© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE (HEALTHCARE IN MAINLAND CHINA)
Asthenopia prevalence and vision impairment severity among students attending online classes in low-income areas of western China during the COVID-19 pandemic
Y Ding, PhD1; H Guan, PhD1; K Du, PhD2; Y Zhang, PhD1; Z Wang, MD1; Y Shi, PhD1
1 Center for Experimental Economics for Education, Shaanxi Normal University, Xi’an, China
2 College of Economics, Xi’an University of Finance and Economics, Xi’an, China
Corresponding author: Dr H Guan (hongyuguan0621@gmail.com)
Abstract
Introduction: This study explored the impact of
online learning during the coronavirus disease 2019
(COVID-19) pandemic on asthenopia and vision
impairment in students, with the aim of establishing
a theoretical basis for preventive approaches to
vision health.
Methods: This balanced panel study enrolled
students from western rural China. Participant
information was collected before and during
the COVID-19 pandemic via questionnaires
administered at local vision care centres, along
with clinical assessments of visual acuity. Paired t
tests and fixed-effects models were used to analyse
pandemic-related differences in visual status.
Results: In total, 128 students were included (mean
age before pandemic, 11.82 ± 1.46 years). The mean
total screen time was 3.22 ± 2.90 hours per day
during the pandemic, whereas it was 1.97 ± 1.90
hours per day in the pre-pandemic period (P<0.001).
Asthenopia prevalence was 55% (71/128) during the
pandemic, and the mean visual acuity was 0.81 ± 0.30
logarithm of the minimum angle of resolution; these
findings indicated increasing vision impairment,
compared with the pre-pandemic period (both
P<0.001). Notably, asthenopia prevalence increased
by two- to three-fold, compared with the pre-pandemic period. An increase in screen time while learning was associated with an increase in
asthenopia prevalence (P=0.034).
Conclusion: During the COVID-19 pandemic,
students spent more time on online classes, leading to
worse visual acuity and vision health. Students in this
study reported a significant increase in screen time,
which was associated with increasing asthenopia
prevalence and worse vision impairment. Further
research is needed regarding the link between online
classes and vision problems.
New knowledge added by this study
- Online learning has become increasingly popular during the coronavirus disease 2019 pandemic. Students reported a nearly twofold increase in screen time during the pandemic, compared with the pre-pandemic period.
- Students reported greater asthenopia prevalence and demonstrated worse vision impairment during the pandemic, compared with the pre-pandemic period.
- Screen time was associated with asthenopia prevalence but not with the progression of vision impairment.
- Policymakers should carefully consider the prevalence of asthenopia and progression of vision impairment among students who are increasingly using digital devices and enrolling in online classes.
- Policies regarding vision care should be implemented in response to the increasing use of online learning approaches.
Introduction
The World Health Organization announced that the
coronavirus disease 2019 (COVID-19) outbreak had
become an international public health emergency on 30 January 2020; on 11 March 2020, it declared that
the outbreak had become a pandemic.1 Governments
and public health authorities worldwide implemented
public health policies to reduce the risk of viral transmission, including strict physical distancing,
severe travel restrictions, and the closure of many
businesses and schools. On 25 January 2020, China’s
Central Government announced a nationwide travel
ban and quarantine policy2; it initiated nationwide
school closures as an emergency measure to prevent
the spread of COVID-19.3 Thus, >220 million school-aged
children and adolescents were confined to their
homes; online classes were offered and delivered via
the internet.4
Vision problems are public health challenges;
among school-aged children, these problems
often involve asthenopia and vision impairment.
Asthenopia is defined as a subjective sensation of
visual fatigue, eye weakness, or eyestrain; it can
manifest through various symptoms, including
epiphora, ocular pruritis, diplopia, eye pain, and
dry eye.5 Vision impairment is defined as visual
acuity (VA) of 6/12 or worse in either eye6; it is
often caused by uncorrected refractive errors, and
its estimated prevalence is 43%.7 Although both
asthenopia and vision impairment have negative
effects on students, the effects of vision impairment
are greater. A previous global analysis revealed
that vision impairment was present in 12.8 million
children aged 5 to 15 years, half of whom lived in
China.8 Moreover, students with vision impairment have lower scores on various motor and cognitive
tests.9 10
Excessive use of digital devices contributes
to increases in asthenopia prevalence and vision
impairment among school-aged children.4 11 12 13 14 15 The
COVID-19 pandemic has led to increased use of
digital device–supported online classes,16 17 18 which
require extended exposure to those devices.19 20
Importantly, long durations of exposure to digital
devices can contribute to many vision problems in
children.14
Asthenopia and vision impairment related
to the excessive use of digital devices during the
COVID-19 pandemic have been investigated in
developed countries and urban China.4 11 12 To our
knowledge, no similar studies have been conducted
in western rural China. Additionally, online classes
are increasingly implemented in rural areas, and the
use of digital devices is becoming more prevalent11;
thus, there is a need for research that focus on vision
health in students.
The primary purpose of this study was to
assess screen time, asthenopia prevalence, and vision
impairment progression during the COVID-19
pandemic among students in western rural China.
To achieve this goal, we first conducted a general
descriptive analysis of student characteristics and
screen time trends before and during the pandemic.
We then investigated the prevalence of asthenopia
and progression of vision impairment. Finally,
we explored factors influencing the prevalence of asthenopia and progression of vision impairment before and during the pandemic.
Methods
Setting
This study focused on areas that were broadly
representative of rural western China because of
limited resources. Thus, the study was conducted
in Shaanxi and Ningxia regions in western China.
In 2019, the per capita gross domestic product in
Shaanxi Province was US$10 167; this is similar to
that in Ningxia Autonomous Region (US$8236).21
Sample selection
Vision data were acquired from local vision care
centres (VCs), which had been established by the
Center for Experimental Economics in Education
at Shaanxi Normal University, in cooperation
with county-level organisations such as the local
education ministries and hospitals.
Before the pandemic, VC screenings were
performed in each county, except during summer
and winter vacations. Staff conducted one to two
screenings per week (covering 2 to 4 schools); they
completed one round of screening in one town each
month. In practice, approximately 1 year is needed
to complete one round of vision screening for all
eligible children in a particular county. The second
round and subsequent rounds of vision screening
were performed using a similar workflow. After the completion of vision screening, students who
required further assessment were referred to the VC
for full eye and refractive examinations. This study
included students who had visited the VC 3 months
before the beginning of the COVID-19 pandemic.
During the pandemic, VC staff could not
attend schools to perform vision screenings. To
maintain vision screening services for students,
we telephoned all students who had visited the VC
before the pandemic. Participants in this panel study
were students who participated in data collection
before and during the COVID-19 pandemic.
Data collection
We conducted two cycles of surveys in the VC. The
first survey cycle was conducted from October to
December 2019 (before the pandemic); the second
survey cycle was conducted among a group of
students who visited the VC for follow-up from July
to December 2020 (during the pandemic), based on
their enrolment in the study before the pandemic.
The same information was collected during the
two survey cycles. During the vision screening
process, VC staff administered questionnaires to
students for collection of the following information:
sex (male=1), age, ethnicity (Han=1), residence
(non-rural=1), only-child status (yes=1), parental
education (parents with ≥12 years of education=1),
and parental migration status (one or both out-migrated=1; defined as one or both parents worked
away from home during the semester). Household
assets were calculated by summing the values of 13
items owned by the family, in accordance with the
China Rural Household Survey Yearbook.22
The survey also included the collection of
information regarding screen time and asthenopia.
Students completed a previously described, self-administered
questionnaire concerning mean time
spent throughout the day on near activities (including
computer and smartphone use, television viewing,
and studying/homework after school). Reports of
time spent on near activities during different parts
of the day were categorised as screen time while
learning and screen time while playing. Information
regarding asthenopia was collected via three
questions focused on ocular discomfort: whether the
student had experienced dry eyes (yes=1), eye pain
and swelling (yes=1), and eye fatigue and watery eyes
(yes=1). Asthenopia was defined as the presence
of at least one of these three types of vision health
problems (yes=1).23 Furthermore, information
regarding VA was collected when students visited
the VC. The optometrist in the VC conducted a VA
test to measure the clarity of each student’s vision.
All students completed VA tests without refractive
correction; students with spectacles completed VA
tests with their routine method of vision correction.
The questionnaire regarding asthenopia was developed and reviewed by a group of health experts
from Shaanxi Normal University and Zhongshan
Ophthalmic Center, a well-known ophthalmology
institution in China. The included questions were
constructed to ensure that they could be clearly
understood by students aged 9 to 17 years with the
aid of trained VC staff. These three questions can
serve as good indicators of symptoms representing
different degrees of asthenopia in students, and they
have been used in previous research.23
Visual acuity assessment
Visual acuity was assessed using Early Treatment
Diabetic Retinopathy Study tumbling-E charts
(Precision Vision, La Salle [IL], United States). In an
indoor area with sufficient light, VA was separately
assessed for each eye without refraction at a distance
of 4 m. Students were first examined using a 6/60
line; if they correctly identified the orientation of
at least four of five optotypes, they were examined
using a 6/30 line, followed by a 6/15 line and a 6/3
line. In this manner, the VA for an eye was defined as
the lowest line on which four of five optotypes were
correctly identified. If the participant could not read
the top line at a distance of 4 m, they were tested at a
distance of 1 m, and the VA result was divided by 4.
In this study, VA levels were calculated and
compared using the logarithm of the minimum angle
of resolution (logMAR) scale, which is a linear scale
with regular increments that offers a reasonably
intuitive interpretation of VA measurement.24 In this
study, vision impairment was defined as logMAR
≥0.3 (ie, VA of 6/12 or worse) in either eye.
Statistical methods
This balanced panel study compared student
data between two periods (before and during
the COVID-19 pandemic). Mean screen time,
asthenopia prevalence, and vision impairment
progression were compared among students using
t tests, after stratification according to various
demographic and behavioural factors. Fixed-effects
logistic and regression models were used to explore
factors influencing the prevalence of asthenopia and
progression of vision impairment before and during
the pandemic. Fixed-effects models were adjusted
for sex, age, ethnicity, rural or non-rural residence,
only-child status, parental migration status, parental
education level, household assets, screen time while
learning, and screen time while playing. All analyses
were performed using Stata Statistical Software,
version 14.1 (StataCorp, College Station [TX],
United States). All tests were two-sided, and P values
<0.05 were considered statistically significant.
Results
This study included 128 students from western rural China (mean age before pandemic, 11.82 ± 1.46
years; mean age during pandemic, 12.32 ± 1.54 years;
80 girls [62.5%] and 48 boys [37.5%]). All participants
had vision impairment and were attending online
classes (Table 1).
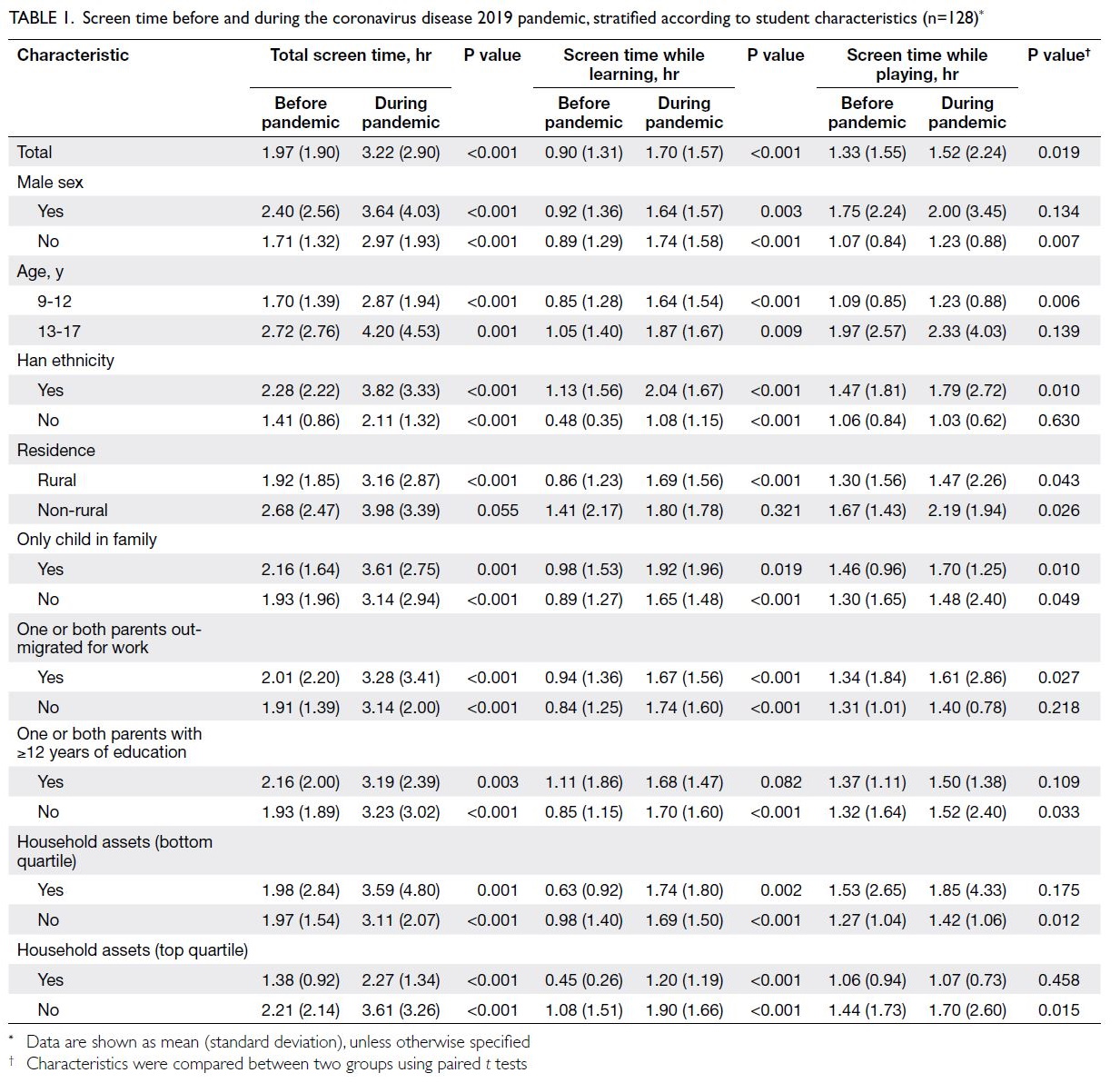
Table 1. Screen time before and during the coronavirus disease 2019 pandemic, stratified according to student characteristics (n=128)
During the pandemic, screen time significantly
increased because of enrolment in online classes.
The mean total screen time during the pandemic was
3.22 hours per day, compared with 1.97 hours during
the pre-pandemic period (P<0.001). The mean
screen time while learning during the pandemic was
1.70 hours per day, compared with 0.90 hours during
the pre-pandemic period (P<0.001); the mean screen time while playing during the pandemic was 1.52
hours per day, compared with 1.33 hours during the
pre-pandemic period (P=0.019). Additionally, rural
students had significantly greater screen time while
learning during the pandemic, compared with the
pre-pandemic period (P<0.001); there was no such
difference among non-rural students (Table 1).
The prevalence of asthenopia and progression
of vision impairment significantly differed between
the pandemic and pre-pandemic periods. The
prevalence of asthenopia during the pandemic was
55% (71/128), whereas it was 27% (35/128) during the
pre-pandemic period (P<0.001). The mean logMAR VA was worse during the pandemic compared with
the pre-pandemic period (0.81 vs 0.65; P<0.001).
The prevalence of asthenopia was higher during the
pandemic than during the pre-pandemic period,
regardless of the characteristics used to stratify
participants. The mean logMAR VA was worse
during the pandemic than during the pre-pandemic
period, although the difference being insignificant
among participants with non-Han ethnicity and
participants in the top quartile of household assets
(Table 2).
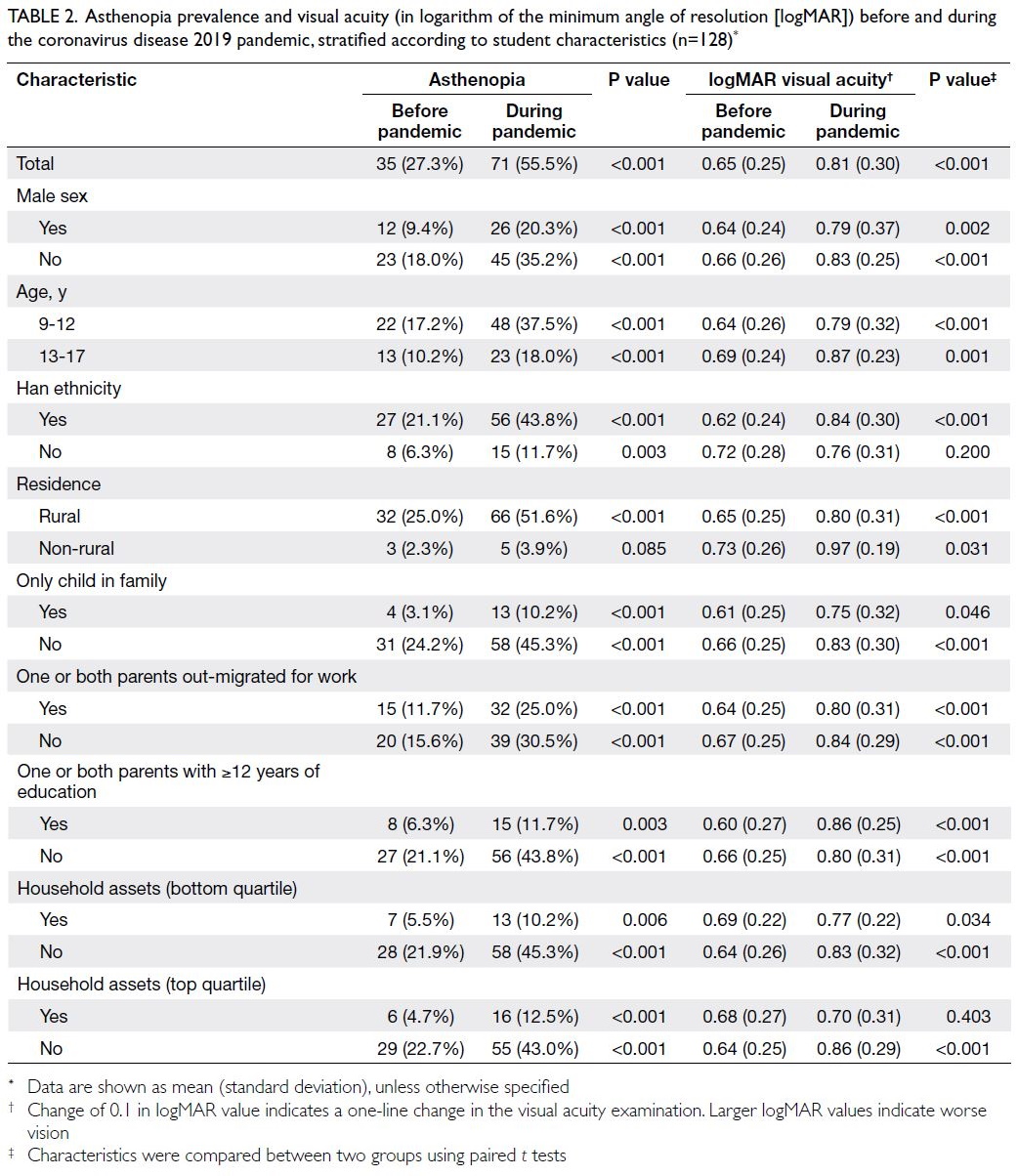
Table 2. Asthenopia prevalence and visual acuity (in logarithm of the minimum angle of resolution [logMAR]) before and during the coronavirus disease 2019 pandemic, stratified according to student characteristics (n=128)
Fixed-effects logistic models for asthenopia revealed that screen time while learning was
associated with asthenopia prevalence, and the
probability of asthenopia increased by 24.6% for
each 1-hour increase in screen time while learning
(95% confidence interval [CI]=1.02-1.53; P=0.034).
Additionally, older age (odds ratio [OR]=2.073,
95% CI=1.13-3.81, P=0.019), Han ethnicity
(OR=2.405, 95% CI=1.22-4.74; P=0.011), and only-child
status (OR=0.488, 95% CI=0.21-1.13; P=0.095)
were factors associated with asthenopia; screen time
while playing was not (Table 3).
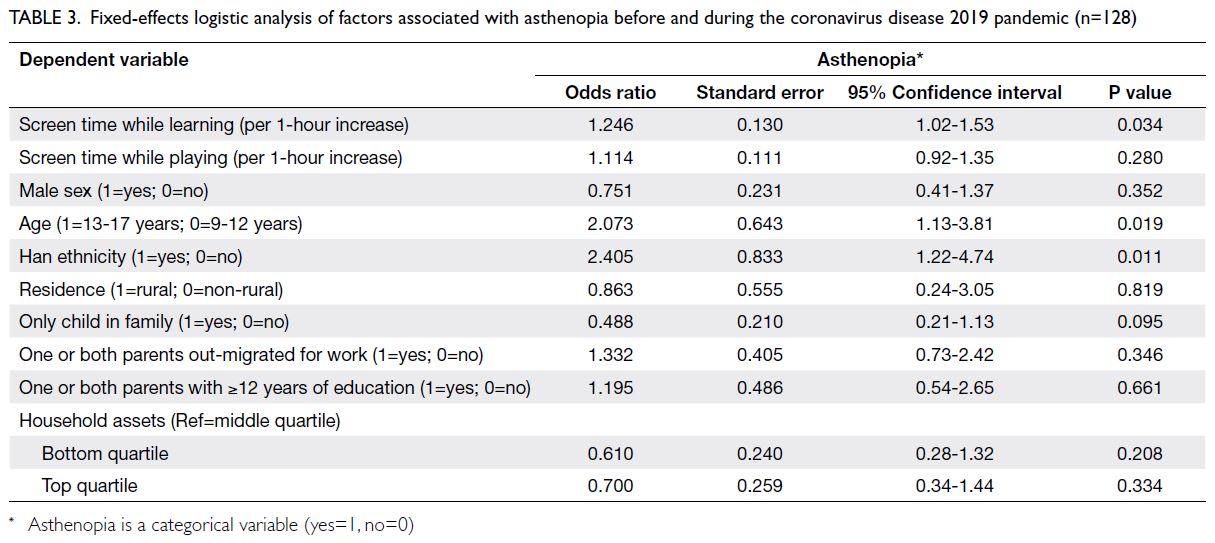
Table 3. Fixed-effects logistic analysis of factors associated with asthenopia before and during the coronavirus disease 2019 pandemic (n=128)
Fixed-effects regression models showed that residence in a non-rural area (OR=-0.200, 95%
CI=-0.355 to -0.046; P=0.011) and only-child status
(OR=-0.099, 95% CI=-0.197 to 0.000; P=0.049) were
factors associated with logMAR VA. The probability
of worse logMAR VA increased by 0.200 in non-rural
areas, compared with rural areas. However,
screen time while learning and screen time while
playing were not associated with vision impairment
(Table 4).
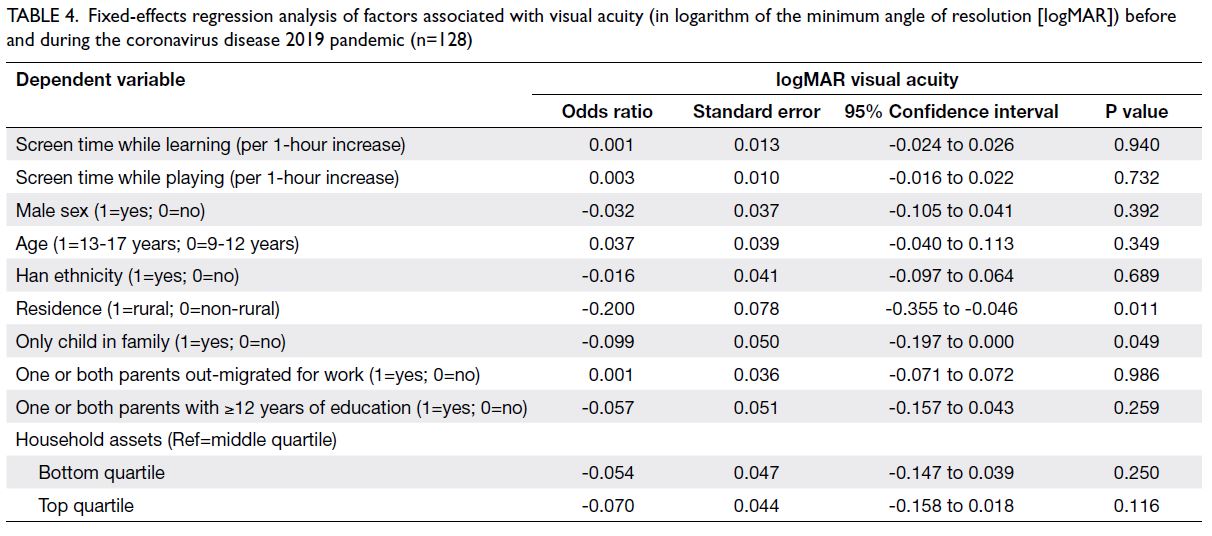
Table 4. Fixed-effects regression analysis of factors associated with visual acuity (in logarithm of the minimum angle of resolution [logMAR]) before and during the coronavirus disease 2019 pandemic (n=128)
Discussion
The global spread of the COVID-19 pandemic
has affected the education of >1.5 billion children
and adolescents worldwide.25 The participants in our study were representative of this important
population. They demonstrated declines in VA and
vision health during the pandemic, in relation to the
excessive use of digital devices; these findings were
consistent with the results of previous studies.19 26
All students in our study were attending online
classes during the pandemic. We observed an increase
in the mean daily time spent on digital devices
between the pre-pandemic and pandemic periods;
these results are consistent with international
findings that screen time was greater during the
pandemic than before the pandemic.19 Notably, we
found that total screen time and screen time while
learning significantly changed among rural students but not among non-rural students; these results
are also consistent with previous findings.19 This
difference presumably occurred because, compared
with rural students, non-rural students were more
likely to use digital devices and online classes before
the pandemic.
We observed a significant difference in
asthenopia prevalence among students in low-income
areas of western China before and during
the pandemic; this finding supports the results of
previous studies.26 27 Although the risk of asthenopia
reportedly increases with screen time,28 there
is no published literature concerning changes
in asthenopia among students in relation to the
COVID-19 pandemic. Similar to previous studies,14
we found that the prevalence of asthenopia was
approximately twofold greater among students aged
13 to 17 years than among those aged 9 to 12 years.
Furthermore, Moon et al26 reported that symptoms
of dry eye diseases were more common among
older children than among younger children. Older
children spend more time using digital devices,
leading to a higher prevalence of asthenopia.29
This study showed significant progression
of vision impairment in relation to the pandemic;
similarly, a study in eastern China revealed that
students had worse vision during the pandemic,
compared with their vision at pre-pandemic
examinations.4 However, screen time has not been
associated with vision impairment among students.
Furthermore, evidence regarding the impact of
digital devices use on vision impairment has been
inconsistent,30 31 with computer screen time made
students’ vision worse while television viewing
had no effect. We speculate that the association
will become clearer as school-aged children spend
increasing amounts of time using these devices.
This study had three important limitations.
First, the screen time data were retrospectively
collected through a self-reporting mechanism, which
may have led to recall bias. However, considering
the resource and measurement limitations that
researchers encountered during the pandemic, self-reported
recall was regarded as the optimal method
for collection of screen time data in the present
study. Second, the selection of students with poor
vision may lead to underestimation of screen time
effects on the general population, and the results
should be generalised with caution. Third, the study
was not designed to accurately distinguish between
vision impairment caused by intrinsic factors and
vision impairment caused by pandemic-related eye
strain.
Our findings provide new evidence regarding
the effects of increased screen time on asthenopia
and vision impairment among students in western
rural China during the pandemic; they can also serve
as a basis for future research. Although pandemic-related school closures are temporary, the increasing
popularity of online classes may accelerate the
overall acceptance of digital devices. The use of
online learning approaches is associated with
multiple vision problems, which merit attention in
future studies.
Conclusion
The present study demonstrated that asthenopia
and vision impairment among students in western
rural China were also affected by the pandemic;
these findings provide critical insights regarding
the effects of the pandemic on vision health in rural
students. Moreover, the findings highlight important
issues related to childhood vision health during the
pandemic; parents, teachers, and eye care providers
should consider evidence-based measures to avoid
asthenopia and vision impairment in children.
The current pace of economic and technological
development is leading to increased use of digital
devices and online learning approaches, but vision
problems in rural China have not received sufficient
consideration. Thus, there is a critical need for
greater efforts to monitor VA and vision health
among students in this region.
Author contributions
Concept or design: All authors.
Acquisition of data: Y Ding, H Guan, K Du.
Analysis or interpretation of data: Y Ding, H Guan, K Du, Y Shi.
Drafting of the manuscript: Y Ding, Y Zhang, Z Wang.
Critical revision of the manuscript for important intellectual content: H Guan, Y Shi.
Acquisition of data: Y Ding, H Guan, K Du.
Analysis or interpretation of data: Y Ding, H Guan, K Du, Y Shi.
Drafting of the manuscript: Y Ding, Y Zhang, Z Wang.
Critical revision of the manuscript for important intellectual content: H Guan, Y Shi.
All authors contributed to the study, approved the final version for publication, and take responsibility for its accuracy
and integrity.
Conflicts of interest
As an International Editorial Advisory Board member of the journal, Y Shi was not involved in the peer review process.
Other authors have disclosed no conflicts of interest.
Acknowledgement
We thank Dr Wenting Liu, Dr Jiaqi Zhu, and staff from the Center for Experimental Economics in Education of Shaanxi
Normal University, China for their valuable contributions.
Funding/support
H Guan received funding for this study from the National Natural Science Foundation of China (Grant No.: 7180310)
and Soft Science Project of Shaanxi Province (Grant No.: 2023-CX-RKX-127). Y Ding received funding for this study from
the Fundamental Research Funds for the Central Universities
(Grant No.: 2020CSWY018). This study was supported by the
111 Project (Grant No.: B16031). The funders had no role in
designing the study, collecting, analysing or interpreting the
data, or in drafting this manuscript.
Ethics approval
This study protocol was approved by Sun Yat-sen University,
China (Registration No.: 2013MEKY018) and all procedures
followed the principles of the Declaration of Helsinki.
Permission was obtained from the local boards of education
in the study area, as well as the principals of all participating
schools. All participating children provided oral assent before
baseline data collection, and legal guardians provided written
informed consent for their children to be enrolled in the study.
References
1. World Health Organization. WHO timeline—COVID-19. 2020. Available from: https://www.who.int/news-room/detail/27-04-2020-who-timeline---covid-19. Accessed 13 Sep 2021.
2. Li D, Liu Z, Liu Q, et al. Estimating the efficacy of quarantine and traffic blockage for the epidemic caused by 2019-nCoV (COVID-19): a simulation analysis. medRxiv [Preprint]. 25 Feb 2020. Available from: https://doi.org/10.1101/2020.02.14.20022913. Accessed 13 Sep 2021. Crossref
3. Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet 2020;395:945-7. Crossref
4. Wang J, Li Y, Musch DC, et al. Progression of myopia in school-aged children after COVID-19 home confinement. JAMA Ophthalmol 2021;139:293-300. Crossref
5. Kowalska M, Zejda JE, Bugajska J, Braczkowska B, Brozek G, Malińska M. Eye symptoms in office employees working at computer stations [in Polish]. Med Pr 2011;62:1-8.
6. Cumberland PM, Peckham CS, Rahi JS. Inferring myopia over the lifecourse from uncorrected distance visual acuity
in childhood. Br J Ophthalmol 2007;91:151-3. Crossref
7. Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol 2012;96:614-8. Crossref
8. Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP. Global magnitude of visual impairment caused by uncorrected
refractive errors in 2004. Bull World Health Organ 2008;86:63-70. Crossref
9. Jan C, Li SM, Kang MT, et al. Association of visual acuity with educational outcomes: a prospective cohort study. Br
J Ophthalmol 2019;103:1666-71. Crossref
10. Roch-Levecq AC, Brody BL, Thomas RG, Brown SI. Ametropia, preschoolers’ cognitive abilities, and effects of
spectacle correction. Arch Ophthalmol 2008;126:252-8. Crossref
11. Zhang Z, Xu G, Gao J, et al. Effects of e-learning environment use on visual function of elementary and middle school
students: a two-year assessment—experience from China.
Int J Environ Res Public Health 2020;17:1560. Crossref
12. Wong CW, Tsai A, Jonas JB, et al. Digital screen time during COVID-19 pandemic: risk for a further myopia boom? Am J Ophthalmol 2021;223:333-7. Crossref
13. Kim J, Hwang Y, Kang S, et al. Association between sexposure to smartphones and ocular health in adolescents.
Ophthalmic Epidemiol 2016;23:269-76. Crossref
14. Mohan A, Sen P, Shah C, Jain E, Jain S. Prevalence and risk factor assessment of digital eye strain among children
using online e-learning during the COVID-19 pandemic:
digital eye strain among kids (DESK study-1). Indian J
Ophthalmol 2021;69:140-4. Crossref
15. Guan H, Yu NN, Wang H, et al. Impact of various types of near work and time spent outdoors at different times of day on visual acuity and refractive error among Chinese school-going children. PLoS One 2019;14:e0215827.Crossref
16. Sultana A, Tasnim S, Hossain MM, Bhattacharya S,
Purohit N. Digital screen time during the COVID-19
pandemic: a public health concern. Available from: https://f1000research.com/articles/10-81. Accessed 13 Sep 2021. Crossref
17. Nigg CR, Wunsch K, Nigg C, et al. Are physical activity,
screen time, and mental health related during childhood,
preadolescence, and adolescence? 11-year results from
the German Montorik–Modul Longitudinal Study. Am J
Epidemiol 2021;190:220-9. Crossref
18. Schmidt SC, Anedda B, Burchartz A, et al. Physical activity
and screen time of children and adolescents before and
during the COVID-19 lockdown in Germany: a natural
experiment. Sci Rep 2020;10:21780. Crossref
19. Aguilar-Farias N, Toledo-Vargas M, Miranda-Marquez S,
et al. Sociodemographic predictors of changes in physical
activity, screen time, and sleep among toddlers and
preschoolers in Chile during the COVID-19 pandemic. Int
J Environ Res Public Health 2020;18:176. Crossref
20. Bates LC, Zieff G, Stanford K, et al. COVID-19 impact on behaviors across the 24-hour day in children and
adolescents: physical activity, sedentary behavior, and
sleep. Children (Basel) 2020;7:138. Crossref
21. National Bureau of Statistics of China, PRC Government. China Statistical Yearbook 2020. Available from: http://www.stats.gov.cn/tjsj/ndsj/2020/indexch.htm. Accessed 14
Sep 2021.
22. National Bureau of Statistics of China, PRC Government. China Statistical Yearbook 2013. Beijing, China: China
State Statistical Press; 2013.
23. Seguí Mdel M, Cabrero García J, Crespo A, Verdú J, Ronda E. A reliable and valid questionnaire was developed to measure computer vision syndrome at the workplace. J Clin Epidemiol 2015;68:662-73. Crossref
24. Yi H, Zhang L, Ma X, et al. Poor vision among China’s rural primary school students: prevalence, correlates and
consequences. China Econ Rev 2015;33:247-62. Crossref
25. United Nations International Children’s Emergency Fund.
Don’t let children be the hidden victims of COVID-19
pandemic. Available from: https://www.unicef.org/press-releases/dont-let-children-be-hidden-victims-covid-19-pandemic. Accessed 6 Oct 2020.
26. Moon JH, Kim KW, Moon NJ. Smartphone use is a risk factor for pediatric dry eye disease according to region and
age: a case control study. BMC Ophthalmol 2016;16:188. Crossref
27. Moon JH, Lee MY, Moon NJ. Association between video display terminal use and dry eye disease in school children.
J Pediatr Ophthalmol Strabismus 2014;51:87-92. Crossref
28. Rechichi C, De Mojà G, Aragona P. Video game vision syndrome: a new clinical picture in children? J Pediatr
Ophthalmol Strabismus 2017;54:346-55.Crossref
29. Mowatt L, Gordon C, Santosh AB, Jones T. Computer vision syndrome and ergonomic practices among undergraduate
university students. Int J Clin Pract 2018;72:e13035. Crossref
30. Terasaki H, Yamashita T, Yoshihara N, Kii Y, Sakamoto T. Association of lifestyle and body structure to ocular axial
length in Japanese elementary school children. BMC
Ophthalmol 2017;17:123. Crossref
31. Fernández-Montero A, Olmo-Jimenez JM, Olmo N, et al. The impact of computer use in myopia progression: a
cohort study in Spain. Prev Med 2015;71:67-71. Crossref

