Hong Kong Med J 2023 Oct;29(5):459–61 | Epub 19 Sep 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Ultrasound-guided spinal anaesthesia in a patient with achondroplastic dwarfism and scoliosis: a case report
Banu Kilicaslan, MD
Department of Anesthesiology and Reanimation, Faculty of Medicine, Hacettepe University, Ankara, Turkey
Corresponding author: Dr Banu Kilicaslan (banuk9oct@gmail.com)
Case presentation
In February 2019, a 27-year-old woman who was
classified as American Society of Anesthesiologists
class III and 8 weeks pregnant presented for elective
therapeutic curettage and tubal ligation. She was
110 cm tall and weighed 30 kg. Her medical history
was notable for thoracolumbar kyphoscoliosis,
congenital dwarfism, and restrictive lung disease.
The patient’s medical history revealed that her
previous two pregnancies were terminated due to
shortness of breathing, reduced exercise tolerance,
and the possibility that progressing pregnancy might
create a life-threatening condition, first one in the
17th week and the other one in the 22nd week of
pregnancy. Her airway assessment was normal but
pulmonary function testing revealed a restrictive
lung disease. Ultrasound-guided spinal anaesthesia
was planned.
In the operating room, after standard
monitorisation, she was placed in a sitting position.
The midline of the spines and intervertebral disc
space were impossible to palpate because of the
severely rotated lumbar spines by marked scoliosis.
Preprocedural ultrasound scan using curved array
probe 2-5 MHz with LOGIQ e R7 ultrasound system
(GE HealthCare, Washington DC, United States) for
marking of insertion site were conducted in both
paramedian longitudinal and transverse planes at
different intervertebral levels.
In the scanning of the paramedian
longitudinal plane, the transducer was placed over
the lumbosacral spine approximately 2 cm lateral
to the midline in a cephalad-caudad direction to
find the appropriate lumbar interlaminar spaces
(the ligamentum flavum–dura mater complex and
posterior face of the vertebral body). The L2-L3 to
L4-L5 interlaminar spaces were identified. In the
transverse plane scanning, deeper structures were
visible between the spinous process. In this view,
the presence of bilateral transverse processes in the
same plane was the clue for the correct intervertebral
space. In this space, the vertebral column did not
rotate due to scoliosis and was the most suitable
intervertebral space for the needle puncture. The
depth of the dorsal dura from the skin was measured as 3.73 cm in transverse view (Fig 1). The appropriate
intervertebral space (L2-L3) was determined to be 2
cm laterally away to the right of the expected spinal
midline as the intersection point of the line obtained
from the paramedian longitudinal image and the line
obtained from the transverse image (Fig 2).
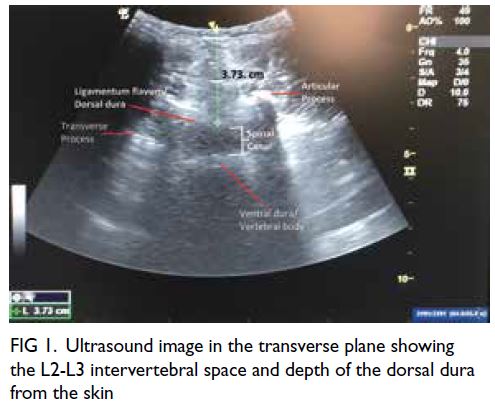
Figure 1. Ultrasound image in the transverse plane showing the L2-L3 intervertebral space and depth of the dorsal dura from the skin
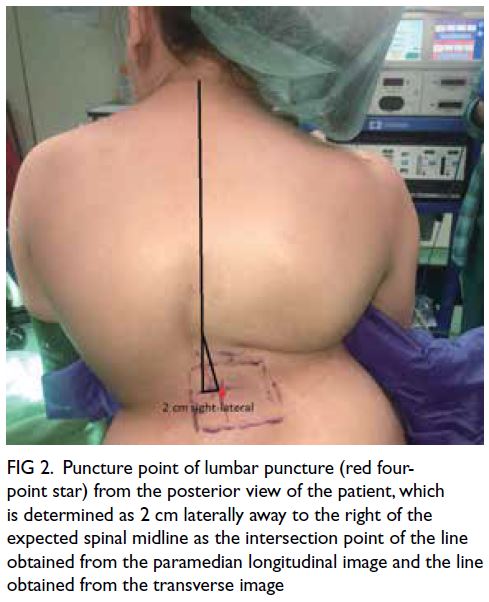
Figure 2. Puncture point of lumbar puncture (red four-point star) from the posterior view of the patient, which is determined as 2 cm laterally away to the right of the expected spinal midline as the intersection point of the line obtained from the paramedian longitudinal image and the line obtained from the transverse image
After aseptic precautions, spinal anaesthesia
was performed by using 5-mg 0.5% hyperbaric
bupivacaine, with 10-μg fentanyl (1.2 mL in volume)
at the L2-L3 interspace without any complications.
The sensorial block was achieved up to the T4
dermatome level bilaterally and the patient was
sedated with dexmedetomidine (200 mcg/2 mL).
Motor functions regressed to her basal level 4 hours
after the initial intrathecal injection and the sensory
component of the block returned by 5 hours.
The patient was discharged on postoperative
day 2 uneventfully without postdural puncture
headache and back pain. A follow-up 1 month after
the surgery showed no further deterioration in her
neurological condition.
Discussion
This case illustrates two important points. First, the transverse plane image shows the rotation point of
the vertebral column better than the longitudinal plane; thus, this makes it easier to decide on the
most appropriate intervertebral puncture point
in the placement of a spinal block in a patient
with abnormal spinal anatomy. Second, this case
highlights the value of a systematic approach and an
individual risk-benefit ratio on a case-by-case basis
when performing neuraxial anaesthesia in patients
with severe scoliosis and dwarfism.
Shiang et al1 demonstrated that nearly all cases of achondroplasia are autosomal dominant and most
of those with achondroplasia will have a normal or
near-normal life expectancy. Therefore, they may live
long enough to experience anaesthesia for various
reasons. Clinical features that may be important for
anaesthesia management are midfacial abnormality,
craniocervical constriction, thoracolumbar
kyphosis, lumbosacral spinal stenosis, and cardiac
and pulmonary abnormalities.
The patient whom we have described with
achondroplastic dwarfism resulting severe in
scoliosis and moderate restrictive lung disease
had a potential risk for general anaesthesia due to
instability of the cervical spine, limited respiratory
reserve, and predisposition to the risk of malignant
hyperthermia. On the other hand, scoliosis and
spinal stenosis might further complicate patient
management with neuraxial anaesthesia technique.2
In our case, the patient’s previous two pregnancies
were terminated without using any anaesthetic
methods. The terminations were performed
by medical abortus (200 mcg oral and vaginal misoprostol) with intramuscular meperidine
analgesia. For the intervention in our case, spinal
anaesthesia was planned after mutual consent had
been achieved with the patient and the medical
team. Because of spinal deformity of the patient,
spinal anaesthesia was predicted to be challenging
even with ultrasound assistance.2 3
The drug and the dosage choice for spinal
anaesthesia in achondroplastic patients with severe
scoliosis may be of concern, as an unpredictable
spread of drug may contribute to a high blockade
that could be catastrophic in patients with a difficult
airway and limited pulmonary reserve. It has been
reported that a satisfactory block level was obtained
with an administration of 0.06 mg/cm height of
intrathecal bupivacaine.4 In the present case, as
the height of the patient was 110 cm and the body
mass index was 24.8 kg/m2, 5-mg bupivacaine and
10-μg fentanyl (1.2 mL in volume) were administered
intrathecally, and a T4-level block was obtained.
For local anaesthetic for spinal anaesthesia in these
patients, we do not recommend dosages >0.06 mg/cm
height to avoid complications caused by abnormal
block levels.
In our patient in whom we had predicted
difficult spinal anaesthesia, we preferred to use
ultrasound before the procedure for landmark
identification. Numerous reports indicate that this
application facilitates technical performance in
obstetric and paediatric patients and in patients
with difficult spinal anatomy.5 However, real-time
ultrasound guidance may provide additional
advantages by taking into account the positional
changes of the patient during the procedure. Ravi et al6
compared the efficacy of real‑time ultrasound‑guided
paramedian approach and preprocedural ultrasound
landmark‑guided paramedian approach in obese
patients. They determined that the time taken for
the identification of the space and for successful
lumbar puncture, and the number of attempts and
passes was more in the latter group as compared
to the former group.6 Although it is not technically
difficult to recognise spinal spaces with real-time
ultrasonography, the success rates for spinal
anaesthesia were similar for both techniques.6 Real-time
ultrasonography may be a better alternative as
it can show all structures that cannot be observed
during the procedure with ‘pre-procedural
ultrasonography’.
An experienced practitioner can achieve >90%
success rate in identifying the epidural space in
difficult situations using ultrasonography, as in the
current patient with difficult spinal anatomy.5 In our
experience, a single screening method of ultrasound
imaging in the transverse plane gives working
knowledge about the anatomical structures. Thus,
the asymmetry of structures on the two sides of the
spinal canal, mainly the articular and the transverse processes in the interspace, can be used as a guide
to determine the level of the rotation on the spinal
column. In our patient, no anatomical landmarks
were identifiable, and it was impossible to detect the
level of rotation of scoliosis. By using ultrasound, we
precisely determined the L2-L3 intervertebral space
available for the placement of spinal block and also
the depth of the dorsal dura from the skin that was
measured as 3.73 cm in the transverse view.
In conclusion, ultrasound-guided spinal
anaesthesia is feasible and can greatly facilitate a
spinal technique, especially in the transverse plane, in
the presence of severe scoliosis with achondroplastic
dwarfism.
Author contributions
The author contributed to the concept or design of the study, acquisition of the data, analysis or interpretation of the data, drafting of the manuscript, and critical revision of the manuscript for important intellectual content. The author had full access to the data, contributed to the study, approved the final version for publication, and takes responsibility for its
accuracy and integrity.
Conflicts of interest
The author declares no conflicts of interest.
Acknowledgement
The author thanks Dr Coskun Salman and his team at the Department of Obstetrics and Gynecology, Hacettepe
University for their sincere support of taking care of the
patient during and after the operation.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki and has provided informed consent for the
publication of the report along with the data, radiological
images, and photographs.
References
1. Shiang R, Thompson LM, Zhu YZ, et al. Mutations in the transmembrane domain of FGFR3 cause the most common genetic form of dwarfism, achondroplasia. Cell 1994;78:335-42. Crossref
2. Mikhael H, Vadivelu N, Braveman F. Safety of spinal anesthesia in a patient with achondroplasia for cesarean section. Curr Drug Saf 2011;6:130-1. Crossref
3. Lange EM, Toledo P, Stariha J, Nixon HC. Anesthetic management for cesarean delivery in parturients with a diagnosis of dwarfism. Can J Anaesth 2016;63:945-51. Crossref
4. Samra T, Sharma S. Estimation of the dose of hyperbaric bupivacaine for spinal anaesthesia for emergency caesarean section in an achondroplastic dwarf. Indian J Anaesth 2010;54:481-2. Crossref
5. Perlas A, Chaparro LE, Chin KJ. Lumbar neuraxial ultrasound for spinal and epidural anesthesia: a systematic review and meta-analysis. Reg Anesth Pain Med 2016;41:251-60. Crossref
6. Ravi PR, Naik S, Joshi MC, Singh S. Real-time ultrasound-guided spinal anaesthesia vs pre-procedural ultrasound-guided spinal anaesthesia in obese patients. Indian J Anaesth 2021;65:356-61. Crossref

