© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
COMMENTARY
Promoting integrated healthcare for Hong Kong
and Macau residents in the Greater Bay Area during the COVID-19 pandemic
Pearl MC Pai, MD, FRCP1,2; Joe KM Fan, MS (HKU), FRCSEd2,3; William CW Wong, MD, FRCP2,4; XF Deng, MBA5; XP Xu, MD5; CM Lo, MS (HKU), FRCSEd2,3
1 Department of Medicine, The University of Hong Kong–Shenzhen Hospital, Shenzhen, China
2 School of Clinical Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China
3 Department of Surgery, The University of Hong Kong–Shenzhen Hospital, Shenzhen, China
4 Department of Family Medicine, The University of Hong Kong–Shenzhen Hospital, Shenzhen, China
5 Clinical Service, The University of Hong Kong–Shenzhen Hospital, Shenzhen, China
Corresponding author: Dr Pearl MC Pai (ppai1@hku.hk)
The coronavirus disease 2019 (COVID-19) pandemic
has affected the world health system drastically,
almost rendering it beyond recognition. At the
height of the pandemic, many patients were unable
to access the healthcare they desperately needed
because hospitals were overwhelmed and exhausted.
Hospitals in many places have been pushed to
the edge of collapse, unable to admit patients for
essential care or provide outpatient services as part
of ongoing chronic disease management.
When the COVID-19 pandemic began in
mainland China, many permanent residents of Hong
Kong living in Guangdong Province were unable to
return home for their clinic appointments under
the Hong Kong Hospital Authority (HA) due to
quarantine and travel restrictions between Hong
Kong and mainland China. In 2020, the Government
of the Hong Kong Special Administrative Region
(HKSAR), the Shenzhen Municipal Government,
and The University of Hong Kong–Shenzhen
Hospital (HKU-SZH) agreed to initiate and operate
a HA special support scheme under which such
patients could use the clinical services available at
HKU-SZH to meet their needs.
Brief overview of The University of Hong Kong–Shenzhen Hospital and its mission
Hong Kong and Shenzhen are separated by the
Shenzhen River and are some 35 kilometres apart.
The HKU-SZH is a joint project between HKU and the
Shenzhen Municipal Government and was formed
in 2011 as part of the Chinese health reform.1 In less
than a decade, it has been awarded Australian Council
on Healthcare Standards accreditation and was
granted the status of a ‘Grade 3A’ hospital (the highest
ranking given by the national hospital accreditation
system of mainland China) as well as several other
prestigious awards. In the 2020 Development Report
on Health Reform in China,2 HKU-SZH has been noted as having been instrumental in the Chinese
health reform. In fact, this is one of the missions that
the Hospital was designed and built. Many innovative
service models have been introduced, including the
primary-secondary care interface and the package
fee for family medicine consultation; these have
subsequently drawn much attention from other
hospitals. Above all, it was expected to integrate the
best Western model of healthcare delivery with the
best Chinese model, thereby providing a socialistic
approach to medicine with Chinese characteristics.
The Hospital has been working hard on this and
making progress.
Use of Elderly Health Care Vouchers in The University of Hong Kong–Shenzhen Hospital
In 2009, the Hong Kong SAR Government established
the Elderly Health Care Voucher (EHCV) Scheme to
support its elderly residents. Those who are eligible
currently receive HK$2000 (equivalent to US$250)
per year. Since October 2015, to increase utilisation
of the Scheme, the Hong Kong SAR Government has
allowed eligible elderly patients to pay for treatment
at HKU-SZH with their EHCVs. Since its launch,
HKU-SZH has recorded over 45 000 EHCV patient
episodes or outpatient attendances. In the process,
the Hospital has established a payment mechanism
with the HA for reimbursement, which will likely be
useful in the future for similar schemes. The Scheme
is in line with the Central Government’s policy
of enabling hospitals with similar backgrounds to
provide quality healthcare for residents of Hong
Kong living in the Guangdong-Hong Kong-Macao Greater Bay Area (GBA).3
Hong Kong SAR Government’s special support scheme and its implementation
In 2020, the Hong Kong SAR Government estimated that between 18 000 to 38 000 Hong Kong residents
living in Guangdong Province were attending
HA clinics in Hong Kong for chronic disease
management.4 Because of the travel restrictions
during the COVID-19 pandemic, many of them were
unable to return to Hong Kong and had to depend
on postal delivery of their repeat prescriptions. In
late 2020, the HKSAR Government decided to set up
the HKSAR Government Special Support Scheme
for Hospital Authority Chronic Disease Patients
Living in the Guangdong Province to Sustain Their
Medical Consultation under COVID-19 (the Support
Scheme). Under the Support Scheme, patients who
had HA appointments between 17 February 2020
and 31 July 2021 and were unable to return to Hong
Kong for their HA appointments because of the
pandemic-related travel restrictions were allowed
to use the following HA outpatient services at
HKU-SZH: family medicine, medical and surgical
specialties, ophthalmology, gynaecology, oncology,
orthopaedics, paediatrics, and the pain clinics. Each
patient received 2000 yuan per year (equivalent to
US$300) which could be used to pay for outpatient
investigations and medications at designated clinics
at HKU-SZH providing clinical services offered by
the HA to carry out the Support Scheme. The expiry
date of the scheme was later extended to May 2023.
Because the HA and HKU-SZH had been
working well together under the EHCV Scheme,
HKU-SZH was invited to run the new Support
Scheme. To set up the special HKU-SZH–HA clinics,
HKU-SZH developed a smartphone application
with which patients could request an appointment.
When doing so, patients will be asked to upload their
HA appointment slips and to authorise HKU-SZH
to apply for their electronic health records and
access their personal health details from the HA.
The application is then checked at the HKU-SZH
appointment booking centre before being forwarded
to the HA electronically as encrypted data. Once the
application is processed by the HA, encrypted copies
of the patient’s eHealth file will be transmitted to
HKU-SZH where a clinic appointment is generated.
All these actions are done with the consent of the
patients and the secure storage and transmission of
the data is supported and protected by information
technology infrastructure, cybersecurity and data
security laws, and, more recently, by the Personal
Information Protection Law of China. The patients
must pay a consultation fee of 100 yuan (equivalent
to US$15), similar to mainland residents, as well as
any excess charges.
Additionally, a special telephone line and
walk-in enquiry desk with Cantonese-speaking
staff have been set up. There is also clear signage
at the outpatient reception, payment counter, and
medication collection window. The logo was designed using the HA pantone colour, which is familiar
to patients from Hong Kong. Each department at
the Hospital has selected its most suitable doctors
in terms of languages and experience to staff the
clinics. It should be noted that many of the Hospital’s
doctors have been taught and trained in mainland
China and therefore have limited English ability.
Prior to the opening of HKU-SZH–HA clinics in
November 2020, several orientation sessions were
held, including a briefing session in which the then–Hospital Chief Executive Professor Chung-mau Lo
delivered an encouraging speech. He emphasised the
importance of the Support Scheme and explained
to the doctors the usual HA clinic process and
behaviours and expectations of its patients. The
doctors were reminded of the brief nature of many
HA clinic letters, their frequent use of abbreviations,
and the use of English medication names, and that
they might need some time to become familiar with
all these.
Analysis of implementation of
The University of Hong Kong–Shenzhen Hospital-Hospital
Authority clinics: a step towards
connection and integration
The HKU-SZH conducted a performance analysis
of its HKU-SZH–HA clinics in March 2021, some
5 months after their opening. A total of 11 000
enquires and 10 938 patient episodes or clinic
attendances had been recorded in the Hospital
under the Support Scheme. The mean age of the
patients was 65.5 ± 13.5 years (range, 1-103). The
male-to-female ratio was 2.13:1. From 1 January to
31 December 2021, there were 28 386 attendances
or patient episodes (Fig a). The most utilised clinics
were the chronic disease clinic (17 414 attendances)
served by the family medicine physicians, followed
by the medical specialty clinics (7810 attendances).
Figure b shows the patient distribution among the
eight medical specialties; there was good cooperation
between the family medicine doctors and specialty
doctors for onward referral, which helped to drive up
the utilisation of these clinics. The 10 most common
conditions for which patients received treatment
were hypertension, diabetes, coronary artery
disease, ischaemic heart disease, dyslipidaemia,
aftercare of post-coronary artery stent, gout, atrial
fibrillation, chronic kidney disease, and chronic
obstructive pulmonary disease. Feedback from
doctors and patients of HKU-SZH–HA clinics was
mostly positive. Although the scope of the Support
Scheme was rather limited, it was extraordinarily
significant. It demonstrated that, despite assorted
difficulties, integrated medical care is working and
sustaining.
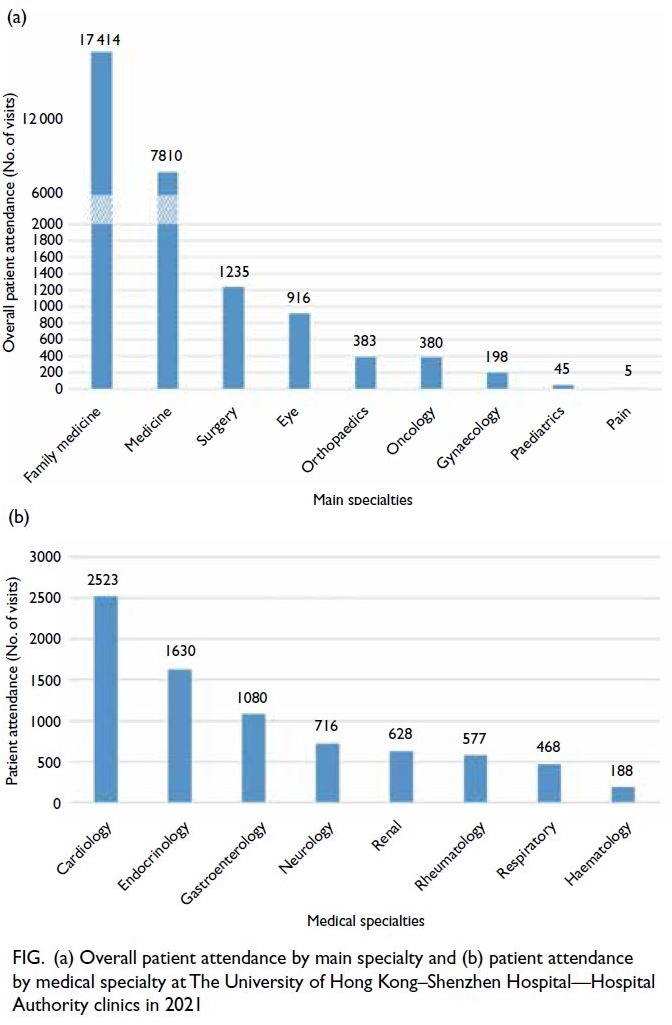
Figure. (a) Overall patient attendance by main specialty and (b) patient attendance by medical specialty at The University of Hong Kong–Shenzhen Hospital—Hospital Authority clinics in 2021
Experiences shared and humble wishes
The HA has been providing quality yet affordable,
and almost free, healthcare services to its patients
in Hong Kong. As the GBA becomes increasingly
popular as a place for work, living, and retirement
for Hong Kong residents, how could the HA health
service follow, serve, and protect them when they
venture into the GBA and beyond? Their decision
whether to relocate to a new residing place in the
GBA or not would be very much influenced by the
availability and affordability of healthcare there. The
successful management of the EHCV Scheme and
the Support Scheme by HKU-SZH indicates possible
directions for the future, but the additional funding
or support required for implementation of similar schemes might be very costly and warrant serious consideration.
If we were to improve the integrated healthcare
delivery at HKU-SZH, the highest priorities would
be to streamline the application process for patients,
speed up the transmission of patient records between
healthcare providers in Hong Kong and Shenzhen,
and enable mutual recognition of laboratory and
radiology reports to avoid duplicated tests and waste.
Government plans to connect and
integrate medical services in the Greater Bay Area
In October 2020, the General Office of the Chinese
State Council proclaimed a directive entitled
‘Implementation Plans on Building Shenzhen into a
Pilot Demonstration Zone of Socialism with Chinese
Characteristics’.3 The title is clear enough to convey
to the nation what the Central Government wants
from and for the nation itself and its people—a
model of a modern metropolis within a strong
nation under socialism with Chinese characteristics,
of which a world-leading health service is an
indispensable component. Answering its call, the
Shenzhen Municipal Government released its own
guideline and the ‘Implementation Plan for the
Pilot Comprehensive Reform of Building a Pilot
Demonstration Zone of Socialism with Chinese
Characteristics in Shenzhen’ (the ‘Pilot Reforms
Plan’) to coincide with its 40th anniversary as a
Special Economic Zone. Among the most important
purposes of the ‘Pilot Reforms Plan’ is to increase
cross-border connection and integration of medical
services between Hong Kong and Shenzhen, as well
as any other borders in the GBA.5 In short, this is
another ‘open for reform’ following the one launched
in 1978. In its 11 measures, it asks both sides of the
border to relieve the congestion of healthcare in
the GBA; promote better circulation of healthcare
resources; allow Shenzhen residents to access
good and qualified Hong Kong doctors; enable the
use of advanced medications from Hong Kong;
allow Hong Kong and Macau residents to receive
good healthcare in mainland China; simplify the
transfer of patients across the border; speed up the
evaluation process and approval of health projects;
and publicise the successful work of HKU-SZH
under the special Support Scheme and the EHCV
scheme and its successful payment mechanism.
Hopefully as a result, other approved hospitals in
Shenzhen may join the integrated medical services
and utilise the payment mechanism to provide good
and reliable services to Hong Kong residents and
their families living in Shenzhen and GBA in the
future. Together, the Directive and the Pilot Reforms
Plan have covered cross-border connection and
integration in every sector of healthcare, extending
from teaching, training, and practice of healthcare workers to medications and hospital management.
Here, in the 11 measures mandated, as the challenges
for connection and integration have been itemised,
something can be done to meet them.
Connection and integration achieved
Following the proclamation of the Directive and
the Pilot Reforms Plan, and under pressure from
the pandemic, the following practical actions
have taken place. In August 2021, Shenzhen had
accredited and granted 37 senior doctors working in
HKU-SZH and from Hong Kong the Chinese title of
chief physician.6 It marked the first time Shenzhen
had awarded this senior professional title to Hong
Kong doctors working in the city. Similarly, the HKU
School of Clinical Medicine has awarded honorary
titles, such as associate professorships, to doctors
from mainland China working in HKU-SZH. These
actions have demonstrated some mutual recognition
of medical qualifications and competencies.
Additionally, the Shenzhen Health Commission
has granted limited medical registration to several
doctors from Hong Kong and Macau allowing them
to practise locally. The implementation of the ‘Hong
Kong and Macau Medicines and Devices policy’7 in
November 2021 has been another effort to provide
integrated healthcare for Hong Kong and Macau
residents living in the GBA. Up to May 2023, under
the special permit, 20 drugs and 11 medical devices
and reagents have been approved and imported by
HKU-SZH for use. It has shared its experience with
four other pilot hospitals in the GBA. It has also been
asked to develop a standard operating procedure for
cross-border connections related to the import of
drugs and medical devices which has been proven
useful to healthcare workers on both sides.
Medical training of international standard is
also taking shape in Shenzhen. Hundreds of HKU
medical students used to attend clinical attachment
in HKU-SZH until it was disrupted by the pandemic.
To speed up the integration of medical training, in
September 2021, the Shenzhen Health Commission
had approved the development of a pilot specialist
training programme by HKU-SZH through the
Shenzhen–Hong Kong Medical Specialist Training
Centre8 and with the full support of the Hong Kong
Academy of Medicine, the respective specialty
Colleges of Hong Kong, and the Shenzhen Medical
Doctors Association. A new medical school of The
Chinese University of Hong Kong is also under
construction in Shenzhen.9
The cross-border connection and integration are
progressing rapidly in multiple directions and levels.
All the measures discussed here, as well as several
others, are important and effective in accelerating the
pace of cross-border connection and the integration of medical services in Hong Kong, Shenzhen, Macau,
the GBA, and beyond. All signs have shown that
not only the connection and integration of medical
services are working, but they will also be sustained
and sustainable in the long run. The connection and
integration programme has yielded good results and
been proven successful and rewarding.
Challenges and sustainability
There are many challenges in the connection
and integration programme, including language
barriers, varying medical training and backgrounds,
differences in culture and governance, and shortage
of human resources and funding. So far, these have
been confronted and resolved successfully. The large
number of episodes of connection and integration
discussed above suggests that connection and
integration in healthcare have been succeeding,
sustained, and striding on within a rather short
period of time. The COVID-19 pandemic provided
a bitter lesson to the Central Government and its
people that a pandemic can harm and destroy a
government, regime, metropolis, nation, and people.
There is no better defence than good healthcare, and
the most expedient and least expensive way to possess
it is through continuing and sustainable connection
and integration with world class healthcare systems.
Although this is a difficult task, it is achievable,
especially so in GBA with its abundant resources.
Promotion of connection and
integration under the fifth wave of COVID-2019 in Hong Kong
The fifth wave of COVID-19 in Hong Kong
accelerated the pace of forming healthcare
connections and partnerships between Hong
Kong and mainland China. The mainland Chinese
healthcare workers started to arrive in Hong Kong
in the middle of March 2022 when the fifth wave of
COVID-19 began. A total of 391 medical workers,
mainly from Guangdong Province, arrived at the
community treatment facility at AsiaWorld-Expo.10
Within a week, they had learned on the job the Hong
Kong nursing standard operating procedure and
information technology structure and were working
side by side with their HA workmates. Meanwhile,
at Lok Ma Chau, some 20 000 mainland Chinese
workers finished building a massive makeshift
hospital within weeks.11 The mainland Chinese
healthcare workers went and served wherever and
whenever they were needed. Their knowledge, skill,
enthusiasm, good manner, and ethics impressed
the patients, their Hong Kong colleagues, and the
public. As the fifth wave of COVID-19 faded in Hong
Kong and the Chinese healthcare workers were
packing to return home, there were many favourable reports at all levels regarding the support provided
by them and the Central Government.10 The positive
experiences and encounters of medical workers on
both sides during the COVID-19 pandemic have
led to the belief that mutual learning, concern,
assistance, and cooperation, between the two
different medical systems are achievable and will be
helpful in providing quality healthcare in the GBA
and beyond. These experiences undoubtedly serve as
one of the best ways to promote the programme of
connection and integration.
Summary
Both the Central and the Hong Kong SAR
Governments are determined to build a healthy
nation and city. Just as the fifth wave of COVID-19
stabilised, Hong Kong’s Chief Executive–elect Mr
John Lee pledged on 29 April 2022, to develop a
better health service and caring society for Hong
Kong in his policy manifesto.12 Meanwhile the Central and Shenzhen Governments have continued
to engage in building Shenzhen into a model
and modern metropolis in a strong nation under
socialism with Chinese characteristics to be followed
by future Chinese cities. Hong Kong, Shenzhen,
and Macau, the ‘Tri-Cities’, are asked to enhance
their participation in and contribution to the grand
development of the GBA. The GBA is expanding
and flourishing. Using well of the talent, wisdom,
intelligence, experience, and resources of their cities
and their residents, Hong Kong will continue to
show its caring character, and Shenzhen will develop
itself into an ultra-modern metropolis in a strong
nation under socialism with Chinese characteristics.
Author contributions
Concept or design: PMC Pai, JKM Fan, WCW Wong, XP Xu, CM Lo.
Acquisition of data: XF Deng.
Analysis or interpretation of data: PMC Pai, JKM Fan, WCW Wong.
Drafting of the manuscript: PMC Pai.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: XF Deng.
Analysis or interpretation of data: PMC Pai, JKM Fan, WCW Wong.
Drafting of the manuscript: PMC Pai.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
We thank Prof Anne Wing-mui Lee and Dr Joseph Chi-yuen Chan from The University of Hong Kong–Shenzhen Hospital
(HKU-SZH) for their direct contribution to the Hospital
Authority clinic service in HKU-SZH, and Prof Walter Wai-kay Seto from Li Ka Shing Faculty of Medicine of The University of Hong Kong for his advice to the manuscript.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The Medical Ethics Committee of The University of Hong Kong–Shenzhen Hospital has waived the need for ethics
approval and patient consent for this study.
References
1. Chu P, Pai P. A new great wall: commissioning a new hospital in China. Future Hosp J 2015;2:28-33. Crossref
2. Liang W, Wang C, Wu P, editors. Blue Book of Health Reform. Development Report on Health Reform in China
2020. Beijing: Social Science Academic Press; 2020.
3. Ministry of Commerce of The People’s Republic of China. Implementation Plan (2020-2025) Issued by the General
Office of the CPC Central Committee and the General
Office of the State Council for Comprehensive Pilot Reform
in Shenzhen to Build the City into a Pilot Demonstration
Zone for Socialism with Chinese Characteristics [in
Chinese]. Available from: http://www.mofcom.gov.cn/article/resume/n/202010/20201003006969. Accessed 31 Mar 2022.
4. 政府擬託港大深圳醫院為港人診症. News.gov.hk. Available from: https://www.news.gov.hk/chi/2020/09/20200915/20200915_171027_139.html. Accessed 12 Jun 2023.
5. 深圳市人民政府辦公廳.《關於加快推動醫療服務跨
境銜接的若干措施》. Available from: http://www.sz.gov.cn/attachment/0/774/774421/8724838.pdf Accessed 31 Mar 2022.
6. Zhang Y. City bestows senior title to 37 HK medical professionals. Shenzhen Daily. 6 August 2021. Available
from: http://www.szdaily.com/content/2021-08/06/content_24459894.htm. Accessed 31 Mar 2022.
7. 廣東省藥品監督管理局. 省藥品監管局切實推進“港澳藥械通”政策 提升灣區居民幸福感. Available from: http://mpa.gd.gov.cn/xwdt/sjdt/content/post_3500048.html. Accessed 25 May 2022.
8. Hong Kong Academy of Medicine. SZ-HK Medical Specialist Training Centre. Available from: https://www.hkam.org.hk/en/initiative/sz-hk-medical-specialist-training-centre. Accessed 23 May 2022.
9. CUHK-SZ unveils new medical school. Shenzhen Daily. 18 August 2021. Available from: https://www.cnbayarea.org.cn/english/News/content/mpost_538179.html. Accessed 11 May 2022.
10. Li Y. HKSAR Chief Executive sees off mainland medical workers supporting pandemic fight. Chinanews.com. 6 May 2022. Available from: http://www.ecns.cn/news/2022-05-06/detail-ihayamfc5315102.shtml. Accessed 5 Jun 2022.
11. Chan O. First phase of emergency hospital handed over to Hong Kong. Chinadaily.com.cn. 18 April 2022. Available from: http://www.chinadaily.com.cn/a/202204/08/WS624f71bba310fd2b29e55ac6.html Accessed 5 Jun 2022.
12. CE-elect pledges new era of unity. News.gov.hk. Available from: https://www.news.gov.hk/eng/2022/05/20220508/20220508_140909_199.html. Accessed 5 Jun 2022.

