Hong Kong Med J 2023 Apr;29(2):142–9 | Epub 29 Mar 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Effect of location on out-of-hospital cardiac arrests involving older adults in Hong Kong: secondary analysis of a territory-wide cohort
Ronald TM Wong, MB, BS, FHKAM (Emergency Medicine)
Department of Emergency Medicine, The University of Hong Kong, Hong Kong SAR, China
Corresponding author: Dr Ronald TM Wong (drwongtmr@gmail.com)
Abstract
Introduction: Most out-of-hospital cardiac arrests
in Hong Kong involve older adults. The likelihood
of survival varies among locations. This study
investigated patient and bystander characteristics,
as well as the timing of interventions, that affect
the prevalences of shockable rhythm and survival
outcomes among cardiac arrests involving older
adults in homes, on streets, and in other public
places.
Methods: This secondary analysis of a territory-wide historical cohort used data collected by the Fire
Services Department of Hong Kong from 1 August
2012 to 31 July 2013.
Results: Bystander cardiopulmonary resuscitation
was primarily performed by relatives in homes but
not in non-residential locations. The intervals in
terms of receipt of emergency medical services
(EMS) call, initiation of bystander cardiopulmonary
resuscitation, and receipt of defibrillation were
longer for cardiac arrests that occurred in homes.
The median interval for EMS to reach patients was
3 minutes longer in homes than on streets (P<0.001).
Forty-seven percent of patients who developed
cardiac arrest on streets had a shockable rhythm within the first 5 minutes after receipt of EMS call.
Defibrillation within 15 minutes after receipt of EMS
call was an independent predictor of 30-day survival
(odds ratio=4.07; P=0.02). Fifty percent of patients
who received defibrillation within 5 minutes in non-residential
locations survived.
Conclusion: There were significant location-related
differences in patient and bystander characteristics,
interventions, and outcomes among cardiac arrests
involving older adults. A large proportion of patients
had a shockable rhythm in the early period after
cardiac arrest. Good survival outcomes in out-of-hospital
cardiac arrests involving older adults can be
achieved through early bystander defibrillation and
intervention.
New knowledge added by this study
- Among out-of-hospital cardiac arrests involving older adults that occurred at different locations, there were significant differences in patient and bystander characteristics, as well as prehospital interventions, which influenced survival outcomes.
- Many older adults who experienced cardiac arrest in non-residential locations had a shockable rhythm in the early period after receipt of emergency medical services (EMS) call, and early defibrillation was associated with favourable survival outcomes.
- Low rates of shockable rhythm and significant delays in bystander and EMS processes were observed within homes.
- Additional measures are needed to overcome bystander inertia.
- Interventions to mitigate the adverse factors related to cardiac arrests occurring in older adult households, such as volunteer dispatch via mobile applications, should be considered.
Introduction
The proportion of older adults in Hong Kong is
expected to increase from 18% in 2019 to 26% by
the year 2029.1 Overcrowding is a serious problem,
such that population densities of 57 530 people/km2
are present in ageing districts.2 3 Most residents
of Hong Kong live in high-rise apartments that require elevators for access, but most elevators
cannot accommodate an ambulance stretcher with
a patient in a supine position.4 More than 50%
of out-of-hospital cardiac arrest (OHCA) events
occur in private homes, a location that is associated
with poor survival outcomes.5 The proportion of
domestic households consisting solely of people aged ≥65 years has increased by approximately
24% between 2011 and 2016, from 8.4% to 10.4%.6
Considering these demographic changes, there is
a need for improved overall understanding of the
prehospital management of cardiac arrests that
involve older adults in homes and other locations.
This study investigated patient characteristics, types
of bystanders involved, and prehospital interventions
that were associated with differences in survival
outcomes among cardiac arrests involving older
adults in homes, compared with cardiac arrests on
streets and in public areas excluding streets (PAES).
Methods
Study design and setting
This secondary analysis focused on a historical
cohort from a previous study.5 The Emergency
Ambulance Service of the Fire Services Department
(FSD) provides most emergency medical services
(EMS) in Hong Kong through a one-tiered system
that serves the entire 1104 km2 region. At the time
of data collection, the population was around 7.1
million.7 Ambulance personnel are required to
perform cardiopulmonary resuscitation (CPR) on
and transfer most cases of OHCA to hospitals. A
small number of patients with obvious post-mortem
changes (eg, rigor mortis) may be directly transferred
to the public mortuary; such patients were not
included in this study. Fire Services Department ambulances will only transfer patients to emergency
departments under the Hospital Authority. At the
time of data collection, callers requesting for EMS
for OHCA patients were not provided with post-dispatch
instructions to perform CPR.
Participants
This secondary analysis included all patients with
OHCA who were transferred to the Emergency
Departments (EDs) by FSD ground ambulances
from 1 August 2012 to 31 July 2013. Exclusion
criteria were cardiac arrests caused by trauma,
patients not transferred by ground ambulance, and
patients directly transferred to the public mortuary.
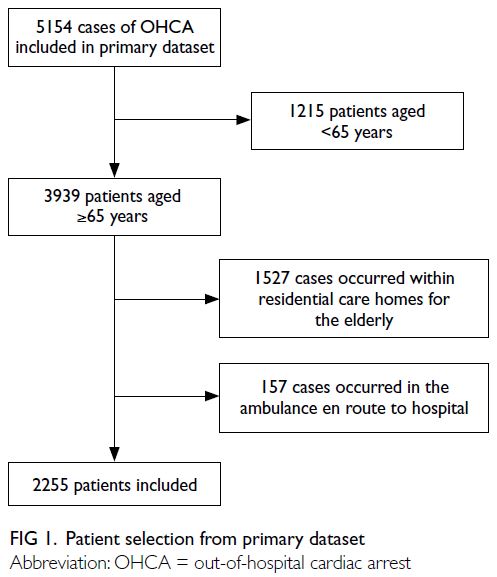
After patient selection from the primary dataset,
the following additional exclusions were made:
cardiac arrests that involved patients aged <65
years, occurred within residential care homes for
the elderly, or occurred in the ambulance en route
to hospital.
Data sources
Data regarding patient characteristics and prehospital
management were prospectively collected by EMS
personnel who were directly involved in prehospital
care for patients who experienced OHCA. The
collected data included patient age and sex, location
of cardiac arrest, whether the cardiac arrest was
witnessed and the identity of the witness, whether
bystander CPR was performed and who performed
it, whether defibrillation with an automated
external defibrillator (AED) was performed, what
electrocardiogram rhythm was first detected, the
timings of prehospital events (recognition of cardiac
arrest, receipt of EMS call, initiation of bystander
CPR, initiation of first defibrillation, EMS arrival at
patient’s side, initiation of CPR by EMS personnel,
and arrival at the ED), and return of spontaneous
circulation (ROSC) before ED arrival.
Electronic medical records at the relevant
ED (Accident and Emergency Information System,
Hong Kong Hospital Authority) were reviewed
to determine the time of defibrillation and time
of ROSC at the ED, as well as whether a patient
survived until admission. A patient was assumed to
have received no resuscitative intervention unless
specific documentation was present in the ED record.
Neurological status upon discharge and survival at
30 days after cardiac arrest were determined from
a territory-wide electronic medical record database
(Clinical Management System, Hong Kong Hospital
Authority).
Variables
Streets were defined as paved thoroughfares for
pedestrians, including sidewalks. Public areas
excluding streets were other areas that were accessible by the public throughout the day; these
included outdoors (eg, parks and markets) and
indoor facilities (eg, eateries, places of recreation,
and day care facilities for older adults). Bystanders
were defined in accordance with the guidelines
of the Utstein Resuscitation Registry Templates
for Out-of-Hospital Cardiac Arrest.8 Fire Services
Department first responders dispatched to the
scene were classified as EMS personnel. Older adult
care workers (OACWs) are individuals who care
for residents in various private and public housing
arrangements for older adults. Older adult care
workers accompanying patients were not dispatched
as part of the organised emergency rescue team;
thus, they were classified as bystanders. Public access
defibrillation (PAD) was defined as a defibrillation
shock delivered from an AED when a bystander
performed CPR. Shocks delivered when FSD first
responders performed CPR were excluded.
Time intervals were rounded to the nearest
minute. The decision interval was the interval
between recognition of cardiac arrest and receipt
of EMS call. Call-to-bystander CPR was the interval
between receipt of EMS call and initiation of
bystander CPR. Call-to-EMS arrival was the interval
between receipt of EMS call and EMS arrival at the
patient’s side. Time of first defibrillation was defined
as the time of the earliest of the following three
events: PAD, defibrillation by EMS, or defibrillation
in the ED. Call-to-bystander CPR intervals were
grouped as 0-2, 3-5, 6-8, 9-11, and 12-31 minutes, as
well as no bystander CPR. Call-to-first defibrillation
intervals were grouped as 0-5, 6-10, 11-15, 16-20,
and 21-55 minutes, as well as no defibrillation (>55
minutes/not applicable).
Post-cardiac arrest neurological status was
classified using the 5-point Glasgow-Pittsburgh
Cerebral Performance Categories (CPC) scale. In
the scale, CPC 1 represents patients with good
cerebral performance; CPC 2 includes patients who
can manage activities of daily living independently
or participate in part-time work in a sheltered
environment; CPC 3 to CPC 5 ranges from patients
who are unable to live independently because of
cerebral disability to patients who have experienced
brain death. Patients with CPC 1 or CPC 2 were
presumed to have a favourable neurological outcome.
Statistical methods
Patient characteristics, interventions, and outcomes were analysed using descriptive statistics. Pearson’s
χ2 test was used to compare categorical variables;
Fisher’s exact test was used if >20% of expected counts
were <5. The Kruskal–Wallis rank sum test was used
to compare non-parametric time intervals. A P value
of <0.05 was considered statistically significant.
Predictors of 30-day survival were analysed using
univariate and multivariate logistic regression; findings were reported as odds ratios (ORs) with
95% confidence intervals. Adjusted variables
included age; sex; arrest location; person witnessing
the arrest (relative, OACW or other bystanders,
EMS personnel, or unwitnessed); person performing
bystander CPR (no bystander CPR, OACW, relative,
or other); PAD (yes or no); first monitored rhythm
(asystole, pulseless electrical activity, ventricular
fibrillation/ventricular tachycardia); and call-to-EMS arrival, call-to-bystander CPR, and call-to-first
defibrillation intervals.
Statistical analysis was performed using R
software, version 3.6.1 (R Foundation for Statistical
Computing, Austria). The original study was
approved by the Institutional Review Board of
The University of Hong Kong/Hospital Authority
Hong Kong West Cluster (Ref No.: UW 15-599).
No new data were collected for secondary analysis.
This manuscript was prepared in accordance with
the STROBE (Strengthening the Reporting of
Observational Studies in Epidemiology) reporting
guidelines.
Results
Participant selection and characteristics
Figure 1 describes patient selection from the primary
dataset. The original cohort comprised 5154 patients
with OHCA who were transferred to the ED by
FSD ground ambulances. After the application of
exclusion criteria, 2255 patients were included in the
analysis. Table 1 compares the patient and bystander
characteristics, interventions, and outcomes of OHCA occurring in homes, in PAES, and on streets.
Patients who experienced cardiac arrest in homes
were significantly older (approximately 5 years;
P<0.001) than patients who experienced cardiac
arrest on streets or in PAES. In all groups, there
were more male patients; the sex disparity was the
greatest in the streets group, followed by the PAES
group.
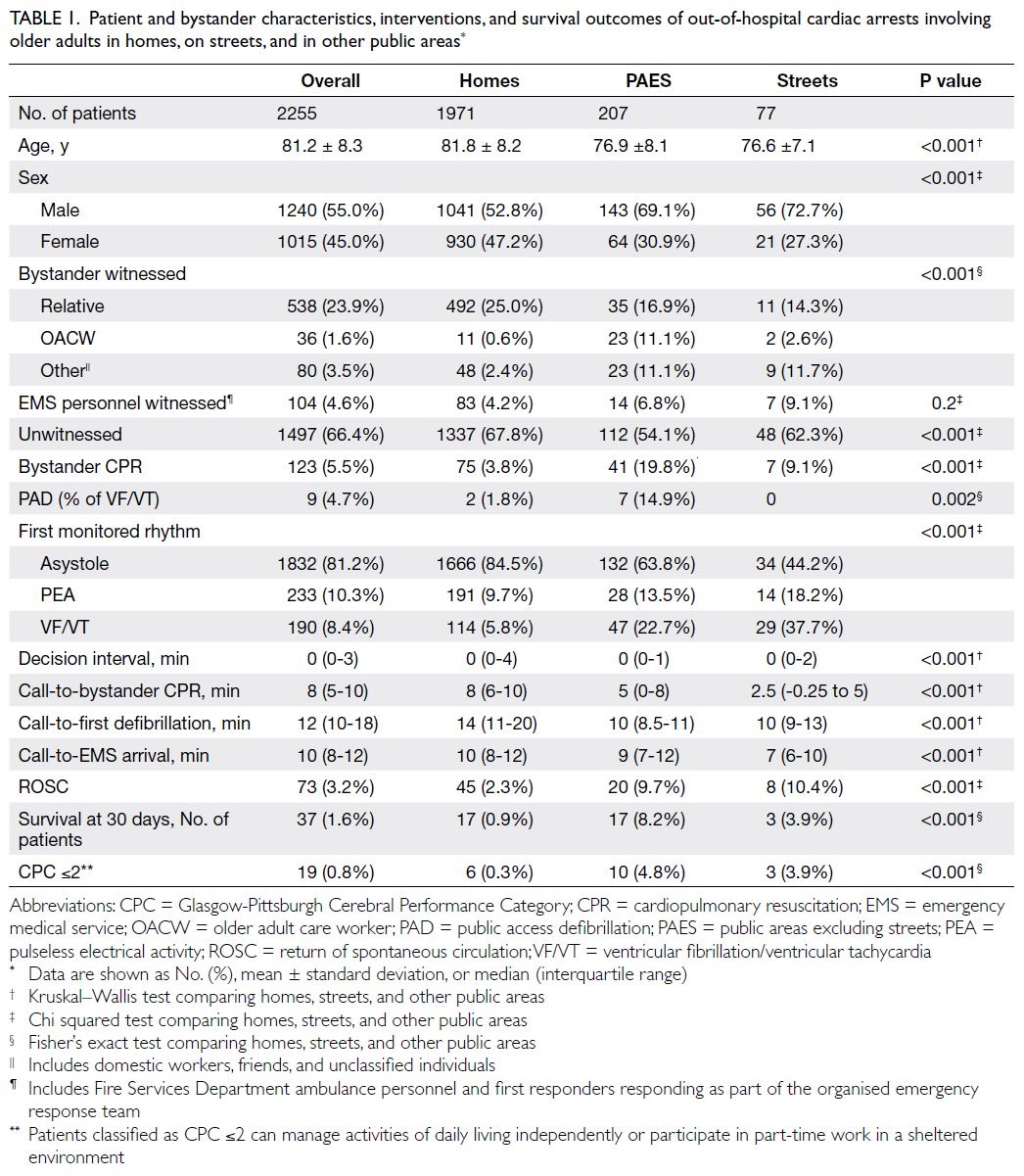
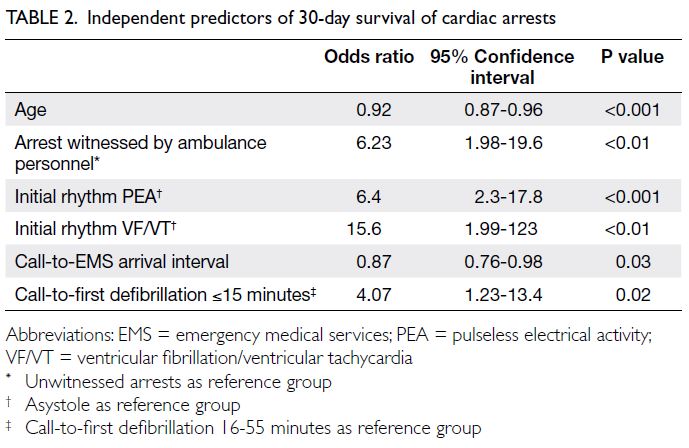
Table 1. Patient and bystander characteristics, interventions, and survival outcomes of out-of-hospital cardiac arrests involving older adults in homes, on streets, and in other public areas
Furthermore, most cardiac arrests (66.4%
among all patients; P<0.001; Table 1) were
unwitnessed. Relatives were the most common type
of bystander present in witnessed arrests, whereas there were significant differences in the involvement
of OACWs, EMS personnel, and other individuals at
the three locations. Compared with EMS personnel,
there were more OACWs as bystanders in PAES and
more bystanders, represented by the ‘other’ group, in
PAES and on streets. There was a significant difference
in the proportion of bystanders performing CPR
among the three locations (P<0.001), as illustrated
in Figure 2. The bystander CPR rate was the highest in PAES and the lowest in homes. Among the nine
patients who received PAD, six received it when
OACWs provided CPR in PAES.
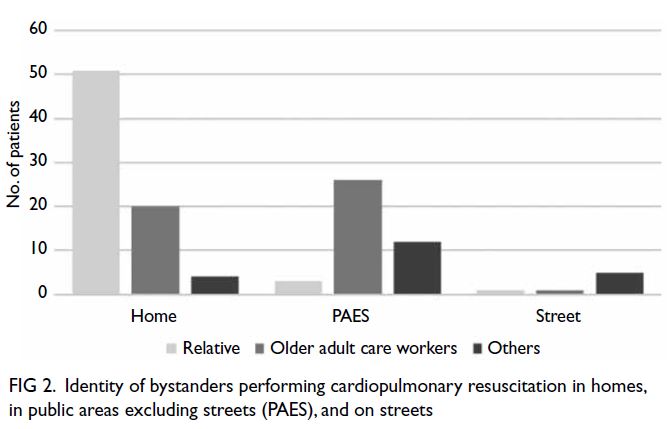
Figure 2. Identity of bystanders performing cardiopulmonary resuscitation in homes, in public areas excluding streets (PAES), and on streets
Initial monitored rhythm
Notably, asystole was the most common initial
monitored rhythm (81.2% among all patients;
P<0.001; Table 1). However, cardiac arrests on
streets and in PAES had significantly higher rates of
shockable rhythm and PEA, compared with cardiac
arrests in homes. The prevalences of shockable
rhythm relative to the time from receipt of EMS call
and the location of cardiac arrest are shown in Figure 3. The highest rates of shockable initial rhythm (SIR)
were observed within the first 5 and 10 minutes after
receipt of EMS call for cardiac arrests on streets,
which were 47% (8/17) and 41% (17/42), respectively.
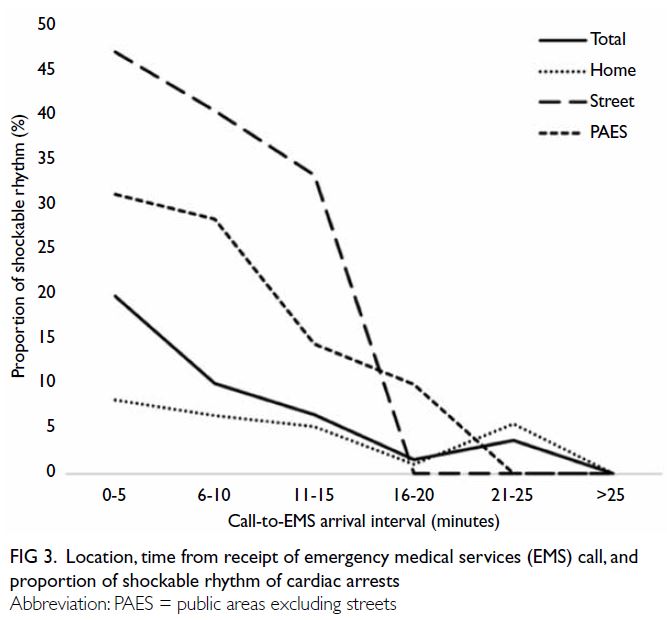
Figure 3. Location, time from receipt of emergency medical services (EMS) call, and proportion of shockable rhythm of cardiac arrests
Timing of interventions
Patients with cardiac arrest in homes had
significantly longer intervals in terms of receipt of
EMS call, initiation of bystander CPR, and receipt
of defibrillation (all P<0.001; Table 1). The median
interval for EMS to reach patients was 3 minutes
longer in homes than on streets. The interval between
recognition of cardiac arrest and receipt of EMS call
was 0 minutes in 57.5% of patients (1297/2255).
Survival and neurological outcomes
Additionally, patients with cardiac arrest in homes had significantly lower rates of ROSC, 30-day
survival, and favourable neurological outcomes (all
P<0.001; Table 1).
Independent predictors of 30-day survival are
shown in Table 2. Older age and longer call-to-EMS
arrival interval both decreased the overall likelihood
of survival (ORs of 0.92 and 0.87, respectively).
Pulseless electrical activity and ventricular
fibrillation/ventricular tachycardia increased the
likelihood of survival compared with asystole
(ORs of 6.4 and 15.6, respectively). Cardiac arrest
witnessed by EMS personnel and defibrillation
within 15 minutes after receipt of EMS call increased
the overall likelihood of survival (ORs of 6.23 and
4.07, respectively).
The relationship among the location, timing of
defibrillation, and 30-day survival of cardiac arrest
is shown in Figure 4. Overall, patients who received
defibrillation within 5 minutes and at 6 to 10 minutes
after receipt of EMS call had survival rates of 33%
(2/6) and 17% (15/86), respectively. For patients who
received defibrillation on streets/in PAES within
5 minutes and at 6 to 10 minutes after receipt of
EMS call, the survival rates were 50% (2/4) and 22%
(10/45), respectively. Two patients in the homes
group received defibrillation within 5 minutes; the
survival rate was 0% (0/2).
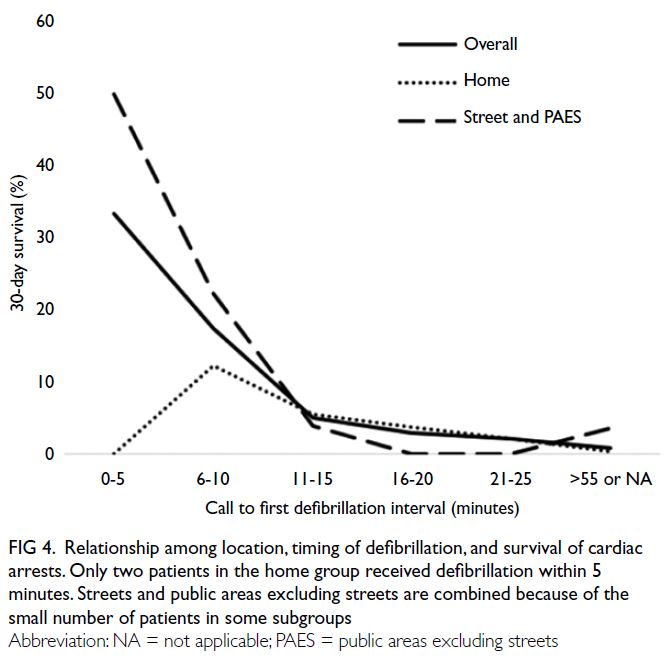
Figure 4. Relationship among location, timing of defibrillation, and survival of cardiac arrests. Only two patients in the home group received defibrillation within 5 minutes. Streets and public areas excluding streets are combined because of the small number of patients in some subgroups
Cardiac arrest at home was a predictor
of survival in univariate analysis (OR=0.076,
95% confidence interval [CI]=0.038-0.15) but not in
multivariable analysis (OR=0.65, 95% CI=0.22-1.90). The effect of location on survival was mediated by the first monitored rhythm, and the call-to-EMS arrival interval.
Discussion
This study investigated factors that affect the
prevalences of shockable rhythm and survival
outcomes among cardiac arrests involving older
adults in Hong Kong. The patient characteristics,
proportion of witnessed arrests, and rates of SIR
and PAD for cardiac arrests involving older adults in homes were similar between the present study and
a previous analysis in Japan.9 Unlike many western
countries, EMS personnel in Hong Kong and Japan
generally do not terminate resuscitation in the field;
this similarity facilitates comparison of data between
the two studies. A notable difference was that in
Japanese homes, 45% of older patients received
bystander CPR; this receipt of CPR was associated
with rate of ROSC, 30-day survival, and favourable
neurological outcomes that were threefold higher
than the corresponding rates in Hong Kong.
Bystander cardiopulmonary resuscitation
The bystander CPR rate in Hong Kong homes was
low (3.8%) [Table 1], and there was a substantial
delay in its initiation. Although the type of relatives
involved as bystanders was not recorded in the
present study, considering the proportion of older
adult households in Hong Kong,6 many of the
relatives presumably were cohabiting older adults.
Such individuals may not be able to follow telephone
instructions to perform CPR because of physical
limitations or emotional distress10; thus, the provision
of post-dispatch instructions and enhancement of
community-wide CPR training will not improve
survival among these patients.11 Although high-rise
apartments create barriers to EMS personnel, they
also increase the likelihood that trained volunteers
will be present in the vicinity, where they may be
dispatched using mobile applications.12 13 14
In non-residential locations, most bystanders
performing CPR were not relatives of the patients.
Fear of legal consequences is reportedly a major
cause for intervention inertia in this situation.15 A
previous survey in Hong Kong, in which one-third of
respondents had prior first aid training, revealed that
nearly all respondents were willing to call for help
but only one-fifth were willing to perform bystander
CPR.16 These findings suggest that knowledge
transfer is insufficient to overcome bystander
inertia in Hong Kong. Training programmes should
ensure that factors inhibiting intervention (eg, legal
concerns, fear of disease transmission, and bystander
effect) are addressed.17 18
Shockable initial rhythm
Previous studies in Hong Kong revealed low rates of SIR in patients with OHCA, ranging from 5% to 14%,
along with dismal survival rates of 0.6% to 3%.1 19 20
These low rates imply that aggressive bystander
interventions (eg, defibrillation for older adults)
are futile. However, the findings of the present
study indicate that older adults in non-residential
locations have much higher SIR rates in the initial
10 minutes after receipt of EMS call; moreover, early
defibrillation is an independent predictor of survival
among such patients, and high survival rates can be
achieved with early defibrillation.
The present study revealed a 2% per-minute
decrease in the rate of SIR. This is similar to
the findings in a large multinational study from
northern Europe.21 Differences in SIR rates between
residential and non-residential locations may be
partly related to patient factors (eg, age and presence
of co-morbidities); they could also be related to
differences in the decision interval (ie, time elapsed
between recognition of cardiac arrest [as reported
by a bystander] and receipt of EMS call). A previous
study in Hong Kong showed that efforts to seek advice from relatives often contributed to delayed
receipt of EMS call.4 Longer decision intervals
and consequential delays in EMS arrival lead to
interactions with later parts of the shockable rhythm
downslope and lower SIR rates. In practice, the recall
of decision intervals by bystanders is unreliable.
This is consistent with the decision interval of 0
minutes reported by most bystanders in the present
study. Despite this confounding factor, the findings
in this study indicate that bystanders should not
hesitate to provide aggressive resuscitation and early
defibrillation for older patients.
Public access defibrillation
Notably, very few patients received PAD in this
study, and most instances of PAD administration
were performed by OACWs in PAES. According to a
nationwide study in Japan, 16.5% of patients received
PAD during witnessed ventricular fibrillation
cardiac arrest.22 Estimation of the AED coverage
rate in Hong Kong using a horizontal level walking
route distance model revealed that only 11% of
patients with OHCA would have an AED within
100 m.23 Considering the large number of OHCA
events occurring within high-rise buildings,
the actual coverage rate is presumably lower.
Furthermore, there is evidence that most people in
Hong Kong do not know the location of the AED
nearest to their home or workplace.16 Unless AEDs
are easy to locate and readily accessible at all times,
PAD rates will remain low.24
Barriers to rescue in high-rise buildings
In a previous study in Hong Kong, the proportions
of patients with OHCA who could be accessed by
elevator or stairs and by stairs alone were 74% and
14%, respectively.4 In the present study, the median
interval for EMS to reach patients was 3 minutes
longer in homes than on streets. This represents the
‘vertical response time’ component of the call-to-EMS arrival interval.25 In a previous study, survival
was lower among patients who experienced cardiac
arrest at higher levels within buildings.26 Nearly 70%
of lifts in Hong Kong do not have sufficient area to
accommodate the ambulance stretcher.4 Therefore,
the vertical response time leads to a delay in EMS
interventions and deterioration in CPR quality,
both of which may contribute to the poor outcomes
of cardiac arrests that occur in homes. The use of
circulatory adjuncts to enhance cerebral perfusion
during head-up position CPR within lifts should be
considered.27
Limitations
Importantly, only patients transported to hospital by FSD ground ambulances were included in this study;
a small number of patients with OHCA may have been transported to hospital by other means.
Furthermore, data regarding the timings of
recognition of cardiac arrest, bystander CPR, and
PAD obtained from bystanders may have been
subject to response bias. The lack of blinding of
emergency department personnel towards patient
factors (eg, absence of shockable rhythm and
prehospital defibrillation, longer time to ROSC,
co-morbidities, and advanced age) may have led
to selection bias regarding treatment decisions,
including the termination of resuscitation,
arrangement of intensive care unit resources, and
coronary angiography; such bias has been reported
to negatively influence the survival rate.28 Data
regarding pre-arrest co-morbidity and functional
status were not available, which may have resulted
in a confounding effect on survival outcomes.
Additionally, a small number of patients received
defibrillation within 5 minutes. All of the factors
listed here may have affected the accuracy of
conclusions drawn from this subset.
This study was based on territory-wide data
collected in 2012 to 2013. Thus, it may not reflect
the current situation because of changes in patient
demography, prevalence of shockable rhythm, and
survival enhancement interventions introduced in
the past several years. A large multinational study in
northern Europe investigated the rate of SIR among
OHCA events occurring in residential and public
locations from 2006 to 2015. The rate of SIR in
public locations remained stable during that period.
A decrease was observed in residential locations
between 2006 and 2010, but the proportion has
remained stable since 2011.21 Therefore, despite
these limitations, the findings of the present
study add to the broader understanding of OHCA
involving older adults.
Conclusion
This study revealed significant differences in the
patient and bystander characteristics and prehospital
interventions among cardiac arrests involving
older adults that occurred in homes, on streets,
and in other public locations. Many older adults
who experienced cardiac arrest in non-residential
locations had a shockable rhythm in the early period
after receipt of EMS call. Early defibrillation, an
independent predictor of survival, was associated
with favourable survival outcomes in older adults.
These findings suggest that bystanders should
provide aggressive resuscitation, including early
defibrillation. Additionally, low rates of shockable
rhythm and significant delays in bystander and
EMS processes were observed within homes. New
interventions (eg, volunteer dispatch via mobile
applications) are needed to overcome unfavourable
factors that affect cardiac arrests occurring within
older adult households. Finally, the overall bystander CPR rate was low, indicating that additional
measures are needed to overcome bystander inertia.
The insights from this study will help to improve
survival outcomes in OHCAs involving older adults.
Author contributions
The author contributed to the concept or design, analysis or interpretation of data, drafting of the manuscript, and critical revision of the manuscript for important intellectual content.
The author had full access to the data, contributed to the
study, approved the final version for publication, and takes
responsibility for its accuracy and integrity.
Conflicts of interest
The author has no conflicts of interest to disclose.
Acknowledgement
The author thanks Dr Ling-pong Leung, Emergency Medicine Unit of The University of Hong Kong, for providing the
original dataset and permitting its use for secondary analysis
in the study. The author also thanks Mr Min Fan and Ms Lujie
Chen, both from Emergency Medicine Unit of The University
of Hong Kong, for their technical support in this study.
Funding/support
This research received no specific grant from any funding in the public, commercial, or not-for-profit sectors.
Ethics approval
This study is a secondary analysis of a historical cohort study which was approved by the Institutional Review Board of The
University of Hong Kong/Hospital Authority Hong Kong West
Cluster (Ref No.: UW 15-599). The requirement for informed
patient consent was waived because of the retrospective study
design. All patient data in the dataset were anonymous.
References
1. Census and Statistics Department, Hong Kong SAR Government. Hong Kong population projections 2020-2069. Available from: https://www.censtatd.gov.hk/hkstat/sub/sp190.jsp?productCode=B1120015. Accessed 7 Nov 2020.
2. Census and Statistics Department, Hong Kong SAR Government. The profile of Hong Kong population analysed by District Council district, 2018. Table 2. Proportion of land-based non-institutional population by District Council district and age group, 2017. Available from: https://www.censtatd.gov.hk/en/data/stat_report/
product/FA100096/att/B71807FB2018XXXXB0100.pdf. Accessed 24 Mar 2020.
3. Census and Statistics Department, Hong Kong SAR Government. 2016 Population By-census Office. Main tables (demographic). Population density by District Council district and year. 2017. Available from: https://www.bycensus2016.gov.hk/en/bc-mt.html?search=A202. Accessed 24 Mar 2020.
4. Leung LP, Wong TW, Tong HK, Lo CB, Kan PG. Out-of-hospital cardiac arrest in Hong Kong. Prehosp Emerg Care 2001;5:308-11. Crossref
5. Fan KL, Leung LP, Siu YC. Out-of-hospital cardiac arrest in Hong Kong: a territory-wide study. Hong Kong Med J 2017;23:48-53. Crossref
6. Census and Statistics Department, Hong Kong SAR Government. 2016 Population By-census. Domestic households in Hong Kong. Available from: https://www.bycensus2016.gov.hk/en/Snapshot-04.html. Accessed 24 Mar 2020.
7. Census and Statistics Department, Hong Kong SAR Government. 2011 Hong Kong Population Census. Census results. Available from: https://www.censtatd.gov.hk/en/scode170.html. Accessed 17 Mar 2023.
8. Perkins GD, Jacobs IG, Nadkarni VM, et al. Cardiac arrest
and cardiopulmonary resuscitation outcome reports:
update of the Utstein Resuscitation Registry Templates for
Out-of-Hospital Cardiac Arrest: a statement for healthcare
professionals from a task force of the International Liaison
Committee on Resuscitation (American Heart Association,
European Resuscitation Council, Australian and New
Zealand Council on Resuscitation, Heart and Stroke
Foundation of Canada, InterAmerican Heart Foundation,
Resuscitation Council of Southern Africa, Resuscitation
Council of Asia); and the American Heart Association
Emergency Cardiovascular Care Committee and the
Council on Cardiopulmonary, Critical Care, Perioperative
and Resuscitation. Circulation 2015;132:1286-300. Crossref
9. Okabayashi S, Matsuyama T, Kitamura T, et al. Outcomes
of patients 65 years or older after out-of-hospital cardiac
arrest based on location of cardiac arrest in Japan. JAMA
Netw Open 2019;2:e191011. Crossref
10. Dami F, Carron PN, Praz L, Fuchs V, Yersin B. Why bystanders decline telephone cardiac resuscitation advice.
Acad Emerg Med 2010;17:1012-5. Crossref
11. Kiyohara K, Nishiyama C, Matsuyama T, et al. Out-of-hospital cardiac arrest at home in Japan. Am J Cardiol
2019;123:1060-8. Crossref
12. Ringh M, Rosenqvist M, Hollenberg J, et al. Mobile-phone dispatch of laypersons for CPR in out-of-hospital cardiac arrest. N Engl J Med 2015;372:2316-25. Crossref
13. Smith CM, Wilson MH, Ghorbangholi A, et al. The use of trained volunteers in the response to out-of-hospital
cardiac arrest—the GoodSAM experience. Resuscitation 2017;121:123-6. Crossref
14. Mao DR, Ong ME. High-rise residential resuscitation: scaling the challenge. CMAJ 2016;188:399-400. Crossref
15. Coons SJ, Guy MC. Performing bystander CPR for sudden cardiac arrest: behavioral intentions among the general adult population in Arizona. Resuscitation 2009;80:334-40. Crossref
16. Fan KL, Leung LP, Poon HT, Chiu HY, Liu HL, Tang WY. Public knowledge of how to use an automatic external
defibrillator in out-of-hospital cardiac arrest in Hong
Kong. Hong Kong Med J 2016;22:582-8. Crossref
17. Resuscitation Council UK. Cardiopulmonary resuscitation,
automated defibrillators and the law. 2018. Available from:
https://www.resus.org.uk/sites/default/files/2020-05/CPR%20AEDs%20and%20the%20law%20%285%29.pdf. Accessed 24 Mar 2020. Crossref
18. Sayre MR, Barnard LM, Counts CR, et al. Prevalence of COVID-19 in out-of-hospital cardiac arrest: implications
for bystander cardiopulmonary resuscitation. Circulation
2020;142:507-9. Crossref
19. Wong TW, Yeung KC. Out-of-hospital cardiac arrest: two and a half years experience of an accident and emergency department in Hong Kong. J Accid Emerg Med 1995;12:34-9. Crossref
20. Lau CL, Lai JC, Hung CY, Kam CW. Outcome of out-of-hospital
cardiac arrest in a regional hospital in Hong Kong.
Hong Kong J Emerg Med 2005;12:224-7. Crossref
21. Oving I, de Graaf C, Karlsson L, et al. Occurrence of
shockable rhythm in out-of-hospital cardiac arrest over
time: a report from the COSTA group. Resuscitation
2020;151:67-74. Crossref
22. Kitamura T, Kiyohara K, Sakai T, et al. Public-access defibrillation and out-of-hospital cardiac arrest in Japan. N Engl J Med 2016;375:1649-59. Crossref
23. Fan M, Fan KL, Leung LP. Walking route–based calculation
is recommended for optimizing deployment of publicly
accessible defibrillators in urban cities. J Am Heart Assoc
2020;9:e014398 Crossref
24. Agerskov M, Nielsen AM, Hansen CM, et al. Public access defibrillation: great benefit and potential but infrequently used. Resuscitation 2015;96:53-8. Crossref
25. Silverman RA, Galea S, Blaney S, et al. The “vertical response time”: barriers to ambulance response in an
urban area. Acad Emerg Med 2007;14:772-8. Crossref
26. Drennan IR, Strum RP, Byers A, et al. Out-of-hospital cardiac arrest in high-rise buildings: delays to patient care and effect on survival. CMAJ 2016;188:413-9. Crossref
27. Moore JC, Segal N, Debaty G, Lurie KG. The “do’s and don’ts” of head up CPR: lessons learned from the animal
laboratory. Resuscitation 2018;129:e6-e7. Crossref
28. Winther-Jensen M, Kjaergaard J, Hassager C, et al. Resuscitation and post resuscitation care of the very old after out-of-hospital cardiac arrest is worthwhile. Int J
Cardiol 2015;201:616-23. Crossref