© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Characteristics of individuals who frequently use
emergency departments in Hong Kong: a region-based cohort study
Peter YT Ng, MB, ChB1; CT Lui, FHKAM (Emergency Medicine), FRCEM2; CL Lau, FHKAM (Emergency Medicine), FRCEM2; HT Fung, FHKAM (Emergency Medicine), FRCEM2; CH Lai, MRCSEd, FHKAM (Emergency Medicine)1; LY Lee, FHKAM (Emergency Medicine), FRCEM1
1 Accident and Emergency Department, Tin Shui Wai Hospital, Hong Kong SAR, China
2 Accident and Emergency Department, Tuen Mun Hospital, Hong Kong SAR, China
Corresponding author: Dr Peter YT Ng (pyt.ng@ha.org.hk)
Abstract
Introduction: This study analysed the characteristics and healthcare needs of emergency department
(ED) users, and identified factors that contribute to
frequent ED use.
Methods: Using the Clinical Data Analysis and
Reporting System of the Hospital Authority, we
identified all patients and visits to three EDs in the
New Territories West Cluster from 1 April 2018 to
31 March 2019. Individuals with 4 to 9 ED visits and
≥10 ED visits were defined as frequent users (FUs)
and high-intensity users (HIUs), respectively; they
were compared with normal users (NUs, 1-3 visits)
in terms of demographics, underlying disease, and
outcomes. Visits by these users were also compared
in terms of demographics, urgency, investigations
performed, nature of complaint, and admission
statistics.
Results: In total, FUs and HIUs constituted 9%
of ED users but represented 27.2% of all visits.
Compared with NUs, FUs and HIUs were older,
more likely to have a payment exemption, and more
likely to have underlying physical and mental health
disorders. Compared with NUs, FUs were more
likely to require ambulance services (17.9% vs 23.9%; P<0.001), be triaged as urgent or above (31.8% vs
38.1%; P^lt;0.001), and require hospitalisation (28.5%
vs 35.7%; P<0.001).
Conclusion: Individuals who frequently use EDs are
more likely to be in poor health and require medical
attention. Additional community- or ED-based
support systems for discharge planning and support,
along with reduced barriers to alternative sources of
care, would improve health in these individuals and
help reduce ED utilisation burden.
New knowledge added by this study
- Frequent users and high-intensity users constituted 9% of emergency department (ED) users but represented 27.2% of all ED visits.
- Frequent users had more underlying physical and mental health disorders; they were more likely to require timely medical care and hospitalisation.
- Interventions targeting frequent users and high-intensity users could help reduce their ED visits.
- There are numerous potential interventions to reduce ED usage.
Introduction
Healthcare spending in Hong Kong continues to
grow, as demonstrated by an 8.6% increase (to
HK$69.7 billion [US$8.99 billion]) from fiscal year
2018 to fiscal year 2019.1 According to internal
statistics drawn from the Clinical Data Analysis
and Reporting System of the Hospital Authority
(HA), the annual number of emergency department
(ED) visits in all public EDs in the New Territories
West Cluster increased by 11.5% (to 410 707)
between 2018-19 and 2019-20. Similar trends have
been observed in many industrialised countries.2
Moreover, the proportion of older adults (age ≥65 years) is projected to increase from 17.2% in 2019
to 25.1% in 2029.3 The increasing demand for ED
services may result in diminished quality of care and
negative outcomes for vulnerable patients.
Frequent ED use is often regarded as a major
component of ED utilisation burden. Substantial
gaps remain in research concerning individuals
who frequently use EDs in Hong Kong. Efforts to
understand this population and the impacts of
frequent use on ED utilisation burden are needed to
identify interventions that can improve healthcare
delivery, both in and out of the EDs.
This region-based study analysed individuals who frequently used public EDs and explored
specific interventions that may reduce ED visits by
these patients.
Methods
Study setting and population
This multi-centre retrospective cohort study analysed ED visits from all acute care hospitals located
within the New Territories West Cluster (serving a
population of 1.14 million in 20183). During the study
period, only three EDs (in Tuen Mun Hospital, Pok
Oi Hospital, and Tin Shui Wai Hospital4) provided
acute emergency care in this region. All three EDs are
public and managed by the HA, the statutory body
that manages all public hospitals in Hong Kong. In
the study region, individuals who called ambulances
were typically taken to one of these three EDs.
The study population included all patients,
regardless of age, who visited any of these three EDs
during the fiscal year from 1 April 2018 to 31 March
2019. Patients without acceptable identification
documents were excluded.
Definitions
Usage classes were defined according to the total
number of ED visits by an individual patient to any
of the 18 public EDs in Hong Kong5 during the study
period, using cut-off values commonly reported in
the literature to facilitate comparison6: normal users (NUs) had ≤3 visits,6 frequent users (FUs) had 4 to 9 visits,6 and high-intensity users (HIUs) had ≥10 visits.7
Two additional groups were defined: non-ED
users had no ED visits over a 12-month period,
whereas superusers had very high numbers of ED
visits (≥35 over a 12-month period, almost 1 visit
every 10 days).
Data collection and analysis
Data were collected from the Clinical Data Analysis
and Reporting System of the HA, a comprehensive
electronic patient database that includes patient
demographics, diagnoses, surgical records, ED
visits, hospitalisation episodes, and radiological
investigations from all public hospitals and most
public clinics in Hong Kong. It allows episode-based
and patient-based analyses according to user-defined
criteria. For this study, multiple visits were linked
using a unique record linkage number. Population
demographic data were obtained from the 2016
Population By-census8 and other official government
statistics.3 9
Two dimensions of analysis were performed on
the three classes NUs, FUs, and HIUs: patient-based
and episode-based, in which patients and individual
visits were the respective units of analysis.
Patient-based analysis
Demographic variables were assigned based on
values reported at the index visit; they included age,
ethnicity (Chinese/non-Chinese), sex (male/female),
institutionalisation (residency in an old-age home
or not), and ED payment status (exempt or not).
In Hong Kong, identity card holders and residents
aged <11 years are charged HK$180 (US$23.2) per
ED visit. Civil servants and their family members,
individuals receiving social security assistance
from the government, and individuals in vulnerable
groups (low income, chronically ill, and older adults
with minimal income/assets) are exempt from the
requirement to pay for ED visits. To evaluate ED
utilisation trends, data were retrieved regarding
utilisation in the 12-month period before the study.
In Hong Kong, all hospital admissions and
ED visits (excluding patients who leave before
consultation) are coded using an appropriate
International Classification of Diseases, Ninth
Revision (ICD-9) diagnosis recommended by the
World Health Organization.9 A list of diagnoses
that represent chronic conditions with significant
morbidity was compiled and classified into
nine categories with reference to ICD-9 (online supplementary Appendix 1).9 All in-patient
procedures, except minor bedside and clinical
procedures, are also appropriately coded and
classified as minor, intermediate, major, or ultra-major10;
they are then divided into elective and emergency categories. These coding processes,
and the processes described below, are routine
procedures that undergo strict internal auditing
for completeness and accuracy. This study analysed
ICD-9 diagnosis codes, as well as major and ultra-major
procedure records, from hospital and clinic
encounters in the 5 years prior to the study period.
The full list of major and ultra-major operations
included in the current study is mostly based on the
HA’s List of Private Services.10
Deaths occurring in Hong Kong were retrieved
from the Hong Kong Death Register. Two-year
mortality was defined as death from any cause
between 1 April 2018 and 31 March 2020.
Episode-based analysis
Variables in the episode-based analysis included age, ambulance utilisation, triage category (in descending
order of urgency: critical, emergency, urgent, semi-urgent,
and non-urgent), imaging performed in ED
(plain radiography and computed tomography), and
visit details (to be discussed below). Admission rates
and median length of stay for admitted patients were
calculated.
For each episode, the attending specialty,
trauma status, and ICD-9 diagnosis or chief
complaint were recorded by the attending
emergency physician. The attending specialty was
regarded as the specialty to which a patient’s chief
complaint belongs. Four main specialties (medicine
and geriatrics, general surgery, orthopaedics, and
paediatrics) were included in the data analysis.
The ICD-9 diagnosis codes were grouped into
musculoskeletal pain (eg, joint pain, cervicalgia,
and lumbago) and minor infections (eg, acute upper
respiratory tract infection). A full list of diagnoses
within each of these two categories is included in
online supplementary Appendix 2.9
Statistical analysis
Descriptive statistics were compiled for the
demographic characteristics of non-ED users, NUs,
FUs, and HIUs, with reference to data from the 2016
Population By-census.8 Age-specific distributions
of ED visits and numbers of ED visits per capita
were analysed. In the patient-based analysis,
demographic and clinical characteristics of NUs,
FUs, and HIUs were compared by univariate analysis
with appropriate statistical tests. The episode-based
analysis compared age distribution, ambulance use,
triage category, investigations performed, principal
diagnosis during each ED visit, and admission
statistics among NUs, FUs, and HIUs. The clinical
and demographic characteristics of superusers were
also analysed.
Two models were used to identify independent
predictors of FU and HIU statuses, compared
with NU status and specific numbers of ED visits. Multinomial logistic regression was conducted,
using the patient as the unit of analysis, to compare
the FU and HIU groups with the reference group.
Zero-truncated Poisson regression was performed
to predict the independent association of each
predictor with the number of ED visits. All bivariate
predictors associated with the outcome (P<0.1)
were entered into the model and used as categorical
variables. Age-stratified subgroup analysis (≤17
years, 18-64 years, and ≥65 years) was performed
to identify independent predictors of FU and HIU
statuses in each age-group. P<0.05 was regarded
as the threshold for statistical significance in all
analyses. Zero-truncated Poisson regression was
performed with R11 with vector generalised linear
and additive model.12 All other statistical analyses were conducted using SPSS (Windows version 25.0;
IBM Corp, Armonk [NY], United States).
Results
As shown in the Figure, the number of per capita ED
visits was the highest in the youngest and oldest
age-groups (0.66 for age 0-4 years and 1.02 for age
≥85 years); patients aged 10 to 54 years had a stable
and low number of per capita ED visits (<0.3).
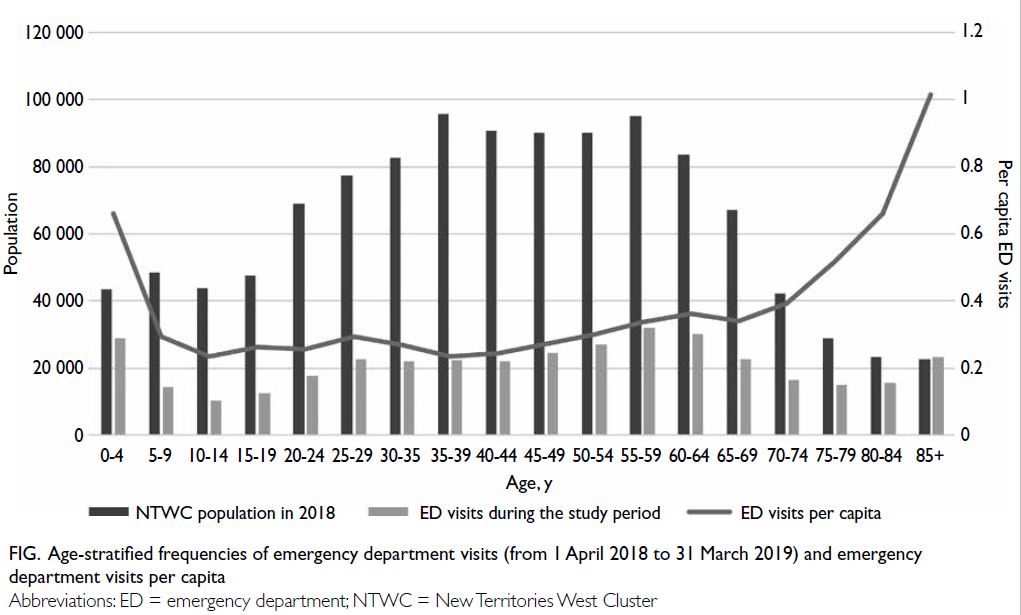
Figure. Age-stratified frequencies of emergency department visits (from 1 April 2018 to 31 March 2019) and emergency department visits per capita
During the study period, 215 862 patients
with valid identity documents accessed EDs in the
study region; there were 371 915 visits in total (Table 1). Frequent users and HIUs constituted small percentages of the total number of patients (8.2%
and 0.8%, respectively), but they represented larger
percentages of visits (21.3% and 5.9%, respectively).
The total number of ED visits by a single HIU ranged
from 10 to 263.
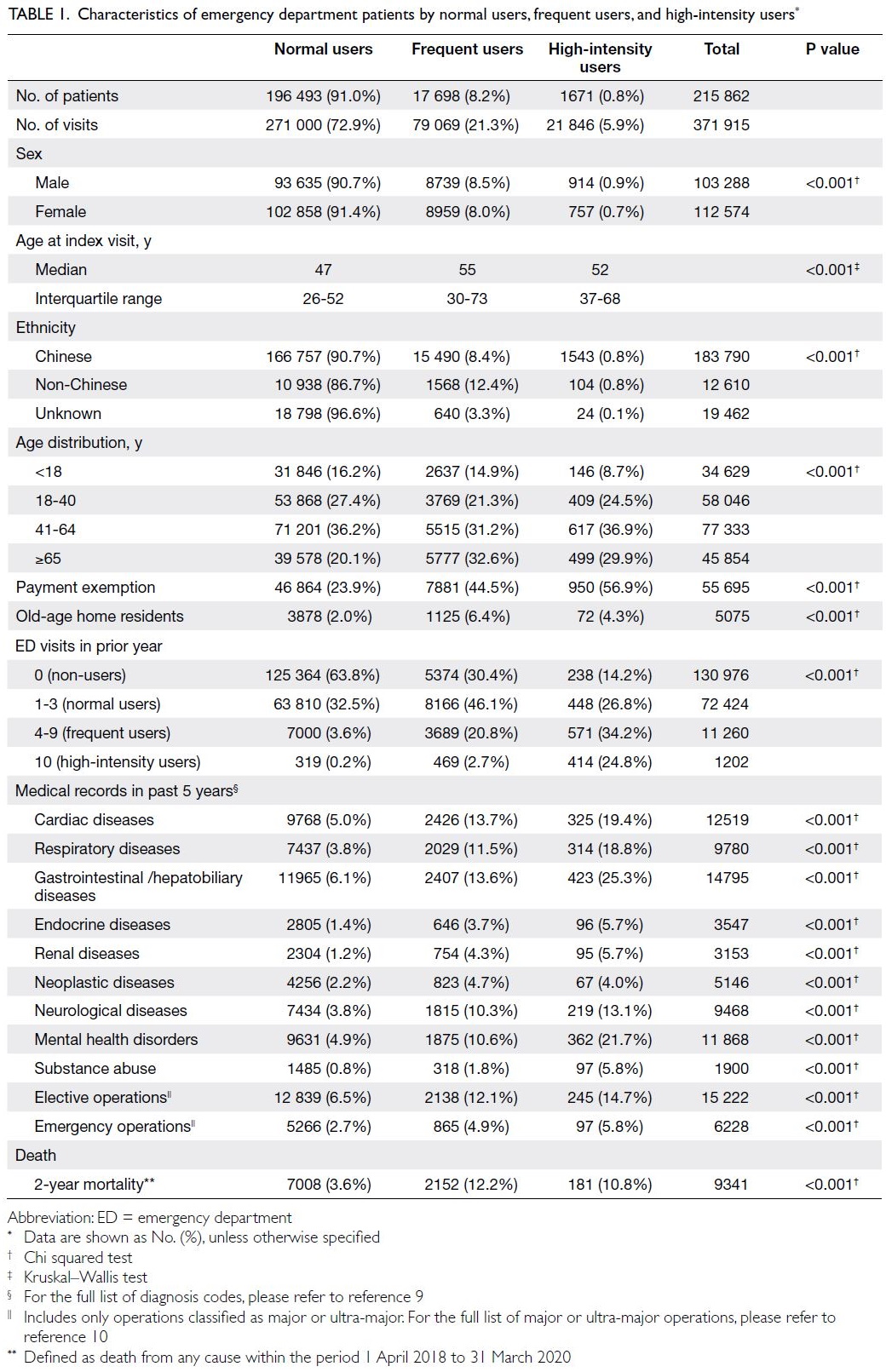
Table 1. Characteristics of emergency department patients by normal users, frequent users, and high-intensity users
Compared with NUs (median age, 47
years), FUs and HIUs were older (55 and 52 years,
respectively). Frequent users and HIUs more often
had underlying chronic illnesses, such as cardiac,
respiratory, neurological, and gastrointestinal/hepatobiliary diseases. Mental health disorders and
substance abuse were also much more prevalent
among FUs and HIUs. Moreover, 23.5% and 59.0% of
FUs and HIUs were FUs or HIUs in the previous year,
implying habitual attendance behaviour. Frequent
users and HIUs also had higher all-cause mortality
rates, compared with NUs.
Reasons for ED visits differed among NUs, FUs,
and HIUs (Table 2). Normal users were much more
likely to visit the ED for an injury, whereas primary
diagnoses related to musculoskeletal pain were more
common in HIUs. Levels of urgency on presentation
also differed among NUs, FUs, and HIUs. More
visits by FUs were triaged as critical, emergency, or
urgent (38.1%), compared with visits by NUs (31.8%).
However, a lower percentage of visits by HIUs were
triaged as urgent or above (28.6%), compared with
visits by NUs; more HIUs attended EDs by calling an
ambulance (HIUs: 21.2% vs NUs: 17.9%).
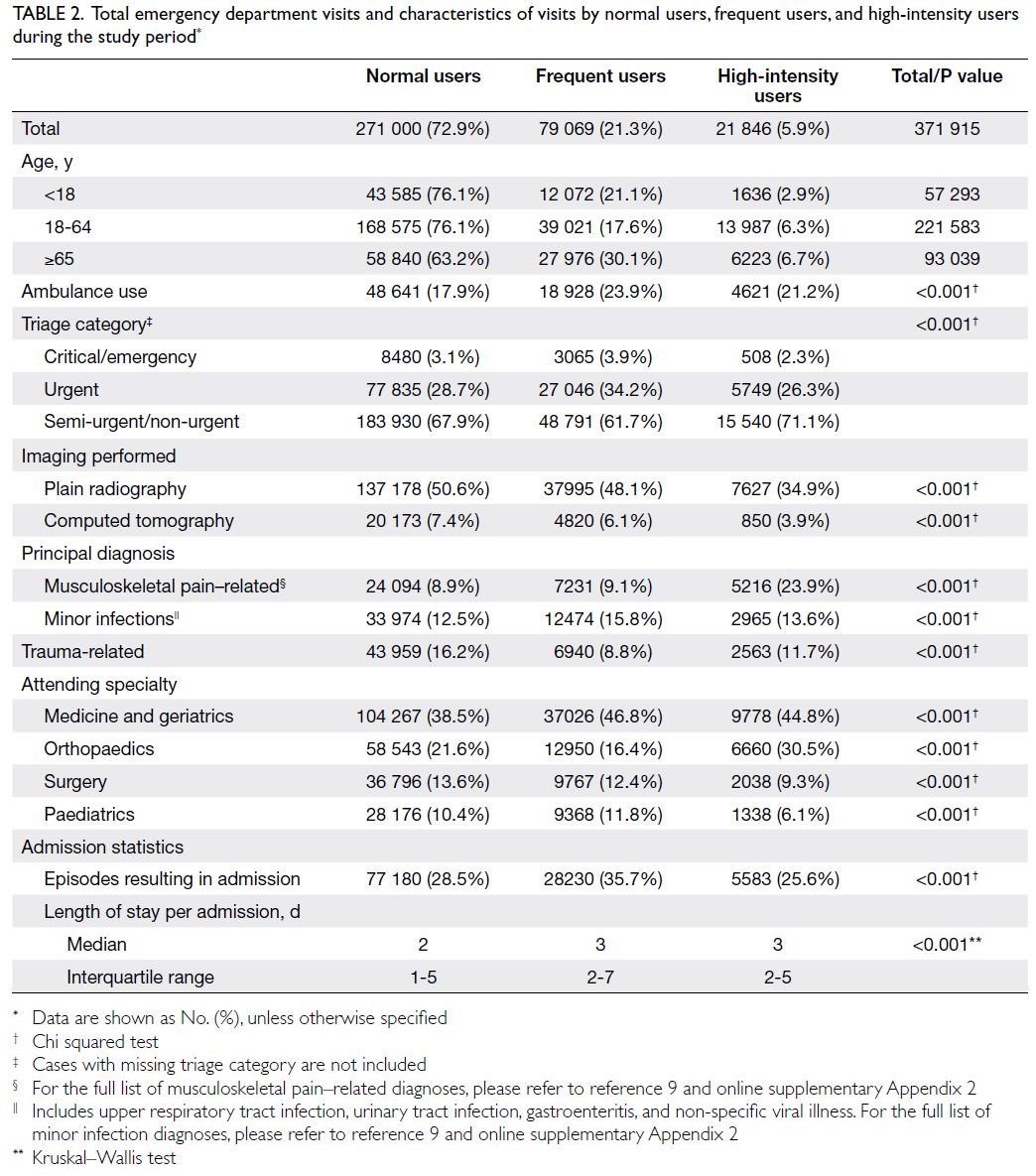
Table 2. Total emergency department visits and characteristics of visits by normal users, frequent users, and high-intensity users during the study period
Multinomial logistic regression and zero-truncated
Poisson regression showed similar
independent predictors of FU and HIU statuses
(Table 3). Payment exemption and number of visits
in the prior year were the strongest predictors.
Residency in an old-age home was a risk factor
for FU status (adjusted odds ratio [OR]=1.131)
but a protective factor for HIU status (adjusted
OR=0.48). Non-Chinese ethnicity, pre-existing
systemic diseases including cardiac, respiratory,
gastrointestinal/hepatobiliary and renal, mental
health disorders, and substance abuse were risk
factors for frequent ED use. Age-stratified analysis
(Table 4) showed similar predictors among the three
groups. Respiratory diseases and gastrointestinal/hepatobiliary diseases were prevalent in paediatric
FUs; neurological diseases and mental health
disorders were prevalent in both paediatric FUs
and paediatric HIUs. Non-Chinese ethnicity was a
risk factor for FU and HIU statuses among patients
aged <18 years (adjusted ORs=1.949 and 2.107,
respectively), but it was not associated with ED use
in older patients (age >64 years).
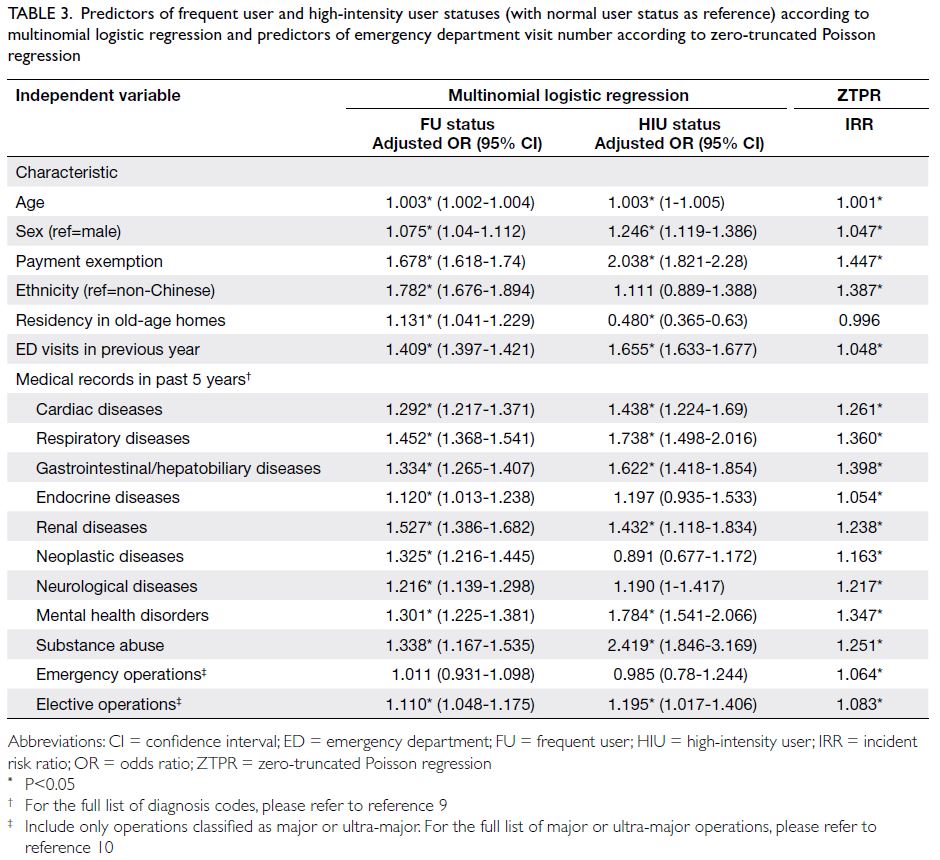
Table 3. Predictors of frequent user and high-intensity user statuses (with normal user status as reference) according to multinomial logistic regression and predictors of emergency department visit number according to zero-truncated Poisson regression
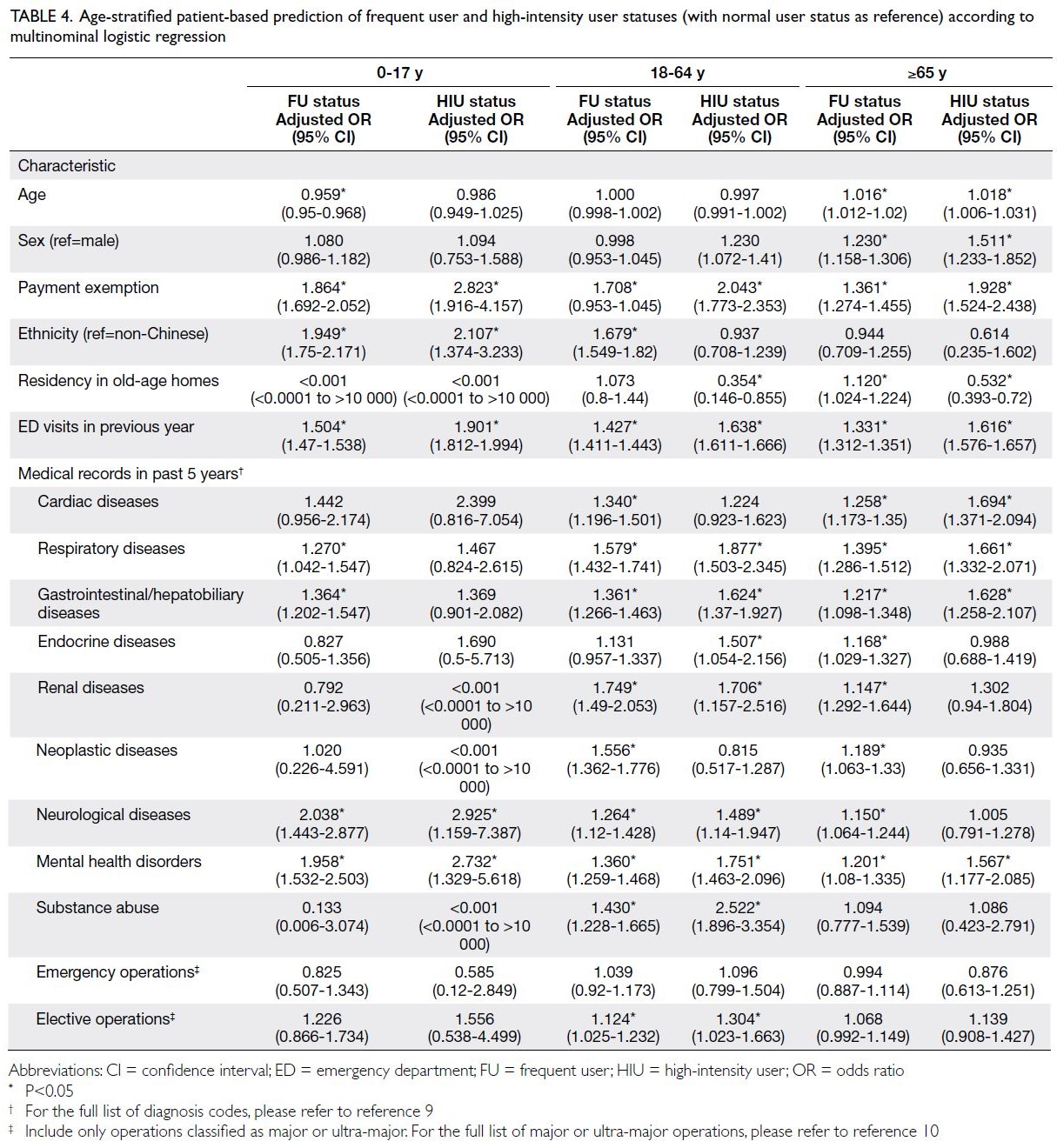
Table 4. Age-stratified patient-based prediction of frequent user and high-intensity user statuses (with normal user status as reference) according to multinominal logistic regression
Superusers had particularly high prevalences of
mental health disorders (26.9%) and gastrointestinal/hepatobiliary diseases (36.5%) [Table 5]. Many of
their visits were less serious or complex, compared
with visits by NUs, FUs, and HIUs. Only 9.4% of
visits by superusers required the use of ambulance
services. Most visits by superusers were triaged as
semi-urgent or non-urgent (90.9%). Musculoskeletal
pain and minor infections represented 54.3% of the
principal diagnoses for superusers.
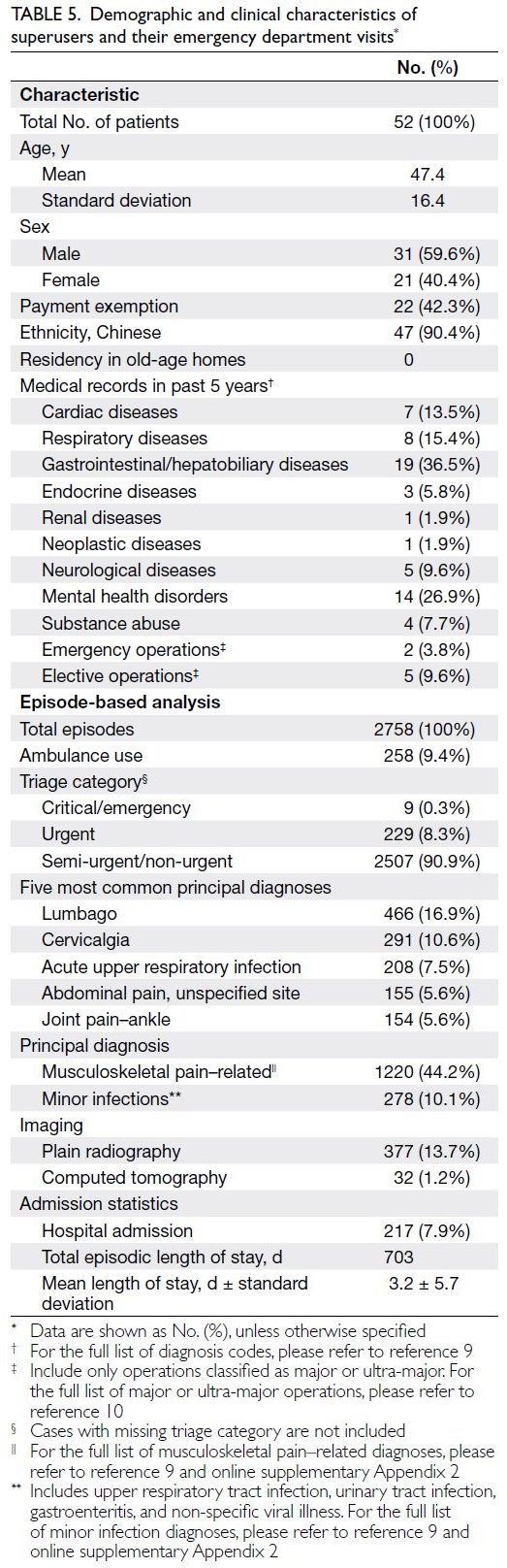
Table 5. Demographic and clinical characteristics of superusers and their emergency department visits
Discussion
Frequent emergency department utilisation
and health needs
The characteristics of individuals who frequently
use EDs in Hong Kong have not been extensively
investigated. Frequent users and HIUs constituted 9%
of all ED patients and represented 27.2% of all visits.
Region-based studies in developed countries have
revealed similar findings.6 7 13 14 15 16 Although frequent ED
use is often assumed to indicate inappropriate use,
our data do not support this assumption. The health
statuses and presentation conditions of FUs strongly
suggest that these individuals have greater health
needs than the rest of the population. Frequent users
were more likely to have underlying illnesses, require
ambulance services, have visits triaged as urgent or
above, require hospital admission, and have a longer
length of hospitalisation. In contrast, HIUs had visits
triaged as less urgent, required less investigations,
often attended for conditions (eg, musculoskeletal
pain and minor infections) that could potentially
be managed in primary care clinics, and had lower
admission rates compared with both NUs and FUs.
These trends were much more pronounced among
superusers.
Improving healthcare delivery services and primary care
High percentages of visits involved musculoskeletal
pain and minor infections, conditions that could
potentially be managed in primary care clinics. Such
visits could be related to a misunderstanding of ED function, a misperception of condition severity, or
use of the ED as a substitute for unavailable forms
of care. Policies to decrease ED utilisation burden
should focus on improving healthcare delivery
services and primary care; such policies are likely to
benefit NUs with similar needs. Recent advances in
information technology and the widespread use of
smartphones offer many opportunities to improve
information dissemination and increase accessibility
to alternative sources of care.
Effective policies targeting ethnic minorities
Our findings suggest disproportionate use of ED services by ethnic minorities. The number of Hong
Kong residents of non-Chinese ethnicity rose by
70% over a 10-year period; they constituted 8% of
the total population in 2016.8 The Chinese literacy
rate was <20% in some age-groups.8 More frequent
ED use may result from language barriers to access
of care, limited knowledge of local healthcare
alternatives, or cultural differences in health-seeking
behaviour. Effective policy measures targeting these
populations should promote an understanding of
the local healthcare system through informative
advertisements about alternative services offered;
measures should also reduce language barriers (eg, through translator services or the provision of online
booking instructions in other languages).
Community-based interventions for frequent
users
Frequent users constitute a sicker population
requiring medical care that cannot be easily
provided in primary care clinics. They need
support to facilitate integration and maintenance
in the community, which would reduce the need
for emergency medical care at EDs. The burden
placed on EDs may be reduced by developing
new community-based support systems, such as
enhanced coverage of community nursing services
and extended service hours (eg, weekends and public
holidays); dedicated multidisciplinary teams to
provide rehabilitation services and caregiver training
in the community; and centres for the provision of
coordinated community services. Eligible geriatric
patients could benefit from a holistic community
geriatric care strategy triggered by an ED visit, with protocol-driven assessments in the ED to identify
potentially reversible risk factors for subsequent
deterioration and repeated ED visits. This strategy
should include comprehensive geriatric assessment
prior to ED discharge, focused on factors such as
fall risk, delirium screening, and frailty assessment.
In addition to physical assessments, psychosocial
assessments and support may improve patient
outcomes and minimise repeated ED visits. Pre-discharge
care planning that empowers patients and
family members to seek help from non-ED sources
may also prevent repeated ED visits. Thus far,
there remains uncertainty about the effectiveness
of community-based interventions for people with
multimorbidity because of the relatively small
number of randomised controlled trials focused on
this area of healthcare.17
Case management for patients with chronic
diseases
Reformation of the chronic disease service model may improve quality of care and reduce repeated ED
visits. Patient-based care, rather than disease-based
care, may be beneficial. Patients with multimorbidity
(especially older adults) receive medical treatment
through multiple specialty or subspecialty clinics,
which can result in fragmented and duplicative
care. It is not uncommon for patients with chronic
diseases to attend the ED for minor problems and questions about their chronic diseases because they
cannot find an alternative source of medical advice.
Case management helps improve outcomes in
some chronic diseases.18 Efforts to strengthen the
abilities of primary care clinics to function as ‘case
managers’ for patients with chronic diseases may
improve quality of care and reduce the number of
ED visits.
Mental health disorders and substance abuse
In this study, mental health disorders and substance
abuse were significant predictors of frequent ED
use. A previous work indicated that one in seven
Hong Kong residents aged 16 to 75 years has anxiety,
depression, or another common mood disorder.19
The HA is the main specialist service provider for
patients with mental health disorders. It provides in-patient
facilities, day hospitals, specialist out-patient
clinics, and community outreach services. The HA is
experiencing increased demand for specialist mental
health services,20 which may be causing patients
to use EDs instead. Emergency department visits
and readmissions for psychiatric problems may be
reduced by reforming the current service model
to expand community psychiatric services, with a
focus on personalised care for psychiatric patients
and their caregivers through a case management
approach that facilitates community re-integration
and strengthens recovery. Enhanced screening to
identify early features of mental health disorders
may allow earlier detection and treatment, thereby
reducing ED utilisation. Patients and caregivers
should receive education about health-seeking
behaviours during instances of acute deterioration
(eg, using a 24-hour psychiatric advisory hotline
or undergoing urgent assessment at a psychiatric
specialist out-patient clinic), rather than simply
using the ED as a safety net.
Limitations
This study was limited to the three EDs in the New
Territories West Cluster. Its findings may not be
generalisable to other regions in Hong Kong with
different demographics, health-seeking behaviours,
and socio-economic statuses. Also, this study only
investigated ED visits within a specific time period
and did not consider past or future periods. Thus, it
may have underestimated ED visits for patients who
were born or died during the study period.
By reviewing diagnosis codes, we were able
to include many visits and patients in the analysis;
however, we could not analyse individual charts.
Although coding is a routine component of hospital
procedures, codes are only required for the current
condition or presenting problem. Generally, coding
is not mandatory for appointments at out-patient
clinics. This difference in coding information may
have led to underestimation of patient comorbidities.
To mitigate this possibility, we examined all
diagnosis codes from the past 5 years to acquire
a more complete representation of underlying
comorbidities.
Because this study excluded patients without
valid identification documents, homeless persons
may have been underrepresented. These individuals
potentially have a heavier disease burden and a
disproportionate share of frequent visits. The study may also have excluded visitors to Hong Kong and
individuals who do not have residency status.
Conclusion
Frequent users and HIUs are a small but diverse
population that represents a substantial proportion
of annual ED visits. Demographic factors, economic
considerations, and medical conditions all contribute
to increased numbers of ED visits. Our data suggest
that there are many opportunities for improvement
via streamlining and enhancement of healthcare
delivery to reduce ED utilisation.
Author contributions
Concept or design: PYT Ng, CT Lui.
Acquisition of data: PYT Ng, CT Lui.
Analysis or interpretation of data: PYT Ng, CT Lui.
Drafting of the manuscript: PYT Ng, CT Lui.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: PYT Ng, CT Lui.
Analysis or interpretation of data: PYT Ng, CT Lui.
Drafting of the manuscript: PYT Ng, CT Lui.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
We thank Mr Chun-ho Lam, Statistical Officer at Research Assist Team of the New Territories West Cluster of Hospital
Authority, Hong Kong, for his advice on the zero-truncated
Poisson regression model.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This research was approved by the New Territories West Cluster Research Ethics Committee of Hospital Authority,
Hong Kong (Ref No.: NTWC/REC/19081). Informed patient
consent was waived by the Committee due to the retrospective
nature of the study.
References
1. Hospital Authority, Hong Kong SAR Government. Hospital Authority annual report 2018-2019. Available
from: https://www.ha.org.hk/ho/corpcomm/AR201819/PDF/HA_Annual_Report_2018-2019.pdf. Accessed 1 May 2020.
2. Pines JM, Hilton JA, Weber EJ, et al. International perspectives on emergency department crowding. Acad Emerg Med 2011;18:1358-70. Crossref
3. Data.gov.hk, Hong Kong SAR Government. Projections of population distribution 2021-2029. Available from:
https://data.gov.hk/en-data/dataset/hk-pland-pland1-projections-of-population-distribution-2021-to-2029. Accessed 17 Jul 2023.
4. Hospital Authority, Hong Kong SAR Government. List of all accident & emergency departments. 2023. Available from: https://www.ha.org.hk/visitor/ha_visitor_index.asp?Content_ID=200246&lang=ENG. Accessed 19 Jul 2023.
5. Hospital Authority, Hong Kong SAR Government. Introduction of clusters: New Territories West Cluster.
2023. Available from: https://www.ha.org.hk/visitor/ha_visitor_index.asp?Content_ID=10181&Lang=ENG&Dimension=100&Parent_ID=10084. Accessed 19 Jul 2023.
6. Krieg C, Hudon C, Chouinard MC, Dufour I. Individual predictors of frequent emergency department use: a scoping review. BMC Health Serv Res 2016;16:594. Crossref
7. Dr Foster UK. High intensity users: reducing the burden on accident & emergency departments. Available
from: https://www.telstrahealth.com/content/dam/telstrahealth/pdf-downloads/Dr-Foster_High-Intensity-Users-Report.pdf. Accessed 10 Aug 2023.
8. 2016 Population By-census, Hong Kong SAR Government. District profiles. Available from: https://www.bycensus2016.gov.hk/en/bc-dp.html. Accessed 1 May 2020.
9. World Health Organization & International Conference for the Ninth Revision of the International Classification of Diseases. Manual of the international statistical
classification of diseases, injuries, and causes of death:
based on the recommendations of the ninth revision
conference, 1975, and adopted by the Twenty-ninth World
Health Assembly, 1975 revision. 2021. Available from:
https://apps.who.int/iris/handle/10665/40492. Accessed 19 Jul 2023.
10. Hospital Authority, Hong Kong SAR Government. Operations. List of private services. Available from:
https://www3.ha.org.hk/fnc/Operations.aspx?lang=ENG. Accessed 19 Jul 2023.
11. R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing. Available from: https://www.R-project.org/. Accessed 17 Jul 2023.
12. Yee TW. Vector generalized linear and additive models: with an implementation in R. Springer. Available from:
https://link.springer.com/book/10.1007/978-1-4939-2818-7. Accessed 17 Jul 2023. Crossref
13. Hunt KA, Weber EJ, Showstack JA, Colby DC, Callaham ML. Characteristics of frequent users of emergency departments. Ann Emerg Med 2006;48:1-8. Crossref
14. Lee WL, Chen WT, Hsiao FH, Huang CH, Huang LY. Characteristics and resource utilization associated with
frequent users of emergency departments. Emerg Med Int.
2022;2022:8064011. Crossref
15. Leporatti L, Ameri M, Trinchero C, Orcamo P, Montefiori M. Targeting frequent users of emergency
departments: prominent risk factors and policy
implications. Health Policy 2016;120:462-70. Crossref
16. Fuda KK, Immekus R. Frequent users of Massachusetts emergency departments: a statewide analysis. Ann Emerg Med 2006;48:9-16. Crossref
17. Smith SM, Wallace E, O’Dowd T, Fortin M. Interventions for improving outcomes in patients with multimorbidity in
primary care and community settings. Cochrane Database
Syst Rev 2021;1:CD006560. Crossref
18. Reilly S, Miranda-Castillo C, Malouf R, et al. Case management approaches to home support for people with
dementia. Cochrane Database Syst Rev 2015;1:CD008345. Crossref
19. Lam LC, Wong CS, Wang MJ, et al. Prevalence, psychosocial correlates and service utilization of depressive and anxiety disorders in Hong Kong: the Hong Kong Mental Morbidity
Survey (HKMMS). Soc Psychiatry Psychiatr Epidemiol
2015;50:1379-88. Crossref
20. Food and Health Bureau, Hong Kong SAR Government. Mental health review report. Available from: https://www.fhb.gov.hk/download/press_and_publications/otherinfo/180500_mhr/e_mhr_full_report.pdf. Accessed 1 May 2020.

