Hong Kong Med J 2023 Jun;29(3):233–9 | Epub 25 May 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Five-year retrospective review of ultrasound-guided
manual vacuum aspiration for first-trimester miscarriage
Olivia SY Chau, MB, ChB, MRCOG1; Tracy SM Law, FHKCOG, FHKAM (Obstetrics and Gynaecology)1; Karen Ng, FHKCOG, FHKAM (Obstetrics and Gynaecology)1; TC Li, PhD (Sheffield), FRCOG2; Jacqueline PW Chung, FHKCOG, FHKAM (Obstetrics and Gynaecology)2
1 Department of Obstetrics and Gynaecology, Prince of Wales Hospital, Hong Kong SAR, China
2 Department of Obstetrics and Gynaecology, The Chinese University of Hong Kong, Hong Kong SAR, China
Corresponding author: Dr Jacqueline PW Chung (jacquelinechung@cuhk.edu.hk)
Abstract
Introduction: Manual vacuum aspiration is
increasingly accepted as an alternative to medical or
surgical evacuation of the uterus after first-trimester
miscarriage. This study aimed to assess the efficacy
of ultrasound-guided manual vacuum aspiration
(USG-MVA) in the management of first-trimester
miscarriage.
Methods: This retrospective analysis included adult women with first-trimester miscarriage who
underwent USG-MVA in Hong Kong between July
2015 and February 2021. The primary outcome
was the efficacy of USG-MVA in terms of complete
evacuation of the uterus, without the need for
further medical or surgical intervention. Secondary
outcomes included tolerance of the entire procedure,
the success rate of karyotyping using chorionic villi,
and procedural safety (ie, any clinically significant
complications).
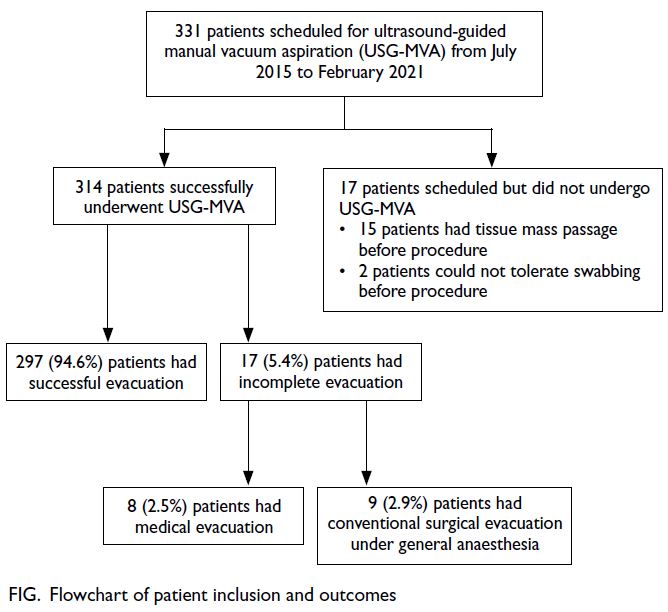
Results: In total, 331 patients were scheduled to
undergo USG-MVA for first-trimester miscarriage
or incomplete miscarriage. The procedure was
completed in 314 patients and well-tolerated in all
of those patients. The complete evacuation rate was
94.6% (297/314), which is similar to the rate (98.1%)
achieved by conventional surgical evacuation in a
previous randomised controlled trial in our unit. There were no major complications. Samples from
95.2% of patients were suitable for karyotyping,
which is considerably higher than the rate of suitable
samples (82.9%) obtained via conventional surgical
evacuation in our previous randomised controlled
trial.
Conclusion: Ultrasound-guided manual vacuum
aspiration is a safe and effective method to manage
first-trimester miscarriage. Although it currently
is not extensively used in Hong Kong, its broader
clinical application could avoid general anaesthesia
and shorten hospital stay.
New knowledge added by this study
- Ultrasound-guided manual vacuum aspiration (USG-MVA) is a safe and effective method for the management of miscarriage, but its use is limited in Hong Kong.
- USG-MVA is similar in safety and efficacy to conventional surgical evacuation of the uterus (dilatation and curettage) under general anaesthesia for the management of miscarriage; it is well-tolerated by patients and causes minimal complications.
- USG-MVA is a good surgical option for women with miscarriage who wish to obtain products of conception for karyotyping.
- USG-MVA can be more widely implemented as an alternative to conventional dilatation and curettage/electrical vacuum aspiration of the uterus for the management of first-trimester miscarriage in Hong Kong.
- For women with recurrent miscarriage, USG-MVA should be considered because it has a higher rate of karyotyping success, compared with conventional suction evacuation of the uterus.
Introduction
Miscarriage occurs in 10% to 20% of pregnancies, and approximately one in four women will experience a
miscarriage in their lifetime.1 It is managed using one
of three approaches: expectant, medical, or surgical.
In 1972, manual vacuum aspiration (MVA) was introduced2 as an alternative method for the surgical
management of miscarriage. It is performed using
a handheld 60-mL syringe, which creates a suction
force to aspirate the contents of the uterus through
a cannula. This technique has various applications,
including the management of first-trimester miscarriage, incomplete or missed miscarriage,
endometrial biopsy, and first-trimester termination
of pregnancy; it can also be used after failed medical
evacuation of pregnancy. Because it only requires
simple oral analgesics or conscious sedation, this
procedure can be performed on an out-patient basis
in a treatment (or procedure) room; thus, it avoids
the use of a surgical theatre and the risks of general
anaesthesia, resulting in a shorter hospital stay.3
Conventional MVA is performed without
ultrasound guidance. However, because MVA is
performed on an out-patient basis without general
anaesthesia, ultrasound guidance may help to
minimise discomfort and procedure duration by
limiting the number of suction catheter passes and
achieving a higher rate of complete evacuation.
Studies by Elsedeek4 and Ali et al5 have shown that
ultrasound guidance allows clinicians to avoid
contact with the uterine fundus, leading to higher
rates of procedure completion, significantly lower
pain scores, and shorter procedure times. We
previously demonstrated that ultrasound-guided
manual vacuum aspiration (USG-MVA) is a feasible
and effective alternative surgical approach for first-trimester
miscarriage.6
Additionally, women with recurrent
miscarriage may prefer surgical evacuation (rather
than medical evacuation) because this approach
facilitates the acquisition of products of conception for cytogenetic analysis. The use of USG-MVA
causes less disruption of products of conception;
it also can aid in the identification of chorionic
villi for karyotyping. Therefore, USG-MVA may
be particularly useful for women with recurrent
miscarriage.
Ultrasound-guided manual vacuum aspiration
is gaining acceptability, awareness, and recognition
in Hong Kong, although it is not commonly used
in clinical practice. To demonstrate the value
of the procedure, this study aimed to assess the
effectiveness of USG-MVA in the management of
first-trimester miscarriage.
Methods
Patient selection
This retrospective observational study included all women who underwent USG-MVA in Hong Kong
during the period from July 2015 to February 2021.
Eligible patients were identified by hospital records
in Prince of Wales Hospital and Union Hospital.
The indications for USG-MVA included missed or
incomplete miscarriage at <12 weeks of gestation,
as well as the desire for cytogenetic examination
of the products of conception to determine the
underlying cause of miscarriage. For naturally
conceived pregnancies, the date of the last menstrual
period was used to determine gestational age. For
artificially conceived pregnancies, gestational age
was determined according to the date of ovulation,
oocyte retrieval, or embryo transfer. All women
were counselled about the management options:
expectant, medical, conventional surgical (electrical
vacuum aspiration with or without dilatation and
curettage, under general anaesthesia), and USG-MVA.
Miscarriage was diagnosed by ultrasound
examination. A diagnosis of missed miscarriage
was made if a discrete embryo ≥7 mm without fetal
heart pulsation, or an intrauterine gestational sac
with a mean sac diameter of 25 mm excluding the
fetal pole, was detected on transvaginal ultrasound.
If only transabdominal ultrasound was performed,
the crown-rump length was recorded; a second scan
was performed 14 days later. A diagnosis of missed
miscarriage also was made if the mean sac diameter
was ≤25 mm without evidence of growth, or if there
was a sustained absence of fetal heart pulsation,
during a follow-up examination 7 to 14 days later.7 8
A diagnosis of incomplete miscarriage was
made if the ultrasound examination showed residual
products of conception after the initial passage,
defined as consistent intra-uterine thickness of
≥11 cm in the sagittal and transverse planes, and/or
if the patient experienced persistent symptoms such
as pain or bleeding.9
Patients were excluded if they had a known history of uterine anomalies, cervical stenosis, and/or multiple fibroids with uterine distortion. Patients
were also excluded if they had suspected infection,
an abnormal coagulation profile, haemodynamic
instability, and/or extreme anxiety that hindered
their ability to tolerate a pelvic examination.
Outcome measures
The primary outcome measure was the efficacy
of USG-MVA in terms of complete evacuation of
the uterus, without the need for further medical
or surgical intervention. We also compared the
complete evacuation rate with optimal outcomes in
our unit from a previous randomised controlled trial
(RCT) that involved other methods of miscarriage
management.10 Secondary outcomes included
whether patients could tolerate the entire procedure
without discontinuation prior to completion; the
success rate of karyotyping using chorionic villi
obtained from USG-MVA–collected samples,
compared with samples collected by conventional
surgical evacuation in our unit during the same
period; and procedural safety, defined as the
occurrence of any clinically significant complications
(eg, bleeding requiring blood transfusion, uterine
perforation, infection, and vasovagal shock).
Ultrasound-guided manual vacuum
aspiration procedure
Ultrasound-guided manual vacuum aspiration was
performed on an out-patient basis in a treatment
room with a handheld syringe and flexible curette,
as well as an ultrasound machine. Each patient was
instructed to take misoprostol 400 μg orally 2 to
3 hours before the procedure for cervical priming;
they were also instructed to take naproxen 500 mg
1 hour before the procedure for pre-emptive pain
relief. Patients were instructed to take paracetamol
or codeine, rather than naproxen, if they were allergic
to non-steroidal anti-inflammatory drugs. Upon
admission, patients were asked not to void because
a full bladder enables better visualisation of the
uterus on transabdominal ultrasound. Prophylactic
antibiotics were not routinely administered prior to
the procedure.
Ultrasound-guided manual vacuum aspiration
was performed by an experienced clinician using a
60-mL handheld syringe with a self-locking plunge
(MedGyn Aspiration Kit; MedGyn Products,
Addison [IL], US) attached to a flexible curette (size
4-7 mm, according to clinician preference); a nurse
assisted with ultrasound guidance. During USG-MVA,
a speculum examination and swabbing were
performed with aseptic technique. A paracervical
block with 2% lidocaine was administered using a
Terumo Dental Needle (Terumo, Tokyo, Japan). If
necessary, the clinician performing the procedure
could immobilise the cervix using a tenaculum. Local topical anaesthetic gel (xylocaine 2%) was applied
to the cervix and suction catheter. To guide curette
insertion into the uterine cavity, transabdominal
ultrasound was performed using a Voluson
E730 Expert USG system (GE Medical Systems,
Kretztechnik, Zipf, Austria). Suction was applied
with the handheld syringe to remove products of
conception, which were then immersed in normal
saline along with detached chorionic villi.
The USG-MVA procedure was completed
when the ultrasound examination showed a thin
endometrial lining, confirming that the uterine
cavity was empty. Products of conception were
sent to the laboratory for histological examination
and cytogenetic analysis, in accordance with each
patient’s preferences. All Rhesus-negative women
were administered anti-D prophylaxis.
Patients were discharged 2 to 3 hours after
the procedure if they were clinically healthy and
haemodynamically stable. A postoperative telephone
hotline was established; patients were advised to
contact the ward at any time if they encountered
excessive bleeding, abdominal pain, or fever. A
follow-up appointment was scheduled 2 to 3 weeks
after the procedure to ensure complete evacuation
had been achieved.
Statistical analysis
Analyses were performed using SPSS (Windows
version 23.0; IBM Corp, Armonk [NY], United States).
Data were expressed as counts and percentages.
Comparisons were conducted using the Chi squared
test for categorical variables and Student’s t test for
continuous variables. Two-tailed P values <0.05 were
considered statistically significant.
Results
In total, 331 patients were scheduled to undergo
USG-MVA during the study period. Seventeen of
these 331 patients did not undergo USG-MVA: 15
patients experienced passage of a tissue mass before
the procedure, and two patients could not tolerate
swabbing before the procedure. Thus, 314 patients
successfully underwent USG-MVA (Fig).
The baseline characteristics of the 314 included
patients are summarised in Table 1. All patients
received oral misoprostol for cervical priming;
all patients were able to tolerate and complete the
procedure. There were no major complications
such as uterine perforation or significant bleeding
(ie, requiring blood transfusion or uterotonics). All
patients were discharged within 3 hours after the
procedure. The complete evacuation rate was 94.6%
(297/314) [Table 2] and there were no unscheduled
readmissions.
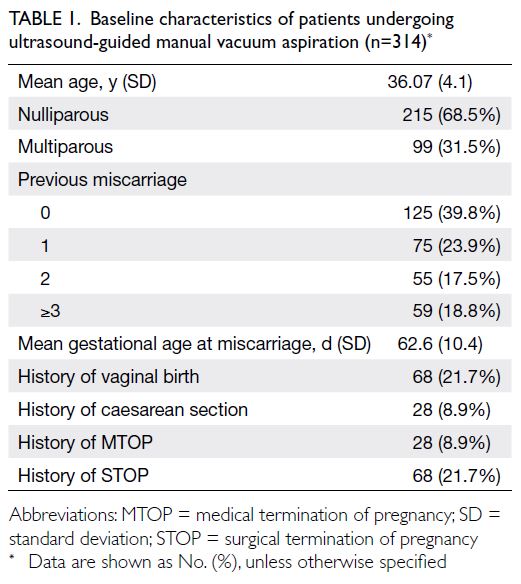
Table 1. Baseline characteristics of patients undergoing ultrasound-guided manual vacuum aspiration (n=314)
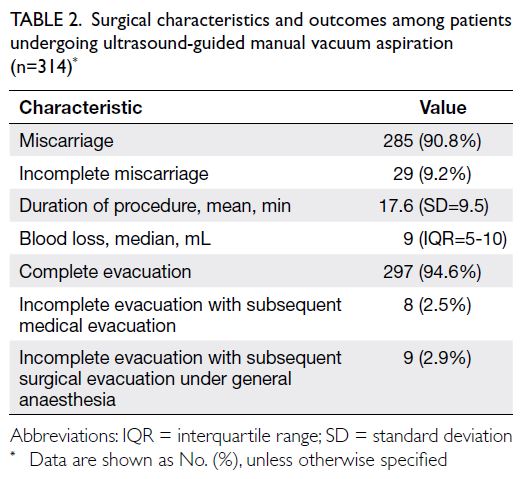
Table 2. Surgical characteristics and outcomes among patients undergoing ultrasound-guided manual vacuum aspiration (n=314)
With respect to the results of other miscarriage
management methods analysed in our previous
RCT,10 we found that USG-MVA had a significantly higher complete evacuation rate compared with
medical evacuation (94.6% vs 70%; P<0.001) or
expectant management (94.6% vs 79.3%; P<0.001).
Ultrasound-guided manual vacuum aspiration also
had a complete evacuation rate that was comparable
with the rate achieved by conventional surgical evacuation (94.6% vs 98.1%10; P=0.024). Furthermore,
the rate of complete evacuation did not significantly
differ between women with missed miscarriage and
women with incomplete miscarriage (P=0.621).
Of the 17 patients (5.4%) who had incomplete
evacuation during USG-MVA, eight (2.5%)
subsequently underwent medical evacuation,
whereas nine (2.9%) selected conventional surgical
evacuation under general anaesthesia (Table 2).
In terms of histological examination, 66.2% of
patients (208/314) requested karyotyping. Among
samples from those patients, 95.2% (198/208) were
suitable for karyotyping; the culture failure rate
was 4.8% (10/208). During the same period, 82.9%
(295/356) of samples obtained via conventional
surgical evacuation10 were suitable for karyotyping,
which is significantly lower than the 95.2% of samples
obtained via USG-MVA (P<0.001).
Among the samples that were suitable for
karyotyping, 65.7% (130/198) had an abnormal
karyotype and 34.3% (68/198) had a normal
karyotype. Of the 10 samples that were unsuitable
for karyotyping, eight contained no chorionic villi,
whereas two had a limited number of villi; these
characteristics contributed to culture failure.
Discussion
Since our unit introduced MVA as an alternative to conventional surgical evacuation of the uterus for
first-trimester miscarriage, it has generally been
well-received by eligible patients.11 Manual vacuum
aspiration constitutes a safe and effective uterine
evacuation procedure; it is widely used in other
countries, including the United States and United
Kingdom.11 12 13 14 Thus far, MVA is not commonly used
in Hong Kong, possibly because there is a lack
of familiarity with the procedure. This study was
conducted to explore the utilisation and outcomes of
USG-MVA, particularly with respect to the complete evacuation rate, safety, tolerability, and successful
acquisition of chorionic villi for karyotyping.
In this study, the complete evacuation rate of
USG-MVA was 94.6%, which is within the range
of 89% to 98% reported in previous studies.12 15 The
complication rate was low, tolerability was good,
and the proportion of samples that were suitable for
karyotyping was high.
The complete evacuation rate achieved using
conventional dilatation and curettage reportedly
ranges from 88% to 98%,16 17 which is consistent
with previous data from our unit (98.1%).10 These
rates are comparable with the rate achieved using
USG-MVA in the present study. Moreover, complete
evacuation rates achieved via medical management
were 84% in an RCT by Zhang et al18 and 70% in our
unit10; complete evacuation rates after expectant
management reportedly ranged from 16% to 76%,19 20
similar to the rate of 79.3% observed in our unit.10
Overall, the complete evacuation rate achieved via
medical or expectant management is substantially
lower than the rate achieved using USG-MVA.
Clinical implications
The rate of complications associated with
conventional dilatation and curettage is reportedly
similar21 to the rate of complications associated
with MVA; neither approach has been linked to
major complications. These low complication rates
may be related to the use of ultrasound guidance,
which lowers the risk of uterine perforation or false
tract creation. There is evidence that ultrasound
guidance for dilatation and curettage reduces the
complication rate.22 23 In an RCT that investigated
the use of ultrasound guidance during surgical
termination of pregnancy, Acharya et al24 found
significant reductions in infection rates, retained
products of conception requiring repeat evacuation,
and volume and duration of bleeding in patients who
underwent the procedure with ultrasound guidance.
Therefore, it is reasonable to expect that USG-MVA
also has a lower complication rate, compared with
conventional MVA lacking ultrasound guidance.
However, ultrasound guidance requires additional
equipment and staff with appropriate ultrasound
probe training. Further research is needed to clearly
determine whether the use of ultrasound during
MVA provides a clinical benefit.
Because USG-MVA is an out-patient procedure
performed with local anaesthesia in a procedure
room, it does not require a surgical theatre or
surgical staff. These modified requirements could
reduce costs and allow the surgical theatre to be used
for other procedures. Patients also would also not
be required to fast for a prolonged period prior to
general anaesthesia, which would reduce discomfort
related to the miscarriage experience. Since a general
anaesthesia is not required, it would facilitate a shorter hospital stay, allowing patients to return
more rapidly to the comfort of their home after the
procedure. Other benefits include the potential for
reduced clinical costs and the availability of beds for
other patients who require hospitalisation.
This study also demonstrated that a large
proportion of samples obtained by USG-MVA
are suitable for karyotyping, which is particularly
important for women with recurrent miscarriage.
The culture failure rates with products of conception
obtained via conventional suction evacuation
reportedly range from 10% to 40%25; these rates
are higher than the culture failure rate using
samples obtained by USG-MVA in the present
study. Karyotyping requires relatively intact and
fresh samples, which are often difficult to obtain
by medical evacuation. The products of conception
may be passed hours before a sample is sent to the
laboratory; they may also be accidentally discarded
by the patient.26 During conventional suction
evacuation, the products of conception may be
extensively damaged by the curette, leading to a
higher rate of culture failure.
Strengths and limitations
To our knowledge, this is the first large study in Hong Kong to assess USG-MVA over an extended
period. It provides a clear picture of the utilisation
of USG-MVA in Hong Kong, with important
information regarding the complete evacuation rate,
safety, and tolerability of the procedure.
A notable limitation in this study was its
retrospective design. Although MVA is generally
well-tolerated by patients, as demonstrated in
previous studies,3 11 12 15 it causes greater discomfort
than conventional dilatation and curettage under
general anaesthesia.11 In the present study, tolerability
was determined by review of patient medical
records; it was solely based on whether a patient had
been able to tolerate the entire procedure, and no
measurement of pain was conducted. The use of a
visual analogue scale score during the procedure may
provide a better indication of the actual tolerability
of the procedure. A previous trial of USG-MVA,
conducted by our unit to investigate the efficacy
of hyoscine butylbromide in reducing uterine
contraction pain during the procedure, showed
a slight reduction in pain score compared with
placebo.6 Additional methods could be investigated
to improve pain control during USG-MVA.
Furthermore, some patients may have
experienced pain because misoprostol was
administered for cervical priming prior to the
procedure; this was intended to facilitate insertion
of the suction catheter. The MedGyn Aspiration
Kit provides suction catheters in sizes 4 to 7; if
necessary, dilatation could thus be performed under
ultrasound guidance using the suction catheters, thereby eliminating the need for misoprostol before
the procedure and reducing the amount of pain
involved in USG-MVA.
The clinicians who performed USG-MVA in
this study ranged from supervised junior trainees to
attending physicians with many years of experience.
Although the procedures were performed by
experienced clinicians who had completed at least
30 MVA procedures before independent practice,
or by trainees who were directly supervised by
an experienced clinician, differences in clinician
experience have the potential to influence the rate
of complete evacuation and the amount of pain
involved. A standardised approach involving a few
dedicated clinicians may reduce this variation.
In this study, data were available concerning
the complete evacuation rate achieved by dilatation
and curettage in our unit and also from the Union
Hospital; however, no data were available from
Union Hospital, where USG-MVA is also performed.
Additionally, the present study was not designed to
allow a comprehensive comparison of miscarriage
management methods. In the future, a well-designed
RCT should be conducted to compare outcomes
among USG-MVA, surgical evacuation, and medical
evacuation.
Importantly, no long-term follow-up was
performed in this study; thus, we could not examine
the long-term effects of USG-MVA.
Future research
Ultrasound-guided manual vacuum aspiration is
regarded as a safe, simple, efficient, and cost-effective
procedure. It allows patients to maintain greater
autonomy, avoids the risks of general anaesthesia,
and has a higher success rate in terms of collecting the
products of conception for karyotyping. However,
USG-MVA remains an invasive procedure, and some
patients may not be able to endure the physical or
(possible) emotional pain involved.27 The addition of
ultrasound guidance to MVA may reduce the number
of suctions required for complete evacuation and
help clinicians avoid contacting the uterine fundus,
thereby minimising the duration and severity of pain
during the procedure. Further research is needed
regarding approaches to minimise the physical and
emotional pain that patients may experience during
the procedure, such as the use of other pain-relieving
agents to minimise discomfort during the procedure.
Research is also needed to identify other potential
advantages of USG-MVA with respect to other
methods of miscarriage management. Moreover,
prospective studies comparing pain scores with
visual analogue scale scores and patient satisfaction
are needed to determine whether the addition of
ultrasound guidance to MVA has a meaningful effect
on pain outcomes.
Because USG-MVA is an out-patient
procedure that does not require a surgical theatre,
an anaesthetist, and an overnight stay, it may be
significantly less expensive than conventional
surgical evacuation of the uterus. The cost of
a USG-MVA procedure includes the MedGyn
Aspiration Kit, which costs approximately US$18. A
cost-effectiveness study is needed to fully explore the
potential for reduced clinical costs.
Future research should also focus on the
potential effects of USG-MVA on fertility. Asherman’s
syndrome, caused by trauma to the basal layer of the
uterus, is most commonly associated with dilatation
and curettage28; it is detected in approximately
20% of patients after dilatation and curettage.29
We hypothesise that the use of USG-MVA without
curettage may reduce endometrial trauma and the
number of intrauterine adhesions, thereby lowering
effects on future fertility. Currently, our unit is
investigating this hypothesis via second-look out-patient
hysteroscopy.
Conclusion
Ultrasound-guided manual vacuum aspiration
is a safe and effective alternative to medical and
conventional suction evacuation, with minimal
complications (eg, uterine perforation, bleeding, and
retained products of conception). Patients can avoid
the risks of general anaesthesia and have a shorter
hospital stay. Ultrasound-guided manual vacuum
aspiration may be appropriate for patients with first-trimester
miscarriage, particularly women who have
experienced recurrent miscarriage and express a
desire for karyotyping.
Author contributions
Concept or design: OSY Chau, TC Li, JPW Chung.
Acquisition of data: OSY Chau, TC Li, JPW Chung.
Analysis or interpretation of data: OSY Chau, JPW Chung.
Drafting of the manuscript: OSY Chau, JPW Chung.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: OSY Chau, TC Li, JPW Chung.
Analysis or interpretation of data: OSY Chau, JPW Chung.
Drafting of the manuscript: OSY Chau, JPW Chung.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, JPW Chung was not involved in the peer review process. Other authors have disclosed no
conflicts of interest.
Acknowledgement
We thank all women who participated in this trial. We also express gratitude to Ms Margaret Hiu-tan Lee, Dr Ying Li,
Ms Cheryl Lee, and Ms Yi-tso Kwan from the Department of
Obstetrics and Gynaecology, The Chinese University of Hong
Kong for assistance in this study.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was performed in accordance with the Declaration of Helsinki. The human study protocol was approved by the
Joint Chinese University of Hong Kong—New Territories East
Cluster Clinical Research Ethics Committee (Ref No.: CREC-2021-206) and the Union Hospital Ethics Committee (Ref No.:
EC025), Hong Kong. All adult participants provided written
informed consent for inclusion in this study. The STROBE
(Strengthening the Reporting of Observational Studies in
Epidemiology) guidelines were followed when reporting this
study.
References
1. Webster K, Eadon H, Fishburn S, Kumar G; Guideline Committee. Ectopic pregnancy and miscarriage: diagnosis
and initial management: summary of updated NICE
guidance. BMJ 2019;367:l6283. Crossref
2. Karman H, Potts M. Very early abortion using syringe as vacuum source. Lancet 1972;1:1051-2. Crossref
3. Sharma M. Manual vacuum aspiration: an outpatient alternative for surgical management of miscarriage. Obstet
Gynaecol 2015;17:157-61. Crossref
4. Elsedeek MS. Comparison between the traditional non-guided and a novel ultrasound-guided technique for office
fitting of intrauterine contraceptive devices. Int J Gynecol
Obstet 2016;133:338-41. Crossref
5. Ali MK, Ramadan AK, Abu-Elhassan AM, Sobh AM. Ultrasound-guided versus uterine sound-sparing approach
during copper intrauterine device insertion: a randomised
clinical trial. Eur J Contracept Reprod Health Care
2022;27:3-8. Crossref
6. Chung JP, Law TS, Mak JS, Liu RC, Sahota DS, Li TC. Hyoscine butylbromide in pain reduction associated
with ultrasound-guided manual vacuum aspiration: a
randomized placebo-controlled trial. Reprod Biomed
Online 2022;44:295-303. Crossref
7. Doubilet PM, Benson CB, Bourne T, et al. Diagnostic criteria for nonviable pregnancy early in the first trimester. N Engl J Med 2013;369:1443-51. Crossref
8. Wie JH, Choe S, Kim SJ, Shin JC, Kwon JY, Park IY. Sonographic parameters for prediction of miscarriage: role
of 3-dimensional volume measurement. J Ultrasound Med
2015;34:1777-84. Crossref
9. Bar-Hava I, Aschkenazi S, Orvieto R, et al. Spectrum of normal intrauterine cavity sonographic findings after first-trimester abortion. J Ultrasound Med 2001;20:1277-81. Crossref
10. Kong GW, Lok IH, Yiu AK, Hui AS, Lai BP, Chung TK. Clinical and psychological impact after surgical, medical
or expectant management of first-trimester miscarriage—a
randomised controlled trial. Aust N Z J Obstet Gynaecol
2013;53:170-7. Crossref
11. Chung JP, Chung CH, Mak JS, Li TC, Kong GW. Efficacy, feasibility and patient acceptability of ultrasound-guided manual vacuum aspiration for treating early pregnancy
loss. Aust N Z J Obstet Gynaecol 2019;59:71-6. Crossref
12. Milingos DS, Mathur M, Smith NC, Ashok PW. Manual vacuum aspiration: a safe alternative for the surgical management of early pregnancy loss. BJOG 2009;116:1268-71.Crossref
13. Macisaac L, Darney P. Early surgical abortion: an alternative to and backup for medical abortion. Am J Obstet Gynecol 2000;183 (2 Suppl):S76-83. Crossref
14. Morrison J. The care of women requesting induced abortion. Guideline No. 7. J Obstet Gynaecol 2003;23:521-4. Crossref
15. Tasnim N, Mahmud G, Fatima S, Sultana M. Manual
vacuum aspiration: a safe and cost-effective substitute of
electric vacuum aspiration for the surgical management of
early pregnancy loss. J Pak Med Assoc 2011;61:149-53.
16. Sajan R, Pulikkathodi M, Vahab A, Kunjitty VM, Imrana
HS. Expectant versus surgical management of early
pregnancy miscarriages—a prospective study. J Clin Diagn
Res 2015;9:QC06-9. Crossref
17. Wen J, Cai QY, Deng F, Li YP. Manual versus electric
vacuum aspiration for first-trimester abortion: a systematic
review. BJOG 2008;115:5-13. Crossref
18. Zhang J, Gilles JM, Barnhart K, et al. A comparison of
medical management with misoprostol and surgical
management for early pregnancy failure. N Engl J Med
2005;353:761-9. Crossref
19. Shelley JM, Healy D, Grover S. A randomised trial of surgical, medical and expectant management of first
trimester spontaneous miscarriage. Aust N Z J Obstet
Gynaecol 2005;45:122-7. Crossref
20. Jurkovic D, Ross JA, Nicolaides KH. Expectant management of missed miscarriage. Br J Obstet Gynaecol 1998;105:670-1.Crossref
21. Goldberg AB, Dean G, Kang MS, Youssof S, Darney PD.
Manual versus electric vacuum aspiration for early first-trimester
abortion: a controlled study of complication
rates. Obstet Gynecol 2004;103:101-7. Crossref
22. Hornstein MD, Osathanondh R, Birnholz JC, et al. Ultrasound guidance for selected dilatation and evacuation procedures. J Reprod Med 1986;31:947-50.
23. Chaikof M, Lazer T, Gat I, et al. Lower complication rates with office-based D&C under ultrasound guidance for missed abortion. Minerva Ginecol 2017;69:23-8. Crossref
24. Acharya G, Morgan H, Paramanantham L, Fernando R. A randomized controlled trial comparing surgical
termination of pregnancy with and without continuous
ultrasound guidance. Eur J Obstet Gynecol Reprod Biol
2004;114:69-74. Crossref
25. Shah MS, Cinnioglu C, Maisenbacher M, Comstock I,
Kort J, Lathi RB. Comparison of cytogenetics and molecular
karyotyping for chromosome testing of miscarriage
specimens. Fertil Steril 2017;107:1028-33. Crossref
26. Soler A, Morales C, Mademont-Soler I, et al. Overview of
chromosome abnormalities in first trimester miscarriages:
a series of 1,011 consecutive chorionic villi sample
karyotypes. Cytogenet Genome Res 2017;152:81-9. Crossref
27. Yu FN, Leung KY. Diagnosis and prediction of miscarriage:
can we do better? Hong Kong Med J 2020;26:90-2. Crossref
28. Asherman JG. Traumatic intra-uterine adhesions. J Obstet Gynaecol Br Emp 1950;57:892-6. Crossref
29. Hooker AB, Lemmers M, Thurkow AL, et al. Systematic review and meta-analysis of intrauterine adhesions after
miscarriage: prevalence, risk factors and long-term
reproductive outcome. Hum Reprod Update 2014;20:262-78. Crossref