Hong Kong Med J 2023 Jun;29(3):265–7 | Epub 12 May 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Home haemodialysis with a novel machine in a patient with end-stage kidney disease: first case report from Asia
Vickie WK Kwong, MB, BS, FRCP; Christine WY Au, RN, BN; MC Law, BN, MSocSc; KM Chow, MB, ChB; CC Szeto, MB, ChB, MD; Philip KT Li, FHKCP, FHKAM (Medicine)
Department of Medicine and Therapeutics, Carol and Richard Yu Peritoneal Dialysis Research Centre, Prince of Wales Hospital, The Chinese University of Hong Kong, Hong Kong SAR, China
Corresponding author: Prof Philip KT Li (philipli@cuhk.edu.hk)
Case report
The patient is a 38-year-old man who previously
worked as a computer programmer and currently
resides in Hong Kong with his parents and his
younger brother in a flat of around 500 square
feet. At age 22, he was diagnosed with diabetes
mellitus subsequently complicated by diabetic
nephrosclerosis and non–vision-threatening
retinopathy. His comorbidity includes overweight,
hypertension, hypothyroidism, and eczema. He
developed end-stage kidney disease (ESKD) in late
2015 and commenced peritoneal dialysis (PD) that
unfortunately failed after 3 years due to refractory
PD-related peritonitis. Thereafter, he commenced
in-centre haemodialysis (HD) in 2018.
The patient underwent 4 hours of in-centre HD
3 times per week via his left forearm arteriovenous
fistula. He subsequently reported increased lethargy
with poor appetite and was mainly sedentary after
quitting his job. His daily fluid intake fluctuated
widely with interdialytic weight gain up to 4 to 6 kg
necessitating an increase in his antihypertensive
medications. His appetite remained suboptimal,
and his dry body weight gradually decreased from
72 kg (height: 1.72 m, body mass index: 24.3) at the
start of in-centre HD in late 2018 to 67 kg (body
mass index: 22.6) by late 2020. He also experienced
a worsening of uremic pruritus. Cannulation for
dialysis became increasingly difficult due to his
eczema. His standardised Kt/V value averaged 1.4
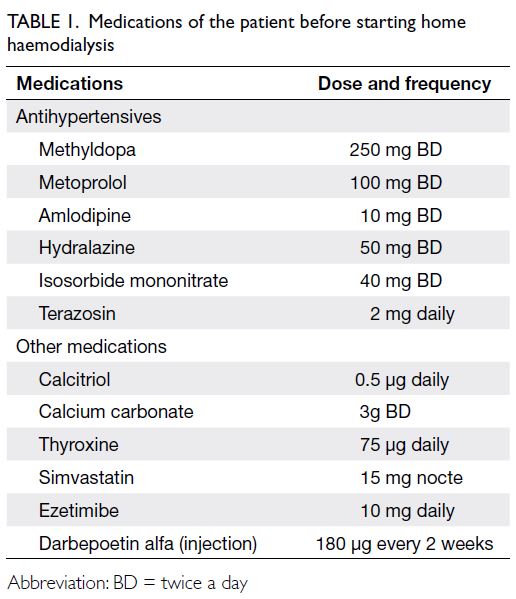
only. His medications are shown in Table 1.
In late 2020, our centre started a home
haemodialysis (HHD) programme using a novel HD
machine (NxStage System One; Fresenius Medical
Care, Tijuana, Mexico). The patient was keen to join
the programme. The dermatology team was consulted
and his eczema improved after treatment. He was
taught to self-cannulate his arteriovenous fistula
by our dialysis nurses and achieved independent
self-cannulation after 10 HD sessions in 3 weeks.
A home visit by engineers indicated a need for
only minimal home modifications. Haemodialysis could be performed in a room of around 25 square
feet, with water source from the washroom basin
pipes and drainage to the original ground drain via
connecting hoses. He received a further 2 weeks
of machine training with the novel HD machine
and commenced HD at home in early 2021. He has
since adopted a HHD schedule of 3.5 to 4 hours of
dialysis per session, 4 times per week since March
2021. We continue to provide 24-hour support for
him via telephone and a communication phone
application. To date, he has continued treatment
with no significant problems reported.
After the commencement of HHD, his need
for antihypertensive agents and erythropoiesis-stimulating
agent gradually reduced and all were
stopped after approximately 3 months. The patient’s
appetite greatly improved and his dry weight gradually increased to 72 kg. Nonetheless this was
accompanied by frequent pre-HD hyperkalaemia
and hyperphosphataemia, hence he was referred for
appropriate dietary advice. He achieved an average
standardised Kt/V value of 2 to 2.1. A comparison
of parameters while he was receiving in-centre HD
and 6 months after he commenced HHD is shown in
Table 2. It is of note that his hyperphosphataemia is
of a lower magnitude after commencing HHD when
compared with the level while he was on in-centre
HD. He experienced increased energy, started going
out more frequently, and resumed exercise that
included regular walking and playing badminton.
In January 2022, he resumed working as a computer
programmer.
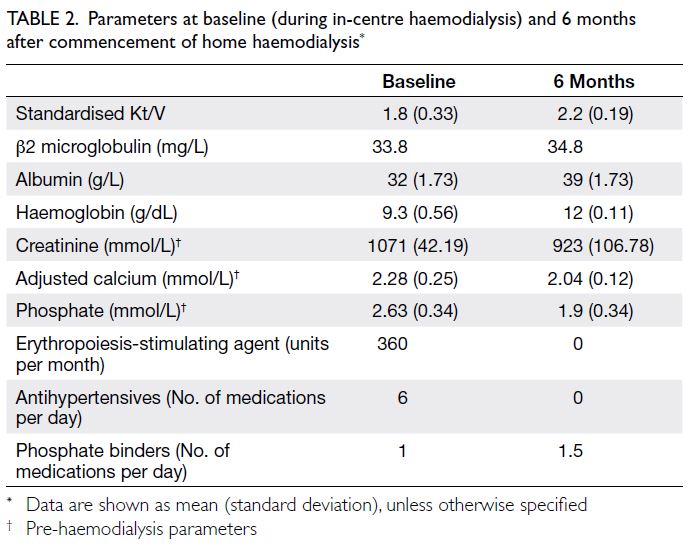
Table 2. Mean parameters at baseline (during in-centre haemodialysis) and 6 months after commencement of home haemodialysis
Discussion
When PD fails in patients with ESKD, it is necessary to commence HD, mostly at a conventional in-centre
HD unit. A selected number of suitable patients are
recruited into the HHD programme.
Conventional in-centre HD has several
limitations including a shorter treatment time
(about 8-12 hours per week) that may not provide
adequate clearance, an inflexible schedule, and
additional financial costs associated with travel, all
of which could have a negative impact on patients’
employment and social life. In contrast, frequent
HHD with longer treatment time may have more
benefits such as better fluid and solute removal with
consequent improvement in blood pressure control,
left ventricular mass index, sleep apnoea, anaemia,
quality of life, pregnancy success rates, as well as
reduced mortality.1 Nocturnal home haemodialysis (NHHD) service has been provided in Hong Kong since 2006, with a typical regimen of alternate nightly HD for around 8 hours, and benefited numerous
patients over the years. Indeed, Hong Kong has
been promoting the use of home therapy including
HHD and PD in ESKD patients to the global renal
community.2
Nonetheless most Hong Kong citizens live in
relatively small flats and may have insufficient space
for the installation of both the conventional HD
machine and the reverse osmosis machine plus other
requisite consumables. Those who live in rented
accommodation that precludes an ability to make
necessary home modifications to meet the specific
electricity and water pressure standards required
during NHHD treatments may not be suitable for
the NHHD programme. The mandatory requirement
for NHHD candidates to have a helper who can
safeguard them during treatments also excludes
those living alone from joining this programme.
Furthermore, the relatively longer training time (up
to 3 months or more) associated with the use of the
more ‘complicated’ conventional machines may pose
learning difficulties for many patients.
To expand the HHD service in Hong Kong,
a pilot HHD programme using the novel NxStage
System One HD machine was introduced in 2019
at the Prince of Wales Hospital. Studies have shown
benefits related to frequent HHD using the new
system.3 It uses a low–dialysate volume approach
aiming to maximise the urea saturation in the
dialysate by reducing the dialysate flow rate to a rate
slower than the blood flow rate, resulting in very
efficient use of the dialysate. Typically, a total of 30
to 60 litres of dialysate is used for a single session
with the new system, whereas 120 to 140 litres of
dialysate is typically required for the conventional
HD machines. Dialysate is generated and stored
before starting treatment, therefore the risk of water
leakage during treatment is reduced, compared
with the ongoing dialysate generation during
conventional NHHD. Its simple design and much
smaller footprint, on top of the advantage of no
requirement for major home plumbing or electrical
system modifications, facilitates a shorter machine
training time of around 2 weeks.4
Initially the patient’s family had reservations
about him performing HD at home alone but
were reassured after detailed discussion and
understanding the simplicity of machine operation.
The patient’s eczema, especially around his
arteriovenous fistula site, occasionally gives cause for
concern but effective dermatological treatment and
the use of the ‘rope ladder’ instead of the ‘buttonhole’
method for cannulation minimises his infection risk.
His appetite was much increased after starting HHD
and there was concern about his glucose and fluid
control as well as rising potassium and phosphate levels. Counselling by our dietitian has improved the situation.
Dialysis adequacy of HD schedules more
frequent than thrice weekly is measured by the
standardised Kt/V and the current clinical practice
guidelines suggest a minimum value of 2.0.
Nonetheless studies have shown that standardised
Kt/V may not correlate well with clinical outcomes.
A more comprehensive evaluation should
include other parameters such as self-reported
health status and physical measurements of
cardiovascular health (such as blood pressure and
echocardiogram). Traditional biochemical outcomes
and measurements of solute clearance may also be
considered.5 Our patient improved clinically as well as socially after commencing HHD with the new
system. We believe that this treatment modality has
the potential to benefit many more patients with
ESKD.
Author contributions
Concept or design: All authors.
Acquisition of data: VWK Kwong, CWY Au.
Analysis or interpretation of data: VWK Kwong, CWY Au, MC Law, PKT Li.
Drafting of the manuscript: VWK Kwong, PKT Li.
Critical revision of the manuscript for important intellectual content: VWK Kwong, CWY Au, MC Law, PKT Li.
Acquisition of data: VWK Kwong, CWY Au.
Analysis or interpretation of data: VWK Kwong, CWY Au, MC Law, PKT Li.
Drafting of the manuscript: VWK Kwong, PKT Li.
Critical revision of the manuscript for important intellectual content: VWK Kwong, CWY Au, MC Law, PKT Li.
Conflicts of interest
The authors have no conflicts of interest to disclose.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki, provided informed consent for the treatment/procedures, and provided consent for publication.
References
1. Diaz-Buxo JA, White SA, Himmele R. Frequent hemodialysis: a critical review. Semin Dial 2013;26:578-89. Crossref
2. Li PK, Cheung WL, Lui SL, et al. Increasing home based dialysis therapies to tackle dialysis burden around the world: a position statement on dialysis economics from the
2nd Congress of the International Society for Hemodialysis.
Nephrology (Carlton) 2011;16:53-6. Crossref
3. Borman N, Ficheux M, Slon MF, et al. SP597 favourable
biochemical outcomes of frequent hemodialysis at
home using the NxStage® System One™—The European
experience. Nephrol Dial Transplant 2016;31(supp_1):i294. Crossref
4. Clark WR, Turk JE Jr. The NxStage System One. Semin Dial 2004;17:167-70. Crossref
5. Rivara MB, Ravel V, Streja E, et al. Weekly standard Kt/Vurea and clinical outcomes in home and in-center
hemodialysis. Clin J Am Soc Nephrol 2018;13:445-55. Crossref