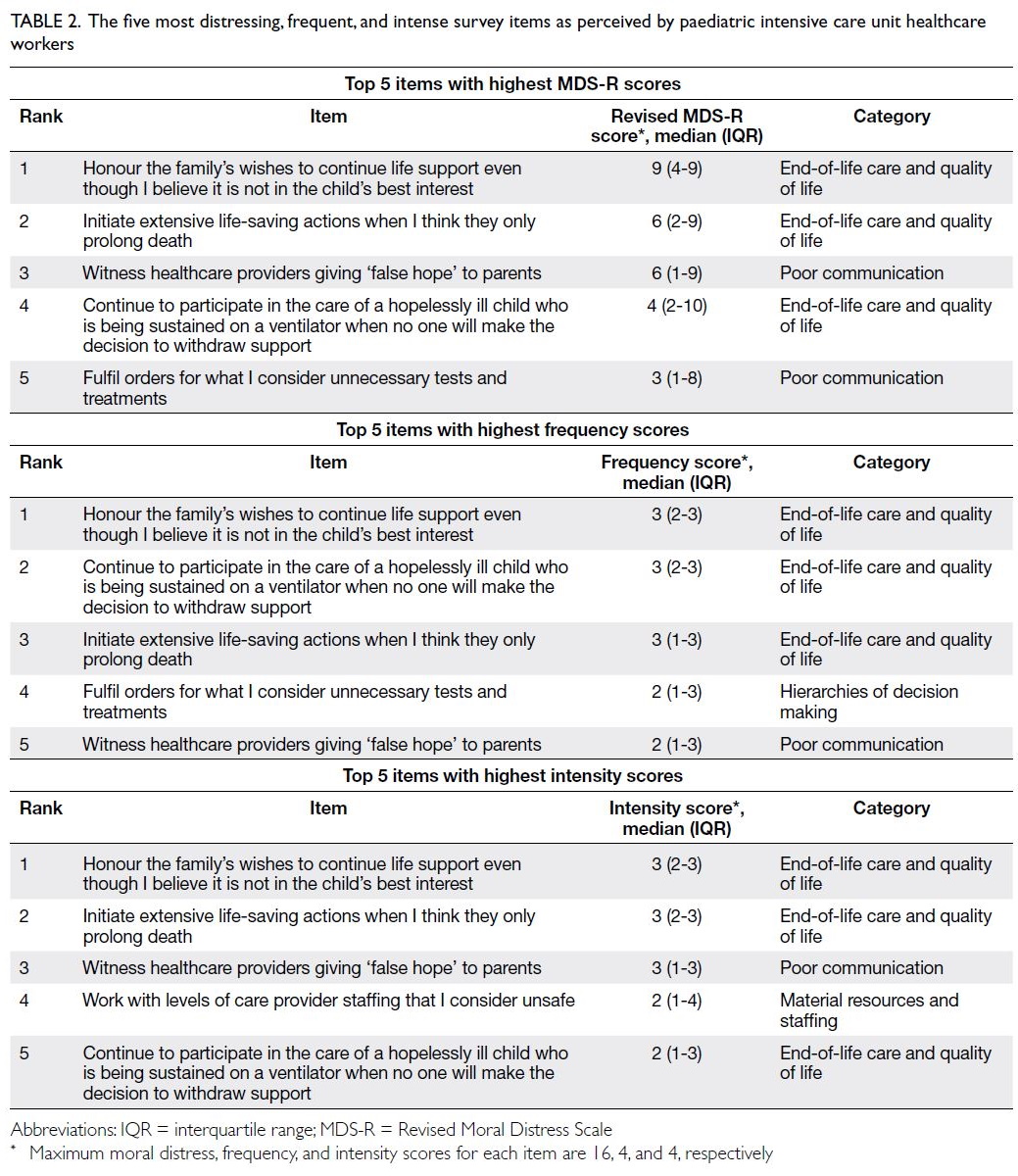
Table 2. The five most distressing, frequent, and intense survey items as perceived by paediatric intensive care unit healthcare workers
A higher MDS-R moral distress score was
associated with the intention to quit. Healthcare
workers who intended to quit their jobs had
significantly higher moral distress scores (P<0.05).
A higher moral distress score was also associated
with higher DASS-21 depression factor (r=0.445;
P<0.05) and anxiety factor scores (r=0.417; P<0.05).
Nurses who had worked for a greater number of
years in the PICU also experienced higher moral
distress (r=0.512; P<0.05). Twenty-eight percent
of all participants and 35% of nurses reported they
intended to quit their jobs because of moral distress.
Psychological status
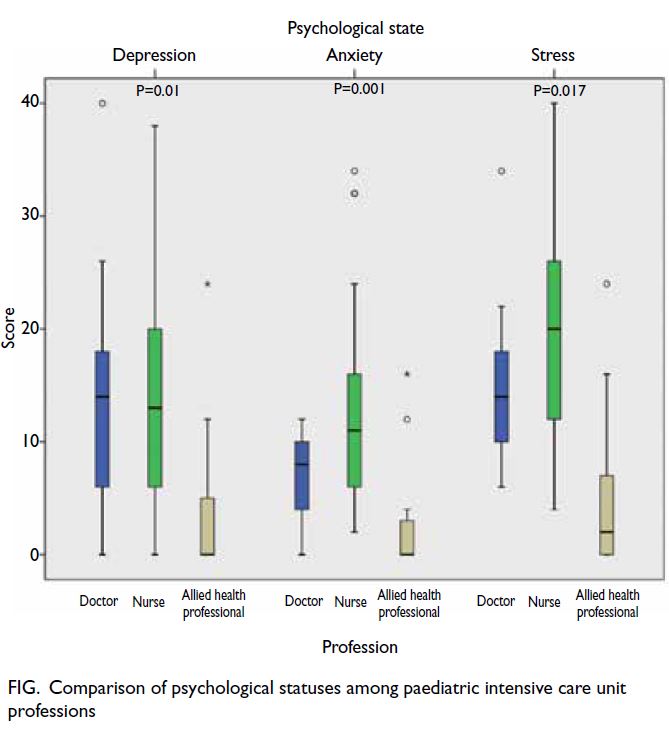
The median depression, anxiety, and stress scores
were 11 (IQR=0.5-18), 8 (IQR=3-145), and 30
(IQR=21-38), respectively; these scores corresponded
to mild depression, mild anxiety, and severe stress.
Among the three groups, nurses had the highest
median anxiety (11, IQR=6-16) and stress scores (20,
IQR=12-26) [Fig]; these scores corresponded to mild
depression, moderate anxiety, and moderate stress.
Participants with significantly higher depression
and anxiety (both P<0.05) scores also intended to
quit their jobs. There was no significant difference in stress score between participants who did and did
not intend to quit their jobs (P=0.434).
Discussion
Moral distress levels among various
healthcare workers
In this study, various levels of moral distress were
present in all three groups of PICU healthcare
workers. There was a significant difference in
MDS-R scores among the three professions, and
nurses had the highest median MDS-R score. This
finding is contrary to the results of previous PICU
studies, which showed that moral distress did
not differ among various healthcare workers.21 22
The literature suggests that nurses exhibit higher
moral distress scores because they often have less
autonomy concerning options in situations that
involve moral dilemmas, and they are required
to implement care plans with which they do not
agree.23 24 25 26 Studies of PICU healthcare workers’
behaviours in ethical and morally distressing
dilemmas have shown that 48% of PICU nurses
reported needing to perform actions that violated
their conscience. These results reflect the culture and
hierarchies of power in the PICU.23 26 27 Moreover,
nurses are the frontline workers who directly
experience the impacts of clinical decisions on
patients and their families.26 28 In newly established
PICUs, decreased self-confidence or increased fear
in a new working environment, combined with an
uncertain ethical climate, unclear team dynamics,
and less decision-making autonomy regarding
care plans, can cause nurses to perceive less moral
agency (ie, ability to act morally and change a
situation).22 24 25 26 29 30 31 A reduced sense of moral agency
can result in moral distress, which may be more
apparent in newly established PICUs.29 31
Our nurses’ moral distress levels among
published studies
We note that moral distress scores among nurses
in the present study are among the highest in
published studies of PICU healthcare workers (Table 3). In addition to the aforementioned lack of clarity in working environment and team dynamics, the
diverse levels of experience among nurses might
have also contributed to their high moral distress
scores. In the present study, 54% of nurses had <3
years of PICU experience, whereas 39% of nurses had
>10 years of PICU experience. These proportions of
nurses with extensive and minimal experience were
both larger than the proportions reported in previous
PICU studies.32 33 The presence of such a large
number of inexperienced junior nurses in the PICU
may place additional stress on more experienced
nurses. Indeed, survey items related to staffing (item
17 ‘Work with nurses or other care providers who
are less competent than the child’s care requires’ and
item 21 ‘Work with levels of care provider staffing
that I consider unsafe’ in the MDS-R) were ranked
by nurses as the seventh and eighth most morally
distressing items; these rankings were higher than in
other professions.
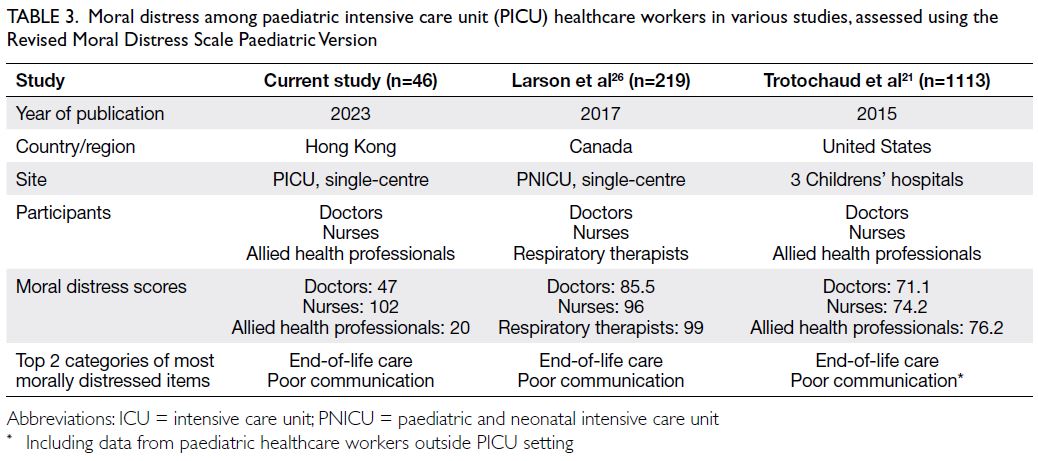
Table 3. Moral distress among paediatric intensive care unit (PICU) healthcare workers in various studies, assessed using the Revised Moral Distress Scale Paediatric Version
Case mix in contribution to moral distress
levels
The PICU case mix might also contribute to moral
distress. The majority of PICU admissions during
the study period involved patients with cancer,
who had considerably higher mortality rates; care
for such patients frequently involved end-of-life
and palliative care issues.34 35 In a study of nurses’
experiences while caring for dying children,
Davies et al36 found that when nurses recognise a
child’s death is inevitable, they often have to manage
conflicting obligations: follow the doctor’s treatment
orders and allow the child to die without unnecessary
pain. These disparate treatment goals for critically ill
children with terminal cancer can exacerbate moral
distress.36 37 In a comparison of moral distress scores
among various paediatric disciplines (eg, general
care and surgical service), Trotochaud et al21 found
that healthcare workers in haematology/oncology
areas experienced the second highest amount of
moral distress on the list, second to healthcare
workers in PICUs. Moreover, the proportion of
patients with cancer in our PICU is much higher
than the proportions in previous PICU studies.38 39
Therefore, it is entirely understandable that moral
distress in our PICU was particularly high among
nurses.
Years of experiences in paediatric intensive
care units in contribution to moral distress levels
The present study revealed a positive correlation
between years of PICU experience and moral
distress scores among nurses, consistent with
previous results concerning healthcare workers in
PICUs and adult ICUs.12 26 This correlation may be
related to effective utilisation of clinical knowledge
and experience, along with greater awareness concerning the impacts of potentially inappropriate
treatment plans on patients.40 Conversely, a study by
Larson et al26 revealed a negative correlation between
moral distress scores and years of experience among
doctors in the PICU. However, the present study
showed no correlation between moral distress scores
and years of experience among doctors. This finding
might be attributed to the small number of doctors
involved, which was insufficient to demonstrate an
association.
Potential impact of moral distress
Moral distress is often associated with the intention to
quit a job.41 42 43 44 The results of the study were consistent
with previous findings. Studies by Sannino et al11 and
Trotochaud et al21 showed that 10.3% to 25% of PICU
nurses intended to quit their jobs because of moral
distress. The proportion of nurses in our study who
intended to quit their job because of moral distress
(34.6%) was higher than the proportions in previous
PICU studies,11 21 which could be explained by their
high moral distress scores. However, further studies
are needed to determine the impact of moral distress
alone on a healthcare worker’s intention to quit their
job, compared with other possible distressing factors
(eg, working hours and promotional opportunities)
that can have a synergistic effect on the decision to
quit.
Strengths and limitations
To our knowledge, this is the first study of moral
distress among healthcare workers in an East Asian
PICU. The results of this study provide insights
concerning the broader understanding of moral
distress in newly established PICUs. The high
response rate also suggests strong participation and
indicates that the study sample is representative of
healthcare workers in our PICU.
However, the results of this study should be
interpreted with the following caveats. First, this
was a single-centre study with a relatively small
sample size, which limits the generalisability of the
findings. The small sample size also hindered further
evaluation of identifiable demographic factors, such
as education level and whether participants had any
children; another study indicated that such factors
may be associated with moral distress.11 Moreover,
the small sample size precluded subgroup analysis.
Second, this study was susceptible to ‘survivorship’
bias because the sample did not include PICU staff
who already quit their jobs, including some who
quit because of moral distress. Third, considering
the cross-sectional nature of this study, causal
relationships among various factors could not be
established. For example, although participants with
higher depression and anxiety scores reported a
stronger intention to quit their jobs, we could not
determine whether these participants reported more psychological symptoms because of their
intention to quit, or if their intention to quit led to
more psychological symptoms. Larger multicentre
studies are needed to further explore moral distress
among healthcare workers in Hong Kong PICUs.
As our unit expands to a 16-bed PICU and a five-bed
high-dependency unit, a longitudinal study will
also enhance the broader understanding of moral
distress dynamics in a developing PICU, as well as
the efficacies of various strategies to address moral
distress.
Coping strategies for moral distress and
stress
Considering the results of this study, moral distress
should be regarded as a key area for service
improvement. The high levels of moral distress
experienced by nurses, as well as the substantial
moral distress in relation to end-of-life care, suggest
that coping strategies should target nurses and focus
on end-of-life education. These coping strategies
are urgently needed to improve staff retention
and quality of care; they can be implemented at
the individual, organisational, and administrative
levels.20
At the individual level, ethics education is
essential for improvements in coping capacity and
sense of moral agency, which can reduce the levels
of moral distress.22 45 Education can be provided
through interactive workshops or self-guided
programmes.41 Prentice et al42 suggested that
education should focus on improving knowledge
regarding patient outcomes, the degree of uncertainty
in specific situations, and appropriate pain control.
Instead of emphasising ethical dilemmas and
underlying principles, education should highlight
communication skills, clarify values, and enhance
the overall understanding of the healthcare system
to address potential environmental conflicts.31 This
approach can ultimately increase staff confidence
(ie, moral courage) in constructively communicating
their concerns.42 Screening tools for various
emotional states, such as the DASS-21, should also
be included to help individuals gain better awareness
of their own psychological well-being and seek
professional help if necessary. Additionally, these
tools can be used to monitor emotions that might
cause moral distress.
At the organisational level, efforts should
be made to promote intra- and interdisciplinary
communication. Poor communication, one of the
five most morally distressing items, can lead to
diminished quality of care, reduced job satisfaction,
and poor patient outcomes.46 Ethics rounds, formal
and informal discussions, and debriefing sessions
regarding morally distressing cases could improve
interdisciplinary communication.22 These initiatives
can help promote better mutual understanding of viewpoints across disciplines and individuals.22
Participation in these events may also allow nurses
to feel more empowered and experience a greater
sense of decision-making autonomy.43 Finally, the
establishment of formal ethical consultation services
may provide support and clarification with respect
to ethical dilemmas.44
At the administrative level, administrators
should recognise that it is acceptable for staff to
perceive moral distress; this perception is a sign
of humanity and an affirmation of moral values.44
Improvements in clinical environments (eg,
reduction of staff shortages, promotion of intra- and
interdisciplinary collaboration, and encouragement
of a safe and supported ethical climate) can help
decrease moral distress.47 These measures include
providing respectful feedback to staff, empowering
staff to voice perceptions and emotions, and making
difficult decisions in a timely manner after open
discussion.48
Conclusion
This study revealed significant differences in moral
distress among doctors, nurses, and allied health
professionals in a newly established PICU in Hong
Kong. Nurses had the highest moral distress scores
among the three groups of PICU healthcare workers
in this study and among published studies involving
PICU nurses. Most areas of moral distress were
related to end-of-life care and poor communication.
Higher moral distress was also associated with
greater depression, anxiety, and intention to quit.
There is an urgent need for interventions to help
healthcare workers cope with moral distress and
create a more sustainable working environment.
Author contributions
Concept or design: WL Cheung, KL Hon, KKY Leung, WF Hui.
Acquisition of data: WL Cheung, KL Hon, KKY Leung, WF Hui.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: WL Cheung, KL Hon, KKY Leung, WF Hui.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, KL Hon was not involved in the review process. Other authors have disclosed no conflicts of interest.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This research was approved by the Hong Kong Children’s Hospital Research Ethics Committee (Ref No.: HKCH-REC-2020-008) and was conducted in accordance with
the Declaration of Helsinki and International Conference
on Harmonisation Good Clinical Practice Guideline. All
participants provided informed consent to take part in the
research.
References
1. Jones S, Rantell K, Stevens K, et al. Outcome at 6 months
after admission for pediatric intensive care: a report of
a national study of pediatric intensive care units in the
United Kingdom. Pediatrics 2006;118:2101-8. Crossref
2. Cremer R, Leclerc F, Lacroix J, Ploin D; GFRUP/RMEF
Chronic Diseases in PICU Study Group. Children with
chronic conditions in pediatric intensive care units located
in predominantly French-speaking regions: prevalence and
implications on rehabilitation care need and utilization.
Crit Care Med 2009;37:1456-62. Crossref
3. Namachivayam P, Shann F, Shekerdemian L, et al. Three
decades of pediatric intensive care: who was admitted,
what happened in intensive care, and what happened
afterward. Pediatr Crit Care Med 2010;11:549-55. Crossref
4. Edwards JD, Houtrow AJ, Vasilevskis EE, et al. Chronic
conditions among children admitted to U.S. pediatric
intensive care units: their prevalence and impact on risk
for mortality and prolonged length of stay. Crit Care Med
2012;40:2196-203. Crossref
5. Ebrahim S, Singh S, Hutchison JS, et al. Adaptive behavior,
functional outcomes, and quality of life outcomes of
children requiring urgent ICU admission. Pediatr Crit
Care Med 2013;14:10-8. Crossref
6. Bruce CR, Miller SM, Zimmerman JL. A qualitative study
exploring moral distress in the ICU team: the importance
of unit functionality and intrateam dynamics. Crit Care
Med 2015;43:823-31. Crossref
7. Austin W. Moral distress and the contemporary plight of
health professionals. HEC Forum 2012;24:27-38. Crossref
8. Jameton A. Nursing practice: the ethical issues. Englewood
Cliffs (NJ): Prentice Hall Inc; 1984.
9. Garros D, Austin W, Carnevale FA. Moral distress in
pediatric intensive care. JAMA Pediatr 2015;169:885-6. Crossref
10. Lusignani M, Giannì ML, Re LG, Buffon ML. Moral distress
among nurses in medical, surgical and intensive-care units.
J Nurs Manag 2017;25:477-85. Crossref
11. Sannino P, Giannì ML, Carini M, et al. Moral distress in the pediatric intensive care unit: an Italian study. Front Pediatr 2019;7:338. Crossref
12. Dodek PM, Wong H, Norena M, et al. Moral distress
in intensive care unit professionals is associated with
profession, age, and years of experience. J Crit Care
2016;31:178-82. Crossref
13. Ohayon MM, Priest RG, Guilleminault C, Caulet M. The
prevalence of depressive disorders in the United Kingdom.
Biol Psychiatry 1999;45:300-7.Crossref
14. de Vargas D, Dias AP. Depression prevalence in
intensive care unit nursing workers: a study at hospitals
in a northwestern city of São Paulo State. Rev Lat Am
Enfermagem 2011;19:1114-21. Crossref
15. Poghosyan L, Clarke SP, Finlayson M, Aiken LH. Nurse
burnout and quality of care: cross-national investigation in six countries. Res Nurs Health 2010;33:288-98. Crossref
16. Humphries N, Morgan K, Conry MC, McGowan Y,
Montgomery A, McGee H. Quality of care and health
professional burnout: narrative literature review. Int J
Health Care Qual Assur 2014;27:293-307. Crossref
17. Prompahakul C, Epstein EG. Moral distress experienced
by non-Western nurses: an integrative review. Nurs Ethics
2020;27:778-95. Crossref
18. Hamric AB, Borchers CT, Epstein EG. Development and
testing of an instrument to measure moral distress in
healthcare professionals. AJOB Prim Res 2012;3:1-9. Crossref
19. Tran TD, Tran T, Fisher J. Validation of the Depression
Anxiety Stress Scales (DASS) 21 as a screening instrument
for depression and anxiety in a rural community-based
cohort of northern Vietnamese women. BMC Psychiatry
2013;13:24. Crossref
20. Wang K, Shi HS, Geng FL, et al. Cross-cultural validation of
the Depression Anxiety Stress Scale–21 in China. Psychol
Assess 2016;28:e88-100. Crossref
21. Trotochaud K, Coleman JR, Krawiecki N, McCracken C.
Moral distress in pediatric healthcare providers. J Pediatr
Nurs 2015;30:908-14. Crossref
22. Sauerland J, Marotta K, Peinemann MA, Berndt A,
Robichaux C. Assessing and addressing moral distress and
ethical climate part II: neonatal and pediatric perspectives.
Dimens Crit Care Nurs 2015;34:33-46. Crossref
23. Papathanassoglou ED, Karanikola MN, Kalafati M,
Giannakopoulou M, Lemonidou C, Albarran JW.
Professional autonomy, collaboration with physicians, and
moral distress among European intensive care nurses. Am
J Crit Care 2012;21:e41-52. Crossref
24. Corley MC. Nurse moral distress: a proposed theory and
research agenda. Nurs Ethics 2002;9:636-50. Crossref
25. Wilkinson JM. Moral distress in nursing practice:
experience and effect. Nurs Forum 1988;23:16-29. Crossref
26. Larson CP, Dryden-Palmer KD, Gibbons C, Parshuram CS.
Moral distress in PICU and neonatal ICU practitioners:
a cross-sectional evaluation. Pediatr Crit Care Med
2017;18:e318-26. Crossref
27. Solomon MZ, Sellers DE, Heller KS, et al. New and
lingering controversies in pediatric end-of-life care.
Pediatrics 2005;116:872-83. Crossref
28. Molloy J, Evans M, Coughlin K. Moral distress in the
resuscitation of extremely premature infants. Nurs Ethics
2015;22:52-63. Crossref
29. McCarthy J, Gastmans C. Moral distress: a review of the
argument-based nursing ethics literature. Nurs Ethics
2015;22:131-52. Crossref
30. LaSala CA, Bjarnson D. Creating workplace environments
that support moral courage. Online J Issues Nurs
2010;15:Manuscript 4. Crossref
31. Epstein EG, Delgado S. Understanding and addressing
moral distress. Online J Issues Nurs 2010;15:Manuscript 1. Crossref
32. Ahmed GE, Abosamra OM. Knowledge of pediatric
critical care nurses regarding evidence based guidelines
for prevention of ventilator associated pneumonia (VAP). J
Educ Pract 2015;6:94-101.
33. Hickey PA, Pasquali SK, Gaynor JW, et al. Critical care
nursing’s impact on pediatric patient outcomes. Ann
Thorac Surg 2016;102:1375-80. Crossref
34. Earle CC, Park ER, Lai B, Weeks JC, Ayanian JZ, Block
S. Identifying potential indicators of the quality of end-of-life cancer care from administrative data. J Clin Oncol 2003;21:1133-8. Crossref
35. Wösten-van Asperen RM, van Gestel JP, van Grotel M,
et al. PICU mortality of children with cancer admitted to
pediatric intensive care unit a systematic review and meta-analysis.
Crit Rev Oncol Hematol 2019;142:153-63. Crossref
36. Davies B, Clarke D, Connaughty S, et al. Caring for dying children: nurses’ experiences. Pediatr Nurs 1996;22:500-7.
37. Johnston EE, Alvarez E, Saynina O, Sanders L, Bhatia
S, Chamberlain LJ. Disparities in the intensity of
end-of-life care for children with cancer. Pediatrics
2017;140:e20170671. Crossref
38. Demaret P, Pettersen G, Hubert P, Teira P, Emeriaud G.
The critically-ill pediatric hemato-oncology patient:
epidemiology, management, and strategy of transfer to the
pediatric intensive care unit. Ann Intensive Care 2012;2:14. Crossref
39. Dalton HJ, Slonim AD, Pollack MM. Multicenter outcome
of pediatric oncology patients requiring intensive care.
Pediatr Hematol Oncol 2003;20:643-9. Crossref
40. Zhang W, Wu X, Zhan Y, Ci L, Sun C. Moral distress and its
influencing factors: a cross-sectional study in China. Nurs
Ethics 2018;25:470-80. Crossref
41. Beumer CM. Innovative solutions: the effect of a workshop
on reducing the experience of moral distress in an intensive
care unit setting. Dimens Crit Care Nurs 2008;27:263-7. Crossref
42. Prentice T, Janvier A, Gillam L, Davis PG. Moral distress
within neonatal and paediatric intensive care units: a
systematic review. Arch Dis Child 2016;101:701-8. Crossref
43. Browning AM. CNE article: moral distress and
psychological empowerment in critical care nurses caring
for adults at end of life. Am J Crit Care 2013;22:143-51. Crossref
44. Santos RP, Garros D, Carnevale F. Difficult decisions in
pediatric practice and moral distress in the intensive care
unit. Rev Bras Ter Intensiva 2018;30:226-32. Crossref
45. Burston AS, Tuckett AG. Moral distress in nursing:
contributing factors, outcomes and interventions. Nurs
Ethics 2013;20:312-24. Crossref
46. Whitehead PB, Herbertson RK, Hamric AB, Epstein EG,
Fisher JM. Moral distress among healthcare professionals:
report of an institution-wide survey. J Nurs Scholarsh
2015;47:117-25. Crossref
47. Atabay G, Çangarli BG, Penbek Ş. Impact of ethical climate
on moral distress revisited: multidimensional view. Nurs
Ethics 2015;22:103-16. Crossref
48. Benoit DD, Jensen HI, Malmgren J, et al. Outcome in
patients perceived as receiving excessive care across
different ethical climates: a prospective study in 68
intensive care units in Europe and the USA. Intensive Care
Med 2018;44:1039-49. Crossref