Hong Kong Med J 2023 Oct;29(5):432–42 | Epub 1 Aug 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE (HEALTHCARE IN MAINLAND CHINA)
Anaemia prevalence and risk factors among children aged 6 to 23 months in rural China
L Zeng, MA, BA; W Zheng, MSc, BSc; Q Gao, PhD, MEcon; N Qiao, PhD, LLM; K Du, MEcon; A Yue, PhD, MEcon
Center for Experimental Economics in Education, Shaanxi Normal University, Xi’an, China
Corresponding author: Dr Q Gao (gqiufeng820@163.com)
Abstract
Introduction: Anaemia is a global public health
problem among children. However, few studies have
examined anaemia prevalence and risk factors among
Chinese children of different ages, particularly in
poor rural areas. This study investigated these two
aspects among children aged 6 to 23 months in poor
rural areas of China.
Methods: This cross-sectional study included 1132
children aged 6 to 23 months in three prefectures
of the Qinba Mountains area. A finger prick blood
test for haemoglobin and anaemia was conducted,
along with household surveys of socio-demographic
characteristics, illness characteristics, and feeding
practices. Multiple linear and logistic regression
analyses were used to determine predictors of
anaemia.
Results: Overall, 42.6% of children in the study
displayed anaemia. Children aged 6 to 11 months
had the highest anaemia prevalence (53.6%).
Anaemia risk factors differed among age-groups
and throughout the overall sample. Bivariate
and multivariable regression results showed that
continued breastfeeding, any history of formula
feeding, and consumption of iron-rich or iron-fortified foods were associated with
anaemia prevalence. However, continued breastfeeding and any
history of formula feeding had the greatest impact
across age-groups (both P<0.05).
Conclusion: Anaemia remains a severe public health problem among children aged 6 to 23 months
in rural China. Healthy feeding practices, nutritional
health knowledge, and nutrition improvement
projects are needed to reduce the burden of anaemia
among children in rural areas of China.
New knowledge added by this study
- The prevalence of anaemia among rural children was higher in the Qinba Mountains area than in the central and eastern areas of China.
- Anaemia prevalence varied among age-groups, and the lowest prevalence was observed in children aged 18 to 23 months.
- Continued breastfeeding, any history of formula feeding, and consumption of iron-rich or iron-fortified foods were associated with anaemia prevalence among children in rural China.
- The government should more closely monitor anaemia among children in rural areas and introduce relevant policies to address this issue.
- Healthy feeding practices, nutritional health knowledge, and nutrition improvement projects are needed to reduce the burden of anaemia among children in rural China.
Introduction
Anaemia is a global health issue that affects one-quarter of the world’s population; it is particularly
prevalent among preschool-aged children in
developing countries.1 Approximately 47.4% of
preschool-aged children worldwide display anaemia.1
There are three categories of factors associated with
anaemia: inherited disorders, infectious diseases, and micronutrient deficiencies.2 3 Among these
factors, iron deficiency is the most common cause,4
especially in China.5 There is evidence that iron
deficiency anaemia affects developmental potential
in children.6 7
Anaemia prevalence among children in China,
particularly in poor rural areas, is higher than that
in developed countries.2 3 In the United States and the Netherlands, the rate is <10%.2 The rate in urban
areas of China is <20%,8 9 whereas the prevalence
in rural areas is more than double that in urban
areas.10 11 12 Thus, there is a need for considerable
effort from the Chinese Government to ensure that
regional anaemia prevalence among children aged
<5 years are below 10% by 2030.13
Few studies have examined factors associated
with anaemia among children of different
ages, particularly in poor rural areas of China.
Previous studies have shown that anaemia may be
associated with the demographic, social, and health
characteristics of children and their families.14 15 16 17
Feeding practices have also been associated with
anaemia in children.1 18 19 20 However, few studies
have extensively analysed anaemia prevalence and
associated factors among children of different ages
in rural China.16 21 22 For example, one study explored
risk factors for anaemia in children aged 0 to 5
months and those aged 6 to 36 months; however, the
age ranges were excessively broad.14 In another study
exploring risk factors for anaemia in children aged
<36 months, stratified according to age, relatively few
potential associated factors (eg, socio-demographic
and illness characteristics) were considered; there
was no consideration of other potential associated
factors, such as complementary feeding.18
This study was therefore conducted to explore
anaemia prevalence and risk factors among children
aged 6 to 23 months in poor rural areas of China;
analyses were performed focusing on the overall sample and with stratification according to age.
Therefore, we established three objectives: to
examine anaemia prevalence among children in the
study area; to identify socio-demographic and illness
characteristics associated with anaemia in children;
and to explore feeding practices associated with
anaemia in children.
Methods
Sample selection
This study was conducted in 22 nationally designated
poverty-stricken counties (all of which are now out
of poverty) within three prefectures in the Qinba
Mountains area of northwest China. By the end
of 2015 in the survey year, the total population of
the sample area was 8 464 200, including a rural
population of 4 716 100 (55.7%). The per capita
income was 20 939 yuan, which was less than half
of the national per capita income (42 359 yuan) in
the same period in China.23 Sample villages and
households were selected in two stages. First, from
each of the 22 counties, all townships (ie, the middle
level of administration between county and village)
that met the criteria were selected to participate in
the study, with two exceptions: the township in each
county containing the county government (which
represents the level of county development), as well
as townships containing <800 people. In total, 115 of
400 townships were included in this study. Second,
in each sample township, we selected random
villages with ≥10 children. All children in our target
age range (6-23 months) were enrolled in the study,
including premature but not congenitally abnormal
children; thus, we included 1694 children and their
households. Because one prefecture did not survey
feeding practices, the corresponding analysis only
included 1210 participants from the other two
sample prefectures. In total, 1132 participants
(children and their households) fully completed the
survey (response rate of 93.6%).
Data collection
Survey data were collected in three waves in
November 2015, April 2016, and February 2017.
After identification of the primary caregiver
responsible for a child’s diet and care, well-trained
enumerators collected information through one-on-one questionnaire interviews with the primary
caregiver.
First, specific components of socio-demographic
and illness characteristics were
recorded in the survey. The socio-demographic
characteristics included the child’s age, sex,
gestational age, and birth order; the primary
caregiver’s identity; maternal education and age;
and whether the family received social security
support (ie, government welfare for the lowest income families nationwide). Illness characteristics
comprised any history of fever, cold, or diarrhoea in
the previous 2 weeks.
Second, detailed information regarding the
child’s feeding practices was collected via dietary
recall, using a series of questions based on the
‘Indicators for assessing infant feeding practices’
compiled by the World Health Organization
(WHO).24 The following definitions were used:
continued breastfeeding, proportion of children
aged 6 to 23 months who had received breast milk
during the previous day; any history of formula
feeding, proportion of children who had ever been
formula-fed; minimum dietary diversity, proportion
of children aged 6 to 23 months who had consumed
≥4 of the 7 food groups under WHO’s classification24
during the previous day; minimum meal frequency,
proportion of children aged 6 to 23 months who
consumed a meal at a standard frequency during the
previous day, considering their breastfeeding status
(two times for breastfed infants aged 6 to 8 months,
three times for breastfed children aged 9 to 23 months,
and four times for non-breastfed children aged 6 to
23 months); minimum acceptable diet, proportion of
children aged 6 to 23 months who consumed a meal
that met standards for minimum dietary diversity
and minimum meal frequency during the previous
day; and consumption of iron-rich or iron-fortified
foods, proportion of children who consumed iron-rich
or iron-fortified foods specifically designed for
children aged 6 to 23 months during the previous
day.
Third, each child’s haemoglobin (Hb)
concentration and anaemia status were assessed by
trained nurses from the Xi’an Jiaotong University,
who performed tests on fingertip blood samples
collected from all children. These analyses
were performed using the HemoCue Hb201
haemoglobin analyser (HemoCue Inc, Ängelholm,
Sweden), which is accurate, rapid, and convenient
for children in remote rural areas.11 15 21 25 Its
measurement accuracy is 1 g/L.18 We confirmed
that the sample villages’ altitudes were below
1000 m; therefore, no adjustments to measured
Hb concentrations were required. Anaemia status
was determined according to Hb concentration
and divided into four categories: non-anaemic,
Hb concentration ≥110 g/L; mild, 100-109 g/L;
moderate, 70-99 g/L; and severe, <70 g/L.26 Children
with severe anaemia were referred to a local hospital
for treatment.
Statistical analysis
Statistical analysis was performed using STATA
version 15.0 (Stata Corporation, College Station
[TX], United States). The children’s socio-demographic
and illness characteristics, feeding
practices, and anaemia statuses were summarised using descriptive statistics. In bivariate analyses,
P values for differences in mean Hb concentration
between subgroups were estimated using t tests. The
Pearson Chi squared test was also used to compare
categorical variables between anaemia and non-anaemia
groups. Multiple linear regression analyses
were performed to identify covariates that were
significantly associated with Hb concentration.
Multiple logistic regression analysis was used to
identify predictors of anaemia. The threshold for
statistical significance was set at P<0.05.
Results
Socio-demographic characteristics, illness characteristics, and feeding practices
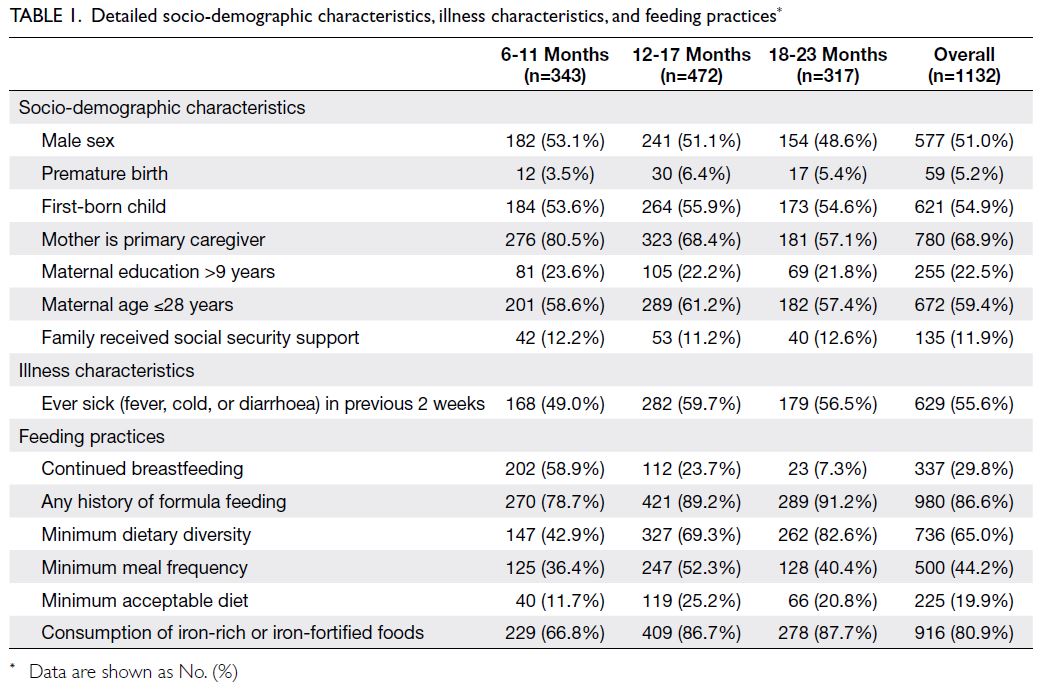
Table 1 presents the socio-demographic and illness
characteristics of the 1132 children. Of these, 51.0%
were boys, 5.2% were born prematurely, and more
than half were first-born (54.9%). Additionally,
more than half of the primary caregivers (68.9%)
were the children’s mothers; the remaining primary
caregivers were the children’s grandmothers. Less
than one-quarter of the children’s mothers (22.5%)
had >9 years of education, and more than half of
them (59.4%) were aged ≤28 years. Social security
support was received by 11.9% of the participating
families. Approximately half of the children (55.6%)
had been sick (with fever, cold, or diarrhoea) in the
previous 2 weeks.
Table 1 also presents the feeding practices
of the children; notably, 29.8% and 86.6% of the
children had continued breastfeeding and any
history of formula feeding, respectively. With
respect to complementary feeding, most children
(80.9%) consumed iron-rich or iron-fortified
foods; however, approximately 65.0% and 44.2%
of the children met the standard requirements for
minimum dietary diversity and meal frequency,
respectively. Moreover, only 19.9% of the children
met the standard requirement for a minimum
acceptable diet. All children were divided into three
age-groups: 6 to 11 months (n=343), 12 to 17 months
(n=472), and 18 to 23 months (n=317).
Prevalence of haemoglobin concentration and anaemia
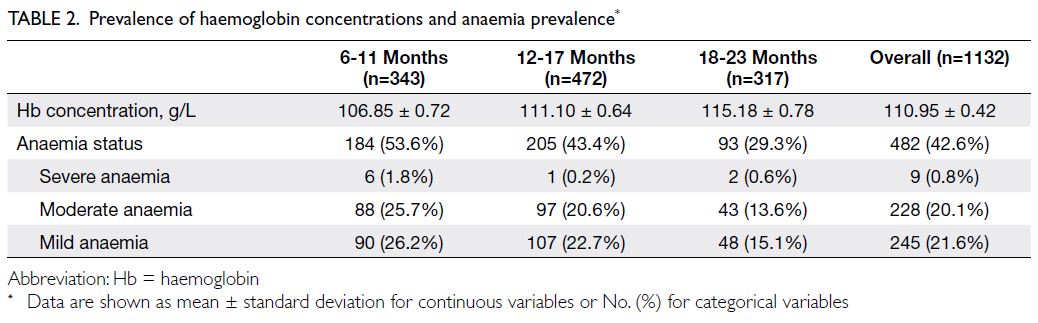
Table 2 presents the children’s Hb concentrations
and anaemia prevalence; the mean and standard
deviation of their Hb concentration was 110.95 ± 0.42 g/L. Overall, 42.6% of the children had anaemia,
including 21.6% with mild anaemia, 20.1% with
moderate anaemia, and 0.8% with severe anaemia.
A similar pattern was observed upon stratification
according to age: few children had severe anaemia,
and approximately one-quarter of children displayed
mild or moderate anaemia in 6 to 11 months and 12
to 17 months age-groups.
As age increased across the groups (from
6-11 months to 12-17 months, and then to 18-23
months), the mean Hb concentration increased,
whereas anaemia prevalence decreased. The mean
and standard deviation Hb concentrations in the
three groups (from youngest to oldest) were 106.85
± 0.72 g/L, 111.10 ± 0.64 g/L, and 115.18 ± 0.78 g/L,
respectively. Furthermore, children aged 6 to 11
months had the highest anaemia prevalence (53.6%),
followed by children aged 12 to 17 months (43.4%)
and then children aged 18 to 23 months (29.3%).
Bivariate analysis of socio-demographic and
illness characteristics
Table 3 shows the bivariate associations of Hb concentration/anaemia prevalence with
the children’s socio-demographic and illness
characteristics, stratified according to age. Among
children aged 12 to 17 months, birth order and
health status were significantly associated with Hb
concentration/anaemia prevalence; however, the
associations were not statistically significant in the
other two age-groups or the overall sample. Among
children aged 12 to 17 months, Hb concentrations
were significantly higher in first-born children than
in non-first-born children (P=0.020). Moreover,
among children aged 12 to 17 months, children who
had been sick in the previous 2 weeks were more
likely to display anaemia, compared with children
who had not been sick (P=0.029).
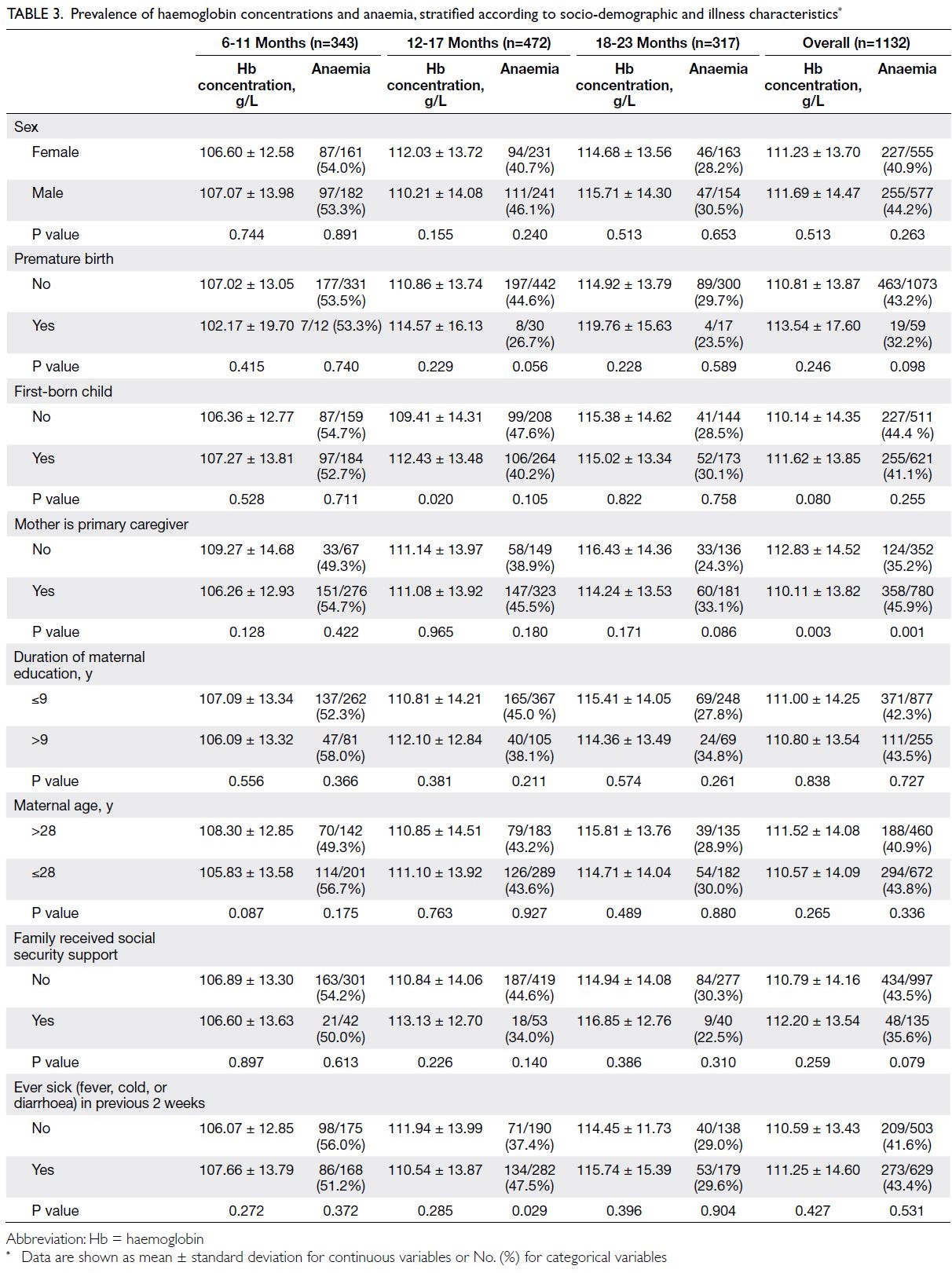
Table 3. Prevalence of haemoglobin concentrations and anaemia, stratified according to socio-demographic and illness characteristics
A similar trend was observed regarding
the relationship of Hb concentration/anaemia
prevalence with the primary caregiver; however, the
only statistically significant result was observed in the
overall sample. In summary, the Hb concentration
was lower (P=0.003) and anaemia prevalence was
higher (P=0.001) among children whose primary
caregiver was their mother, compared with children
who had a different primary caregiver. Furthermore, in the overall sample and all age-groups, there were
no significant binary associations between the Hb
concentration/anaemia prevalence and variables
such as sex, premature birth, maternal education
and age, or receipt of social security support.
Bivariate analysis of feeding practice variables
Table 4 shows the bivariate associations of Hb concentration/anaemia prevalence with feeding
practices. The associations varied among age-groups
and in the overall sample. Children with any history
of formula feeding had higher Hb concentrations and
lower rates of anaemia, compared with children who
had never received formula (both P<0.001); these
differences were statistically significant in all age-groups.
Children who had continued breastfeeding
displayed lower Hb concentrations and higher rates
of anaemia, compared with children who had stopped
breastfeeding (both P<0.001); these differences
were statistically significant among children aged
12 to 17 months (both Hb concentration and
anaemia prevalence) and 18 to 23 months (anaemia
prevalence only).
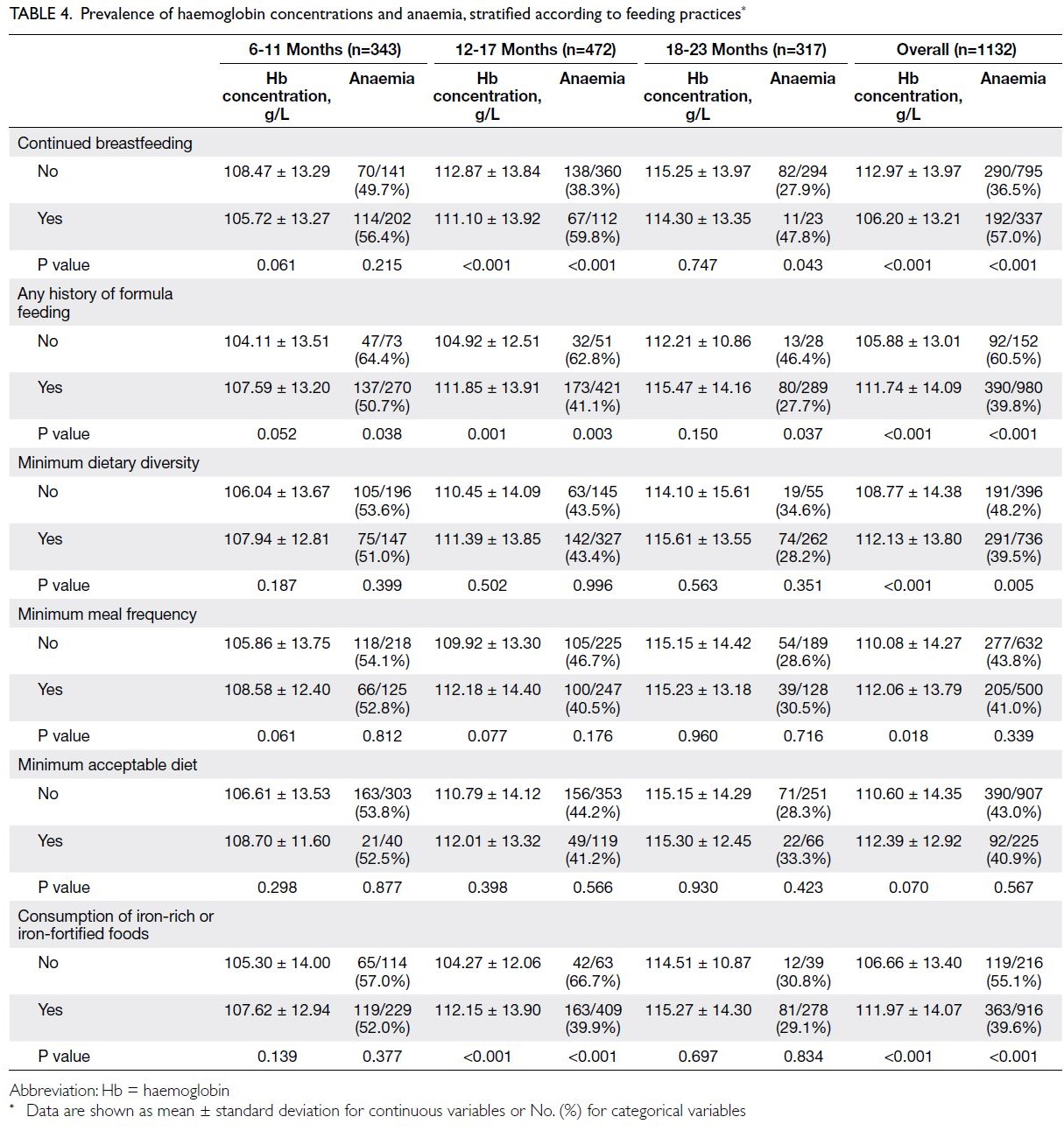
Table 4. Prevalence of haemoglobin concentrations and anaemia, stratified according to feeding practices
Additionally, observable complementary food–related variables were significantly associated with
Hb concentration and anaemia prevalence. In the
overall sample, children with feeding practices that
met the minimum requirements for dietary diversity
had significantly higher Hb concentrations (P<0.001)
and lower rates of anaemia (P=0.005), compared with
children whose feeding practices did not meet those
requirements. Children with feeding practices that
met the minimum meal frequency requirements had
higher Hb concentrations (P=0.018), compared with
children whose feeding practices did not meet those
requirements. Regarding the consumption of iron-rich
or iron-fortified foods, a significant positive
association with Hb concentration and a significant
negative association with anaemia prevalence was
observed among children aged 12 to 17 months and
in the overall sample (both P<0.001).
Multivariable analysis of socio-demographic
and illness characteristics, and feeding practice variables
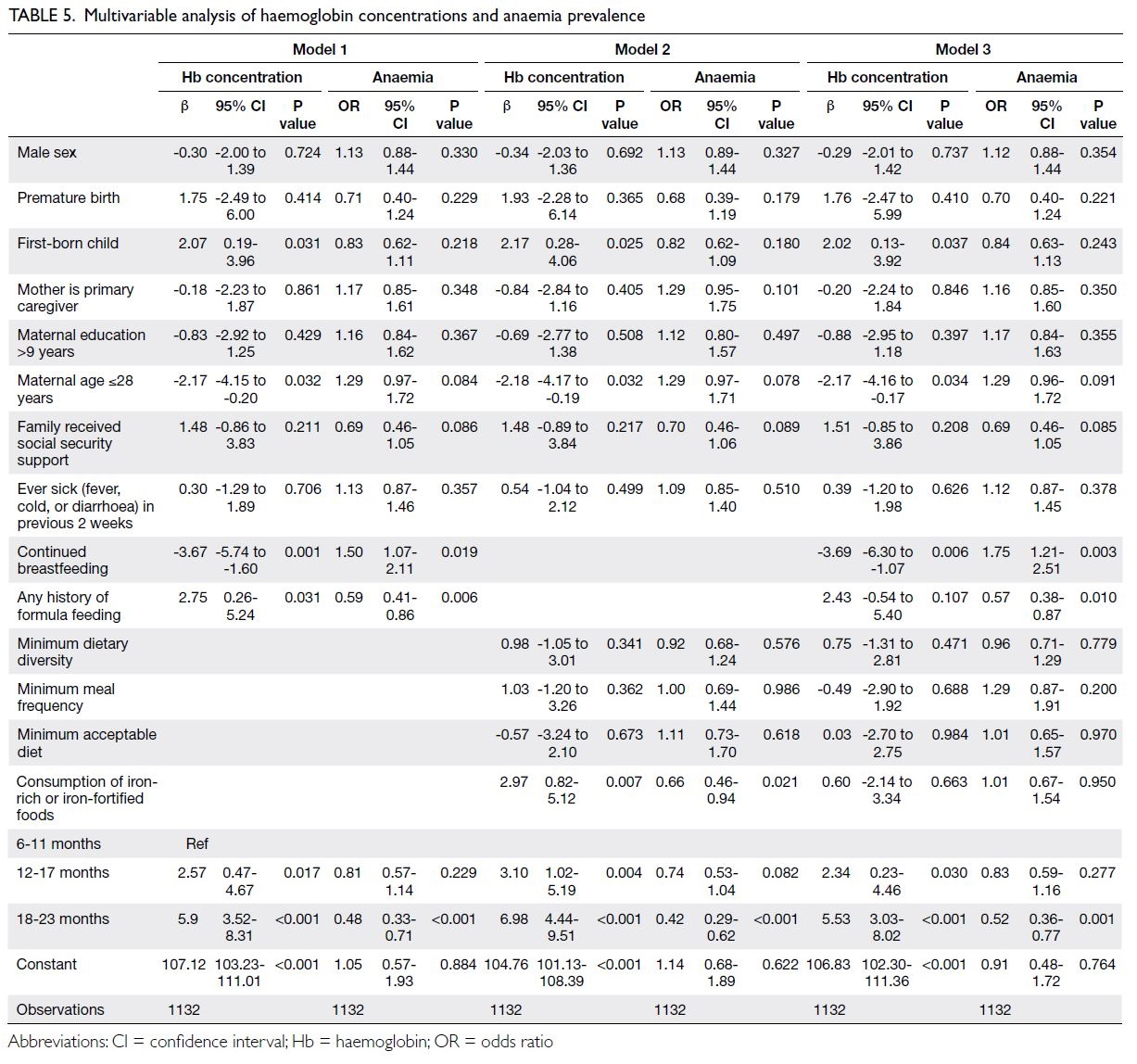
The results of multivariable analysis of the relationship
between Hb concentration and anaemia prevalence
are presented in Table 5. The initial multivariable
model included variables related to socio-demographic
and illness characteristics, continued
breastfeeding, and any history of formula feeding;
the results showed that Hb concentrations were
significantly higher in first-born children (P=0.031)
and significantly lower in children of younger
mothers (P=0.032), but no factors were significantly
associated with anaemia prevalence. Any history of
formula feeding was positively associated with Hb
concentration (P=0.031) and negatively associated
with anaemia prevalence (odds ratio [OR]=0.59,
95% confidence interval [CI]=0.41-0.86; P=0.006),
whereas continued breastfeeding was significantly
negatively associated with Hb concentration
(P=0.001) and positively associated with anaemia
prevalence (OR=1.50, 95% CI=1.07-2.11; P=0.019).
A subsequent multivariable model included socio-demographic
and illness characteristics, as well as complementary food–related variables; the results
showed that Hb concentration remained positively
associated with first-born-child status (P=0.025)
and younger maternal age (P=0.032), whereas
consumption of iron-rich or iron-fortified foods
was negatively associated with anaemia prevalence
(OR=0.66, 95% CI=0.46-0.94; P=0.021). The final
multivariable model included all variables; the
results showed that continued breastfeeding was
positively associated with anaemia prevalence
(OR=1.75, 95% CI=1.21-2.51; P=0.003), whereas any
history of formula feeding was negatively associated
with anaemia prevalence (OR=0.57, 95% CI=0.38-0.87; P=0.010).
Discussion
In this analysis of 1132 children aged 6 to 23 months
in a poor rural area of China, we found that the
anaemia prevalence was high in the overall sample,
although it varied among age-groups. Bivariate
analysis of socio-demographic characteristics,
illness characteristics, and feeding practices revealed
diverse risk factors among age-groups and in the
overall sample. Additionally, multivariable analysis
showed that feeding practice–related variables were
risk factors for anaemia prevalence. Compared with
complementary food–related variables, continued
breastfeeding and any history of formula feeding had
much greater impacts across age-groups.
Anaemia prevalence among children in rural
China
Our findings revealed that 42.6% of children in the
overall sample displayed anaemia, and anaemia
prevalence among children in rural China varied
according to age. According to WHO guidelines,
anaemia prevalence exceeding 40% is a ‘severe
public health problem’.26 Previous studies revealed
anaemia prevalence among children in rural areas of
central China (29.7%) and eastern China (24.2%)21 27;
the prevalence was higher among children in our
sample, indicating that urgent attention is needed
regarding anaemia among children in rural areas
of western China. Furthermore, our results showed
that anaemia prevalence decreased with increasing
age, consistent with previous reports.8 15 17 28 We
found that anaemia prevalence was lower among
children aged 18 to 23 months than among those
aged 6 to 11 months or 12 to 17 months; this may
have been related to the successful inclusion of
complementary foods after 12 months of age. There
is evidence that increasing iron intake from various
foods contributes to a slow decrease in anaemia
prevalence.26 Overall, our findings imply substantial
differences in anaemia prevalence according to age;
thus, analyses of anaemia in children, along with
its risk factors, should consider the effect of age (in
months).
Bivariate and multivariable analyses of risk
factors of anaemia
Our bivariate analysis showed significant differences
in risk factors for low Hb concentration and anaemia
prevalence among children in the overall sample and
in each age-group. These findings were consistent
with the results of other studies regarding anaemia
among children in China.21 22 In particular, a
study of children aged 6 to 23 months showed
that complementary feeding practices meeting
the minimum dietary diversity requirement were
negatively associated with anaemia prevalence
among children aged 12 to 17 months; however, the
association was not statistically significant among children aged 6 to 11 months or 18 to 23 months.
Additionally, complementary feeding practices
meeting the minimum meal frequency requirement
were negatively associated with anaemia prevalence
in all age-groups.22 Therefore, we conclude that the
risk factors for anaemia prevalence in children differ
according to age.
Our results also indicated that socio-demographic
and illness characteristics were
associated with anaemia prevalence among children
in poor rural areas of China, consistent with previous
findings.11 17 Specifically, birth order and a history
of illness in the previous 2 weeks were statistically
significant risk factors for anaemia in children aged 12 to 17 months. Regarding health status,
previous studies revealed that anaemia is positively
associated with a history of recurrent illness, such as
diarrhoea or fever.11 19 We found that children who
had been sick in the previous 2 weeks were more
likely to display anaemia, presumably because they
experienced a loss of appetite and had poor intestinal
nutrient absorption.27 The child’s relationship with
their primary caregiver was significantly associated
with Hb concentration and anaemia prevalence in
the overall sample. Previous studies showed greater
dependence on breast milk among children whose
primary caregiver was their mother; this dependence
may lead to anaemia. Thus, the provision of adequate
nutrition via complementary food is recommended.29
Bivariate and multivariable analyses showed
that feeding practices (continued breastfeeding, any
history of formula feeding, and consumption of iron-rich
or iron-fortified foods) were associated with
anaemia prevalence in poor rural areas of China.
However, continued breastfeeding and any history of
formula feeding had greater impacts on specific age-groups.
Children who had continued breastfeeding
displayed significantly lower Hb concentrations and
higher rates of anaemia, both in the overall sample
and among children aged 12 to 17 months or 18
to 23 months. These findings are consistent with
the results of previous studies.30 31 32 Although the
importance of breastfeeding for children before the
age of 2 is widely recognised, empirical studies have
shown that prolonged breastfeeding (ie, beyond 6
months of age) is positively associated with anaemia
in children aged <2 years.31 32 Increases in total
breastfeeding duration are associated with decreases
in iron stores, implying late introduction or poor
quality of complementary foods in children, as well
as maternal anaemia.31 33 Accordingly, although there
remains a need to encourage breastfeeding, careful
monitoring of maternal and infant anaemia should
be implemented, along with timely introduction
of appropriate complementary foods to infants
by 6 months of age; maternal diets and nutritional
supplementation should also be improved.33 Children
with any history of formula feeding had a higher Hb
concentration and lower anaemia prevalence in each
age-group, as well as the overall sample, consistent
with previous findings.11 19 34 Formula feeding
protects against anaemia in children, presumably
because most commercially available formulas are
fortified with micronutrients (eg, iron).27 Children
with any history of formula feeding would have
received additional iron, which have may helped
to improve their anaemia status.11 Therefore, high-iron
formulas are recommended for infants aged
>6 months.35
In the overall sample, children with feeding
practices that minimum dietary diversity standards and children who consumed iron-rich or iron-fortified
foods were less likely to display anaemia.
These results are consistent with the findings of
studies in other rural areas of China.16 20 22 Regarding
minimum dietary diversity, the WHO recommends
that children aged 6 to 23 months receive a variety
of foods to ensure that their nutrient requirements
are met.36 A child’s needs with respect to the type
and quantity of complementary foods increase
with monthly age.37 Other studies have shown
that the addition of complementary food in
moderate amounts protects against anaemia.18 30
After 6 months of age, sources of iron for anaemia
prevention are mainly derived from complementary
foods.19 20 22 The consumption of iron-rich foods
can reduce the risk of anaemia by improving iron
storage and subsequent Hb production.19 The results
of some studies have highlighted the importance of
high-energy foods rich in iron, including beans, dark
green leafy vegetables, meat, and viscera. These foods
constitute sources of haem iron, which has better
bioavailability.18 Therefore, caregivers should receive
information concerning the importance of iron-rich
complementary foods before they begin introducing
complementary foods to their children.37
However, there is evidence that many
children in rural China do not meet the standards
for complementary feeding recommended by
the WHO.18 22 24 Family income level substantially
impacts nutritional intake.20 Although formula and
complementary foods are widely available, they
may not be prioritised in poor rural households.22
Because parents in such households often lack
nutritional knowledge, they may assume that
nutrient deficiency is unlikely; this belief can
lead to inappropriate feeding in many children.20
Therefore, active intervention is needed; effective
communication methods should be established to
provide nutritional health knowledge and social
support for family nutrition.
Limitations
This study had several important limitations. First, we
could not determine whether seasonal or temporal
factors were associated with anaemia. Although we
had some seasonal and temporal data regarding the
three survey waves, key information was unavailable;
thus, we could not confirm the findings of Luo et al.11
Second, although previous studies indicated that
anaemia during pregnancy is a risk factor for
anaemia in children,38 39 the present study lacked
data regarding maternal anaemia during pregnancy;
thus, we could not explore this relationship. Third,
we only assessed any history of formula feeding,
rather than ongoing formula feeding, which may
have led to inaccurate results. Additional studies are
needed to address these limitations.
Conclusion
Anaemia remains a severe public health problem
among children aged 6 to 23 months in rural China.
Continued breastfeeding was significantly positively
associated with anaemia prevalence, whereas any
history of formula feeding and the consumption of
iron-rich or iron-fortified foods were significantly
negatively associated with anaemia prevalence.
Although we could not make causal inferences on
the basis of findings in this cross-sectional study,
our analysis provided key information concerning
factors associated with anaemia prevalence among
children of various ages in rural China; these findings
will help to guide clinical practice and support policy
formulation.
Author contributions
Concept or design: L Zeng, W Zheng, Q Gao.
Acquisition of data: K Du, A Yue.
Analysis or interpretation of data: L Zeng, Q Gao.
Drafting of the manuscript: W Zheng, A Yue, Q Gao.
Critical revision of the manuscript for important intellectual content: Q Gao, N Qiao.
Acquisition of data: K Du, A Yue.
Analysis or interpretation of data: L Zeng, Q Gao.
Drafting of the manuscript: W Zheng, A Yue, Q Gao.
Critical revision of the manuscript for important intellectual content: Q Gao, N Qiao.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
We thank the enumerators for their contribution to data
collection.
Funding/support
This research was supported by the 111 Project (Grant No.: B16031), the National Social Science Foundation of China
(Grant No.: 22BGL212), the National Natural Science
Foundation of China (Grant No.: 72203134), and the Special
Project of Philosophy and Social Science Research in Shaanxi
Province (Grant No.: 2023QN0058). The funders had no role
in study design, data collection/analysis/interpretation, or
manuscript preparation.
Ethics approval
This study protocol was approved by the Sichuan University Institutional Review Board of China (Protocol ID: 2013005-01). All caregivers of the children under investigation provided
oral informed consent before participating in this study.
References
1. McLean E, Cogswell M, Egli I, Wojdyla D, de Benoist B. Worldwide prevalence of anaemia, WHO Vitamin and
Mineral Nutrition Information System, 1993-2005. Public
Health Nutr 2009;12:444-54. Crossref
2. Tolentino K, Friedman JF. An update on anemia in less developed countries. Am J Trop Med Hyg 2007;77:44-51.Crossref
3. Balarajan Y, Ramakrishnan U, Ozaltin E, Shankar AH, Subramanian SV. Anaemia in low-income and middle-income
countries. Lancet 2011;378:2123-35. Crossref
4. World Health Organization. Anaemia. Available from: https://www.who.int/health-topics/anaemia#tab=tab_1. Accessed
17 May 2023.
5. Wang L, Sun Y, Liu B, et al. Is infant/toddler anemia a problem across rural China? A mixed-methods analysis.
Int J Environ Res Public Health 2018;15:1825. Crossref
6. Lozoff B, Smith JB, Kaciroti N, Clark KM, Guevara S, Jimenez E. Functional significance of early-life iron deficiency: outcomes at 25 years. J Pediatr 2013;163:1260-6. Crossref
7. Deng X. Effects of iron deficiency anemia on physical development, intelligent behavior development and sleep quality of infants [in Chinese]. Pract Clin Med 2019;4:719-81.
8. Jin D, Zhuo Y, Hu L, Ruan D. Influence of iron deficiency anemia on intelligence of infants aged 6 to 36 months [in Chinese]. Chin J Woman Child Health Res 2019;30:281-3.
9. Zhang B. Analysis of the prevalence of anemia in infants and young children and the causes of transformation in a community in Shanghai [in Chinese]. Shanghai Med Pharm J 2019;40:61-2.
10. Wang L, Liang W, Zhang S, et al. Are infant/toddler developmental delays a problem across rural China? J Comp Econ 2019;47:458-69. Crossref
11. Luo R, Shi Y, Zhou H, et al. Anemia and feeding practices among infants in rural Shaanxi province in China. Nutrients 2014;6:5975-91. Crossref
12. Nie J, Yang J, Zhang L, Li Y, Yang J. Current situation and influencing factors of anemia in infants in poor rural areas in western China. J East China Norm Univ Sci 2019;37:58-69.
13. The State Council Information Office of the People’s
Republic of China. Circular of the General Office of
the State Council on the Issuance of China’s Food and
Nutrition Development Program (2017-2030) [in Chinese].
State Office 2017. Available from: http://www.scio.gov.cn/xwfbh/xwbfbh/wqfbh/42311/44583/xgzc44589/Document/1695253/1695253.htm Accessed 9 Sep 2021.
14. Gao W, Yan H, Wang D, Dang S, Pei L. Severity of anemia among children under 36 months old in rural western
China. PLoS One 2013;8:e62883. Crossref
15. Chen L, Li Y, Li Y, Yang F, Bi X. Iron deficiency anemia
status and influencing factors among children aged 6 to
23 months in rural minority areas in Yunnan [in Chinese].
Chin J Child Health Care 2017;25:85-7.
16. Huang Y, Wang L, Huo J, et al. Prevalence and causes of anaemia in children aged 6-23 months in rural Qinghai,
China: findings from a cross-sectional study. BMJ Open
2019;9:e031021. Crossref
17. Yang Y, Liu L, Yang W, Zhang S, Wang Y. State and influencing factors for anemia of infants aged 0-18 months
in rural area of Shaanxi province [in Chinese]. Matern
Child Health Care China 2013;28:1897-9.
18. Luo RF, Liang X, Liu CF, Zhang LX, Yue A. Risk factors for anemia in infants aged 6-12 months from rural areas
of southern Shaanxi Province, China [in Chinese]. Chin J
Contemp Pediatr 2016;18:736-41.
19. Sun S, Wu Y, Chen Y, Hao G, Zhou H. Analysis of the
influencing factors of infant anemia in underdeveloped
rural areas of southern Shaanxi [in Chinese]. Chin J Dis Control Prev 2015;19:1138-41.
20. Zhou X, Fang JQ, Luo JY, et al. Prevalence and influencing factors of anemia among 6-23 months old children in poor rural areas [in Chinese]. Chin J Public Health 2017;33:1302-5.
21. Xin QQ, Chen BW, Yin DL, et al. Prevalence of anemia and its risk factors among children under 36 months old in
China. J Trop Pediatr 2017;63:36-42. Crossref
22. Hipgrave DB, Fu X, Zhou H, et al. Poor complementary
feeding practices and high anaemia prevalence among
infants and young children in rural central and western
China. Eur J Clin Nutr 2014;68:916-24. Crossref
23. Shaanxi Provincial Bureau of Statistics. Shaanxi statistical yearbook [in Chinese]. 2016. Available from: http://tjj.shaanxi.gov.cn/tjsj/ndsj/tjnj/sxtjnj/index.html?2016. Accessed 17 May 2023.
24. World Health Organization. Indicators for assessing infant
and young child feeding practices (Part I—definitions).
Conclusions of a consensus meeting held 6-8 November
2007 in Washington, DC, USA. 2008. Available from: https://apps.who.int/iris/bitstream/handle/10665/43895/9789241596664_eng.pdf;jsessionid=96860366C0058393F12BC11CE25498BA?sequence=1 . Accessed 23 Dec 2021.
25. Seguin P, Kleiber A, Chanavaz C, Morcet J, Mallédant Y. Determination of capillary hemoglobin levels using the
HemoCue system in intensive care patients. J Crit Care
2011;26:423-7. Crossref
26. World Health Organization. Haemoglobin concentrations
for the diagnosis of anaemia and assessment of severity.
2011. Available from: https://apps.who.int/iris/bitstream/handle/10665/85839/WHO_NMH_NHD_MNM_11.1_eng.pdf?sequence=22&isAllowed=y . Accessed 4 Jul 2023.
27. Huang Z, Jiang FX, Li J, Jiang D, Xiao TG, Zeng JH.
Prevalence and risk factors of anemia among children aged
6-23 months in Huaihua, Hunan Province. BMC Public
Health 2018;18:1267. Crossref
28. Huo J, Sun J, Fang Z, et al. Effect of home-based complementary food fortification on prevalence of anemia
among infants and young children aged 6 to 23 months in
poor rural regions of China. Food Nutr Bull 2015;36:405-14. Crossref
29. Li H, Xiao J, Liao M, et al. Anemia prevalence, severity and associated factors among children aged 6-71 months in rural Hunan Province, China: a community-based cross-sectional
study. BMC Public Health 2020;20:989. Crossref
30. Hopkins D, Emmett P, Steer C, Rogers I, Noble S, Emond A. Infant feeding in the second 6 months of life related to iron
status: an observational study. Arch Dis Child 2007;92:850-4. Crossref
31. Hu S, Tan H, Peng A, et al. Disparity of anemia prevalence
and associated factors among rural to urban migrant and
the local children under two years old: a population based
cross-sectional study in Pinghu, China. BMC Public Health
2014;14:601. Crossref
32. Wu LX, Wang PW, Liu S, Li SY, Yan H, Zuo D. Analysis on breast feeding and anemia status among infants under
2 years old in rural areas of Hubei province [in Chinese].
Chin J Child Health Care 2013;21:1175-7.
33. Meinzen-Derr JK, Guerrero ML, Altaye M, Ortega-Gallegos H, Ruiz-Palacios GM, Morrow AL. Risk of infant
anemia is associated with exclusive breast-feeding and
maternal anemia in a Mexican cohort. J Nutr 2006;136:452-8. Crossref
34. Dong C, Ge P, Zhang C, et al. Effects of different feeding practices at 0 to 6 months and living economic conditions on anemia prevalence of infants and young children [in Chinese]. J Hyg Res 2013;42:596-9.
35. Vendt N, Grünberg H, Leedo S, Tillmann V, Talvik T.
Prevalence and causes of iron deficiency anemias in
infants aged 9 to 12 months in Estonia. Medicina (Kaunas)
2007;43:947-52. Crossref
36. World Health Organization. Indicators for assessing
infant and young child feeding practices: definitions and
measurement methods. 2021. Available from: https://www.who.int/publications/i/item/9789240018389. Accessed 20 Sep 2021.
37. Lu P, Wang J, Jiang W, et al. Feeding status of 0~23-month-old infants in poor rural areas of Gansu Province from 2018 to 2019 [in Chinese]. Wei Sheng Yan Jiu 2020;49:731-43.
38. Wang L. Investigation on risk factors of iron deficiency anemia in infants [in Chinese]. Chin J Woman Child Health Res 2017;(S4):434-5.
39. Shukla AK, Srivastava S, Verma G. Effect of maternal anemia on the status of iron stores in infants: a cohort study. J Family Community Med 2019;26:118-22. Crossref