Hong Kong Med J 2023 Apr;29(2):132–41 | Epub 14 Apr 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
The real-world impact of the COVID-19 pandemic on patients with cancer: a multidisciplinary cross-sectional survey
Kelvin KH Bao, MB BChir, FRCR; Ka-man Cheung, MB, ChB, FRCR; James CH Chow, MB, ChB, FRCR; Carmen WL Leung, MB, ChB, FRCR; Kam-hung Wong, MB, ChB, FRCR
Department of Clinical Oncology, Queen Elizabeth Hospital, Hong Kong SAR, China
Corresponding author: Dr Kelvin KH Bao (bkh641@ha.org.hk)
Abstract
Introduction: The coronavirus disease 2019
(COVID-19) pandemic has caused unprecedented
disruptions to cancer care worldwide. We conducted
a multidisciplinary survey of the real-world impact of
the pandemic, as perceived by patients with cancer.
Methods: A total of 424 patients with cancer were
surveyed using a 64-item questionnaire constructed
by a multidisciplinary panel. The questionnaire
examined patient perspectives regarding COVID-19–related effects (eg, social distancing measures)
on cancer care delivery, resources, and healthcare-seeking
behaviour, along with the physical and
psychosocial aspects of patient well-being and
pandemic-related psychological repercussions.
Results: Overall, 82.8% of respondents believed
that patients with cancer are more susceptible to
COVID-19; 65.6% expected that COVID-19 would
delay anti-cancer drug development. Although only
30.9% of respondents felt that hospital attendance
was safe, 73.1% expressed unaltered willingness
to attend scheduled appointments; 70.3% of
respondents preferred to receive chemotherapy
as planned, and 46.5% were willing to accept
changes in efficacy or side-effect profile to allow
an outpatient regimen. A survey of oncologists
revealed significant underestimation of patient motivation to avoid treatment interruptions. Most
surveyed patients felt that there was an insufficient
amount of information available concerning the
impact of COVID-19 on cancer care, and most
patients reported social distancing–related declines
in physical, psychological, and dietary wellness. Sex,
age, education level, socio-economic status, and
psychological risk were significantly associated with
patient perceptions and preferences.
Conclusion: This multidisciplinary survey concerning the effects of the COVID-19 pandemic
revealed key patient care priorities and unmet needs.
These findings should be considered when delivering
cancer care during and after the pandemic.
New knowledge added by this study
- Most patients with cancer (73.1%) reported that their willingness to attend scheduled oncology appointments was not affected by the pandemic. All surveyed oncologists underestimated patient motivation to avoid treatment interruptions.
- Patient acceptance of telerehabilitation varied according to age and socio-economic status, whereas the negative impact of social distancing on patients with cancer were substantial and multidimensional.
- Psychometric analyses can stratify patients with cancer into psychological risk groups, based on their distinct perceptions of the pandemic.
- These findings will help to increase awareness of the effects of the coronavirus disease 2019 pandemic on patients with cancer, revealing their priorities and unmet needs.
- This work aligns the expectations of oncologists and patients with cancer with respect to modifications of cancer services during the pandemic.
- These results will promote better resource allocation and earlier multidisciplinary interventions to reduce pandemic-related impact on at-risk populations.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic
poses an unprecedented threat to health systems
worldwide. During the first year of the pandemic, there were more than 110 million confirmed
COVID-19 cases globally and more than 2.6 million
deaths.1 In terms of scale, the number of COVID-19
cases during that period was at least sixfold more than the global number of new cancer cases in 2018; the
mortality during that period exceeded the combined
mortalities of lung cancer and breast cancer in
2018.2 The many consequences of COVID-19 have
included unprecedented disruptions to cancer
care services,3 4 5 such as cancellations of outpatient
appointments to delays in scheduled systemic
treatments and radiotherapy; during periods of
increased transmission, such disruptions have forced
oncologists to make difficult decisions in attempts to
balance patient protection and disease control. There
have been similar impact to the delivery of oncology-related
allied health services, including physical
therapy and occupational therapy,6 dietetics,7
diagnostic imaging,8 and psychological services for patients with cancer9; there has been a particularly large shift in the use of telemedicine. Throughout the COVID-19 pandemic, and particularly
during periods of increased transmission, good
multidisciplinary coordination has been a crucial
aspect of cancer care. By acquiring comprehensive
knowledge regarding perceptions of the pandemic,
changes in healthcare-seeking behaviour, impact
on daily life, and the newly emerged unmet needs
(physical, socio-economic, and psychological)
of patients with cancer, multidisciplinary cancer
caregivers can customise and adjust their services
accordingly, thus enabling appropriate resource
allocation. Considering these challenges, we
designed and conducted a prospective study to comprehensively examine the real-world impact of
COVID-19 on patients with cancer; we sought to
identify actionable solutions from the perspective of
experienced multidisciplinary cancer caregivers.
Methods
A prospective survey regarding the perspectives
of patients with cancer on the impact of the
COVID-19 pandemic was jointly developed by
a multidisciplinary team at Queen Elizabeth
Hospital, Hong Kong that consisted of clinical
oncologists, clinical psychologists, physiotherapists,
occupational therapists, and dieticians specialising
in cancer care. A pilot survey was administered
to 88 patients, followed by interviews to further
assess patient understanding of the questions
and to develop additional items via thematic
analysis. The multidisciplinary team then refined
the questionnaire. The final version consisted of
64 items with a combination of Likert scales and
polar questions; it covered topics such as patient
perceptions of cancer care resources, treatment
delivery and quality, changes in healthcare-seeking
behaviour, adequacy of available pandemic-related
information, social distancing–related adverse
impact, and psychological repercussions of the
pandemic. We also invited patients who were newly
diagnosed with cancer to complete an extended
questionnaire which focused on psychometric
measurements of post-traumatic stress disorder
(PTSD) [the PTSD Checklist for DSM-5 (PCL-5)],10 anxiety and depression (the Emotion Thermometers
tool),11 and intolerance of uncertainty (the Intolerance of Uncertainty Scale-12 [IUS-12]).12 Patients were then stratified into risk groups. High-risk
individuals had scores of ≥5 on the abbreviated
PCL-5 scale,13 ≥3 on the Emotion Thermometers for depression or anxiety,14 and ≥25 on the IUS-12
scale.11 Associations between patient perceptions
and psychological risk were then explored. Full
details of the patient questionnaire are shown in
online supplementary Table 1.
Furthermore, we surveyed clinical oncologists
in Hong Kong (practising in Queen Elizabeth
Hospital, United Christian Hospital, and Buddhist
Hospital) regarding their perceptions of the
pandemic; the oncologists were also asked to predict
the responses of patients with cancer in various
domains of interest.
The patient survey was conducted between
12 and 22 May 2020 at Queen Elizabeth Hospital.
Patients with cancer and survivors aged ≥18 years
who attended their outpatient oncology appointments
were invited to participate. Patients who could
not read English or Chinese were excluded, and
participation was voluntary. Detailed survey
information was provided on the questionnaire
cover sheet, and a patient’s decision to participate in the survey was regarded as informed consent.
Hardcopies of the questionnaire were anonymously
completed by participants on site, then collected by
dedicated nursing staff.
Data analysis
Descriptive analysis was used to describe various
impact of the pandemic on patients. Patient
demographics, disease characteristics, treatment
details, and socio-economic information were
summarised. Qualitative data are presented as the
percentage of respondents who selected a particular
response. Chi squared tests were used to determine
associations between responses and categorical
patient factors. P values <0.05 were considered
indicative of statistical significance. Analyses were
performed using SPSS software (Windows version
25.0; IBM Corp, Armonk [NY], United States).
Results
Demographic characteristics
Between 12 and 22 May 2020, 650 patients with
cancer were invited to participate in the survey; 424
responses were received, yielding a response rate of
65.2%. Demographic and clinical characteristics of
the participants are presented in the Table. Most
survey respondents were female (70.0%), and more
than half were aged 46 to 75 years. Nearly half (46.0%)
of the respondents were receiving active cancer
treatment. The cancer stage was III or below in half
of the respondents and 20.3% of respondents were
at stage IV; 29.2% of respondents were uncertain of
their staging. Almost half (43.9%) of the respondents
had a monthly family income of <HK$16 000 (around
US$2000), which is Hong Kong’s 2018 poverty line
for a family of three.15
Impact of coronavirus disease 2019 on cancer
resources
As shown in online supplementary Table 1, most
respondents (82.8%) believed that patients with
cancer are more susceptible to COVID-19, while
more than half (52.1%) believed that cancer-related
resources will be depleted and 59.3% were
concerned that healthcare workforce shortages
during the pandemic would harm their treatment.
Overall, 65.6% of respondents were concerned that
COVID-19 would lead to delays in anti-cancer drug
development. These concerns were significantly
associated with education level of patients, in which
the more educated respondents demonstrated less
concern (tertiary level 57.6% vs secondary 64.4% vs
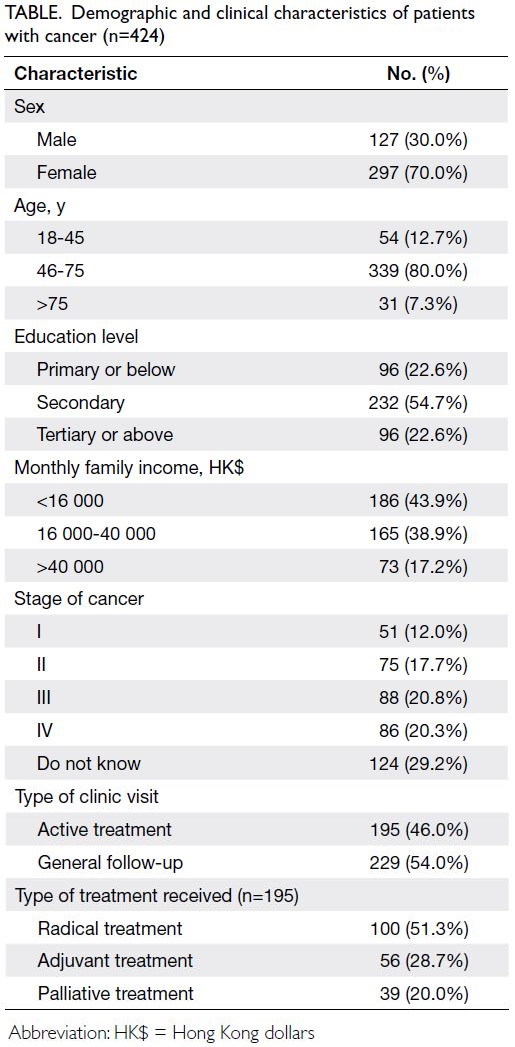
primary 71.4%, P=0.01) [Fig 1a].
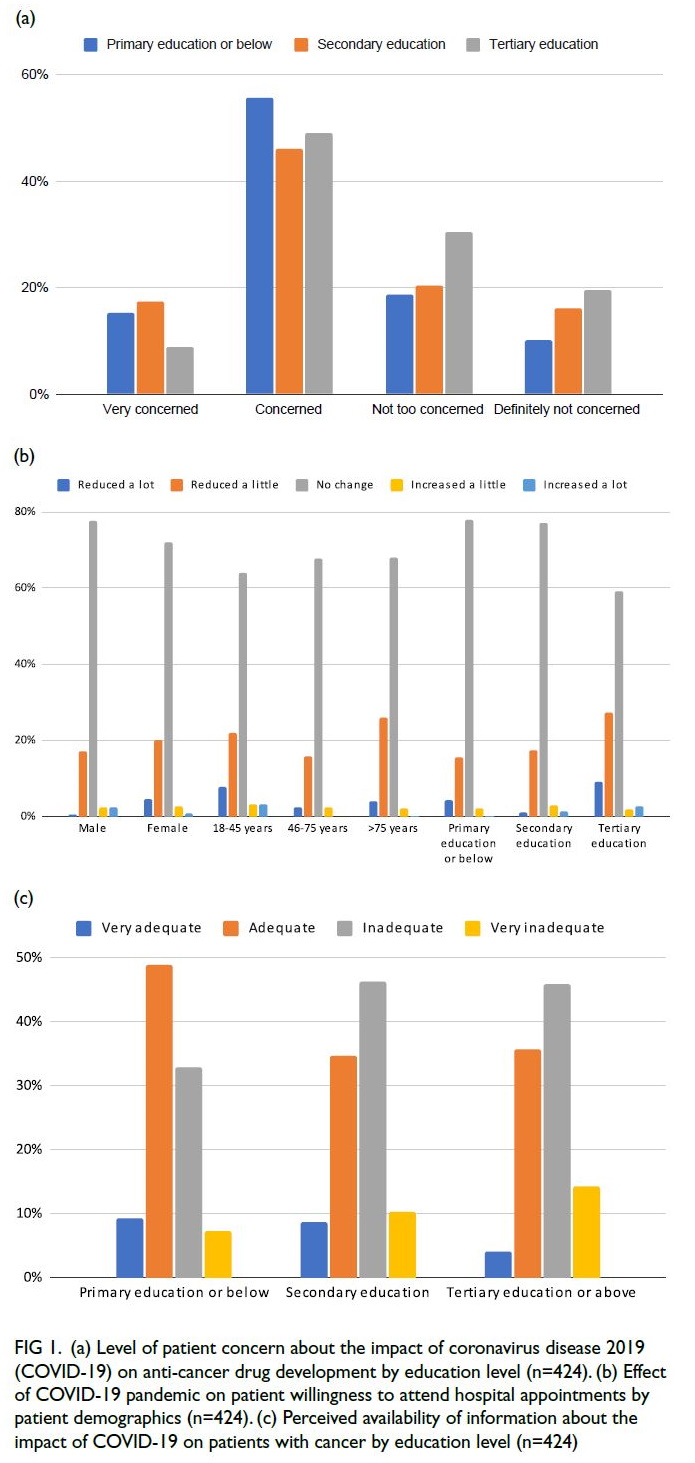
Figure 1. (a) Level of patient concern about the impact of coronavirus disease 2019 (COVID-19) on anti-cancer drug development by education level (n=424). (b) Effect of COVID-19 pandemic on patient willingness to attend hospital appointments by patient demographics (n=424). (c) Perceived availability of information about the impact of COVID-19 on patients with cancer by education level (n=424)
Impact of coronavirus disease 2019 on
healthcare-seeking behaviour
As shown in online supplementary Table 1, fewer than one-third of respondents (30.9%) felt that it
was safe to attend hospital appointments during the
pandemic (the proportion was greater among men
than among women: 37.8% vs 27.8%). Furthermore,
most respondents reported that their willingness
to attend oncology clinic appointments (73.1%)
or undergo clinical tests (80.2%) was unaffected.
Age (P=0.021), sex (P=0.029), and education level
(P=0.003) were factors significantly associated with
patient willingness; respondents aged 18-45 years
or >75 years, female, and more educated individuals
were more hesitant to attend their scheduled
appointments (Fig 1b).
Compared with the pre-pandemic period,
most respondents (79.0%) stated that they were
equally willing (65.1%) or more willing (13.9%)
to seek medical attention now if they felt unwell.
Overall, 62.2% of respondents were equally willing or more willing to be hospitalised if requested by their
oncologists. Male respondents were more willing to
be hospitalised, compared with female respondents
(68.3% vs 59.2%); additionally, respondents
receiving radical treatment were more willing to be
hospitalised, compared with respondents receiving
palliative treatment (71.3% vs 59.0%).
Effects of social distancing on medical
consultation and cancer treatment
Nearly all respondents (98.4%) felt that it was
acceptable for medical staff to maintain an increased
physical distance from patients during consultations,
and most (83.3%) felt that it did not negatively
impact the quality of their clinic experience. During
the pandemic, some clinically stable patients
were exempt from the requirement for oncologist
examination prior to medication refills. Overall,
59.9% of respondents felt that such an arrangement
should continue beyond the pandemic period
(male respondents vs female respondents: 69.3% vs
55.9%; respondents receiving radical treatment vs
respondents receiving palliative treatment: 54.4% vs
69.2%).
Concerning the effects of the pandemic on
plans for cancer treatment, most respondents stated
that their decisions to receive chemotherapy (70.3%)
or radiotherapy (67.9%) were unaffected. However,
46.5% of the respondents were willing to accept
changes in treatment efficacy or side-effect profile
to allow an outpatient regimen; this preference was
particularly strong among respondents receiving
palliative treatment (61.5%), compared with
respondents receiving radical treatment (33.7%).
Acquisition and adequacy of pandemic-related
information
As shown in online supplementary Table 1, half of
the respondents (49.1%) spent an average of 10 to 30
minutes daily interacting with news and information
sources focused on COVID-19. Their most common
news sources were television (41.7%), the internet
(28.0%), and newspapers (12.9%). Only 3.5% of
respondents received pandemic-related news or
information from their hospitals. Young respondents
(<45 years) were significantly more likely to receive
news primarily from the internet, compared with
older respondents (>75 years) (37.6% vs 13.4%;
P=0.001); such a difference was also present between
respondents with different education levels (tertiary
education vs primary education: 35.5% vs 17.4%;
P=0.001) and between respondents with different
levels of monthly family income (>HK$40 000 vs
<HK$16 000: 32% vs 25%; P=0.006).
Concerning the adequacy of information
received regarding COVID-19 and its impact
on patients with cancer, more than half of the respondents (54.1%) felt that it was inadequate; this
sentiment was more prevalent among respondents
with a higher education level, compared with those
who were less educated (tertiary vs primary level:
60.2% vs 40.3%; P=0.017) [Fig 1c].
Effects of social distancing on allied health
professional services
During the pandemic, social distancing became
the new daily norm. Nearly half of the respondents
(49.5%) reported exercising less, whereas 10.4%
reported exercising more. In general, 55.4% of
respondents noticed an overall deterioration in
their physical well-being (Fig 2a); about one-third
of respondents (32.1%) reporting reduced walking
tolerance, and 25.9% of respondents noticed some
reduction in limb power (online supplementary Table 1).
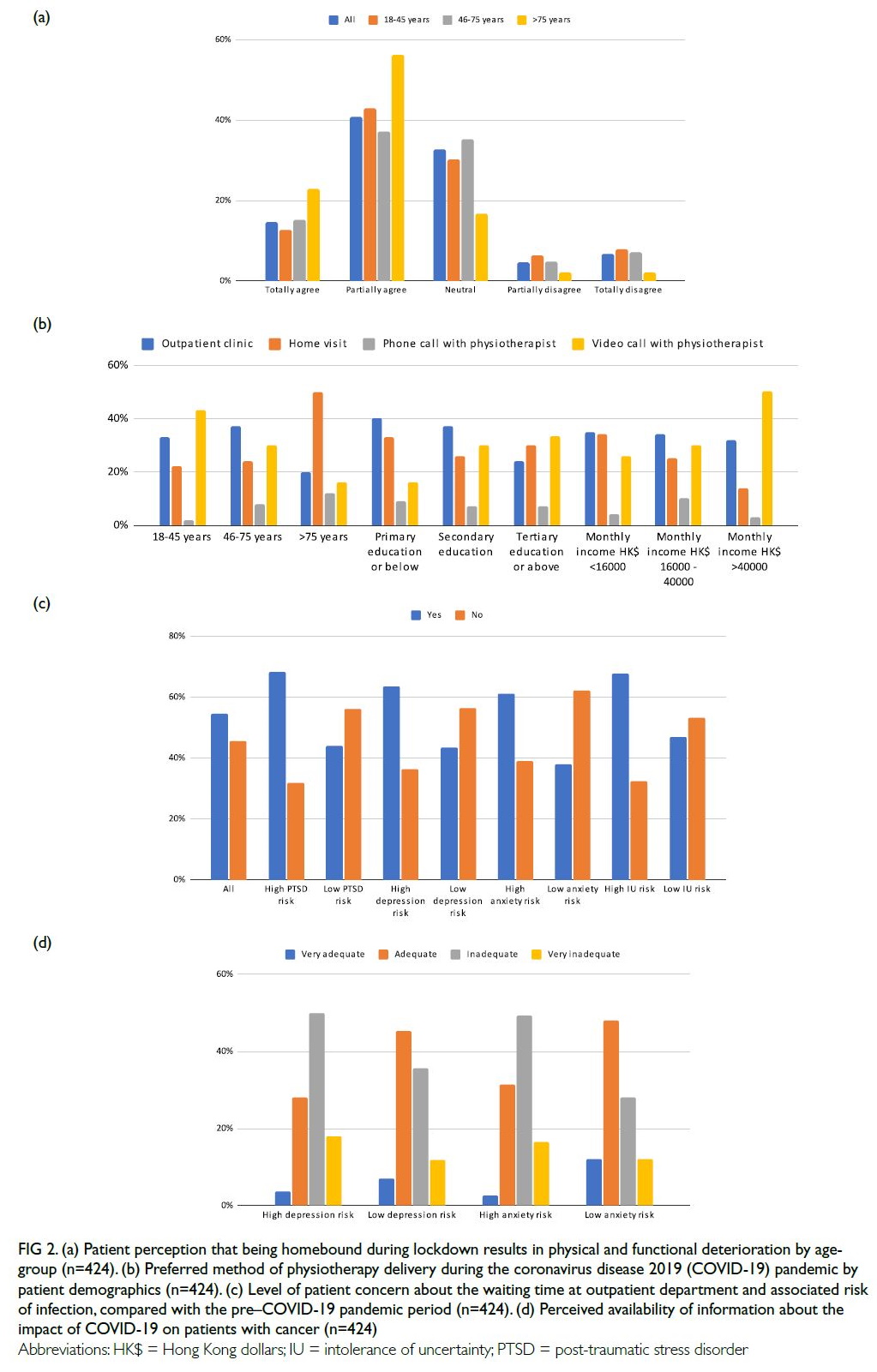
Figure 2. (a) Patient perception that being homebound during lockdown results in physical and functional deterioration by age-group (n=424). (b) Preferred method of physiotherapy delivery during the coronavirus disease 2019 (COVID-19) pandemic by patient demographics (n=424). (c) Level of patient concern about the waiting time at outpatient department and associated risk of infection, compared with the pre–COVID-19 pandemic period (n=424). (d) Perceived availability of information about the impact of COVID-19 on patients with cancer (n=424)
With respect to patient preferences regarding
physiotherapy delivery during the pandemic, 42.9%
of young respondents (18-45 years) preferred online
sessions, whereas 50.0% of older respondents (>75
years) preferred home visits by a therapist [Fig 2b].
Education level (P=0.029) and income (P=0.034)
were significantly associated with patient preference.
Respondents with a higher education level (tertiary
vs primary level: 33.3% vs 16.3%) and respondents
with a higher income (monthly income >HK$40 000
vs <HK$16 000: 50.3% vs 26.0%) preferred online
sessions, rather than in-person sessions.
During the period of social distancing, 64.5%
of older respondents (>75 years) felt that their lives
had become monotonous and lonely; significantly
fewer (39.3%) younger respondents (<45 years)
expressed this sentiment. Most respondents (58.0%)
agreed that their home care support had improved
because family members spent more time together;
this sentiment was more prevalent among older
respondents (>75 years) [70.9%].
As shown in online supplementary Table 1,
the pandemic caused dietary habit alterations in
38.9% of respondents. Approximately one-fifth of
respondents reported reduced appetite (22.2%) and
increased consumption of junk food (processed
or ready-made meals) (19.3%). Significantly more
respondents in the low-income subgroup reported
reduced appetite, compared with respondents in
the high-income subgroup (30.6% vs 8.2%, P=0.001).
Notably, the use of face masks led to a reduction in
meal frequency among 30.7% of respondents; this
reduction was more prevalent among respondents
with lower income, compared with respondents who
had higher income (32.6% vs 23.2%).
Psychological impact of coronavirus disease
2019
Overall, 41.0% and 23.1% of respondents had recently experienced anxiety and/or depressed mood. In total,
103 consecutive newly diagnosed patients responded
to the extended psychometric questionnaire. The
results revealed greater levels of concern regarding
the impact of COVID-19 on cancer care manpower
and the risk of infection during outpatient clinic
waiting time in patients with higher risks of PTSD
(P=0.011 and P=0.015, respectively), anxiety
(P=0.013 and P=0.034, respectively), depression
(P=0.017 and P=0.043, respectively), and uncertainty
intolerance (P=0.004 and P=0.044, respectively) [Fig 2c]. A high IUS-12 score (uncertainty intolerance)
was associated with the presence of greater concern
regarding the effects of the pandemic on cancer
research and drug development (P=0.03). As shown
in online supplementary Table 2, respondents with
a high risk of anxiety were less likely to agree with
the ‘no visiting’ policy of hospitals (P=0.013). More
respondents with high risks of anxiety (P=0.024)
and depression (P=0.044) felt that there was an
insufficient amount of information available in the
media regarding the impact of COVID-19 on patients
with cancer (Fig 2d). Moreover, respondents with a
high risk of PTSD demonstrated significantly greater
concern when asked about their fear of being infected
by their caregiver or family members, compared with
respondents who had a low risk of PTSD (P=0.005).
Detailed results of the psychometric questionnaire
are shown in online supplementary Table 2.
Comparison of oncologist and patient
perspectives
We invited 30 practising clinical oncologists to predict patient healthcare-seeking behaviour during the
pandemic. All 21 responding oncologists predicted
significant reductions in patient willingness to
attend appointments and patient willingness to be
hospitalised, but most patients reported no change
in either type of willingness (73.3% and 54.7%,
respectively). A greater proportion of oncologists
(50.0%) than patients (16.7%) reported a negative
impact on their clinic experience because of doctor-patient
distancing measures (Fig 3a). Furthermore,
when asked about their confidence in identifying the
cause of a new fever (COVID-19–related vs other
causes), most oncologists reported little (73.3%) or
no confidence (13.3%), whereas almost half of the
patients (47.4%) reported that they were quite or
very confident in their ability to identify the cause of
a new fever (Fig 3b).
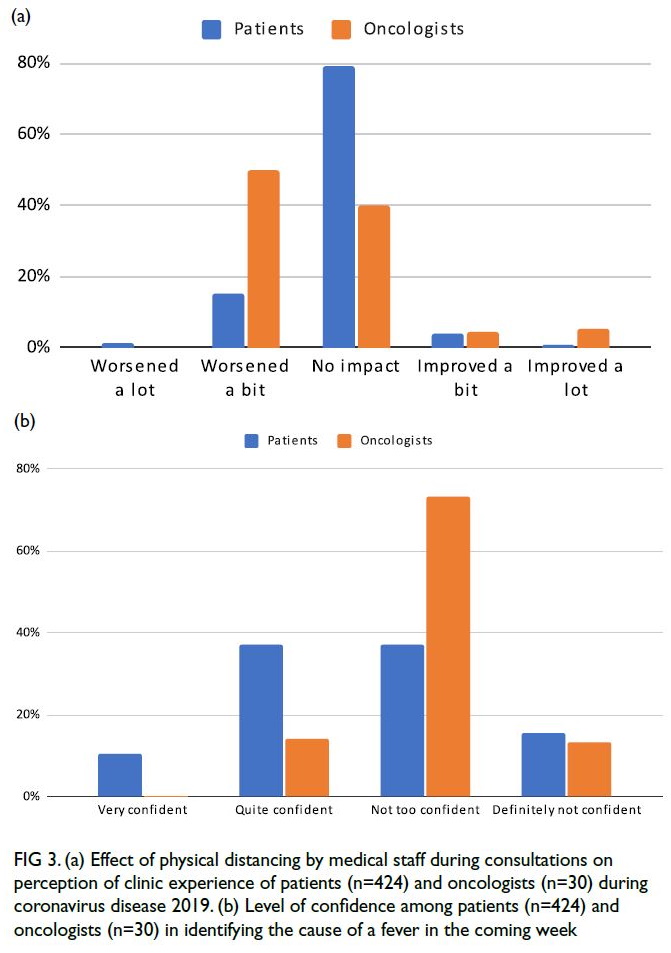
Figure 3. (a) Effect of physical distancing by medical staff during consultations on perception of clinic experience of patients (n=424) and oncologists (n=30) during coronavirus disease 2019. (b) Level of confidence among patients (n=424) and oncologists (n=30) in identifying the cause of a fever in the coming week
Discussion
This study investigated the perceptions of patients
with cancer regarding the real-world impact of
COVID-19 (during the early days of the pandemic)
through the perspective of a multidisciplinary
team that included clinical oncologists, clinical psychologists, physiotherapists, dieticians, and
occupational therapists. Using a comprehensive
set of questions, we identified key concerns, unmet
needs, perceptions, and expectations of patients
with cancer at different stages in their cancer care
journeys. Cancer care16 and pandemic management17
are both resource-intensive endeavours. Because
the COVID-19 pandemic has become the focus
of healthcare worldwide, it is understandable
that patients with cancer are concerned about
pandemic-related negative impact on cancer care
resources. Our results suggest that patients with
cancer remained committed to attending scheduled
appointments, despite the perceived risk of
COVID-19 during the early days of the pandemic.
This sustained clinical demand—along with general
acceptance among patients regarding COVID-19
adaptive measures (staff-patient distancing),
streamlined services (prescription-only clinics),
and outcome trade-offs (efficacy and side-effect
profile)—allowed our oncology services to continue
with minimal disruptions despite the reduced
availability of healthcare resources. Nevertheless,
only 30.9% of surveyed patients felt that it was safe
to attend the hospital; this observation highlights the
need to ensure patients are informed about hospital
safety measures for COVID-19 management,
with details regarding rationale and efficacy. This
study also revealed a discrepancy between male
and female patients in terms of healthcare-seeking
behaviour; moreover, patients receiving radical
treatment demonstrated different perceptions and
needs, compared with patients receiving palliative
care. Oncology healthcare providers should consider
the unique needs of various patient groups when
implementing pandemic management strategies.
Between the initial outbreak and the time of
this survey, the general public’s understanding of
COVID-19 heavily relied on mainstream media
coverage,18 which often did not focus on the needs
of specific patient groups. International guidelines
regarding cancer management during the pandemic
began to emerge later in 2020,19 but they mainly targeted medical professionals. Accordingly,
patients with cancer felt that the COVID-19–related
information provided to patients was inadequate.
This perception was particularly prevalent among
patients with a higher education level, who tended to
obtain news and information more frequently from
multiple sources (eg, the internet and social media).
Notably, this situation highlights the phenomenon
of ‘the more you know, the more you realise you
don’t know’, thereby emphasising the presence of an
additional information barrier for underprivileged
patient groups.20 The situation is further
complicated by the presence of COVID-19–related
misinformation, which has been widespread on
social media since 2020.21 The findings in this study provide insights concerning the distinct pandemic-related
information preferences and needs among
patients according to age, education level, and
income. Cancer services should focus on addressing
these preferences and needs by providing patients
with current COVID-19–related information from
official sources, ensuring that the hospital remains
a source of verified and practical pandemic-related
information accessible to all patients.
The consequences of social distancing (eg,
reduced exercise, poor diet, increased financial
burden, and loss of social interactions) are
detrimental to the physical and psychological well-being
of patients with cancer,22 23 24 potentially reducing
cancer treatment tolerance and compromising
outcomes. Although the impact of pandemic-related
lockdowns on dietary patterns of diabetic patients25 and older population26 have been studied,
there are limited prospective data regarding the
nutritional status of patients with cancer and their
needs during the pandemic. This study has revealed
some real-world patient needs, particularly among
socio-economically disadvantaged patients; it also
highlights the importance of individualised dietetic
and occupational health assessments and early
interventions (inpatient or outpatient) by dieticians
and occupational therapists who specialise in cancer
care. Dedicated self-help materials prepared by
allied health professionals to address the adverse
effects of social distancing may also serve as effective
resources.
When the pandemic began, telerehabilitation
emerged as a promising alternative method for
patient–clinician interactions, with effective use in
a physiotherapy context.27 28 However, our findings
indicate that telerehabilitation may not be universally
welcomed, particularly among older patients. Turolla
et al29 described the challenges of implementing
telerehabilitation; our findings highlight the need
to carefully examine telemedicine accessibility and
‘telehealth literacy’30 among socio-economically underprivileged populations.31 32 When possible,
conventional physiotherapy and rehabilitation
should remain available, particularly for older
adults, less-educated individuals, and low-income
patients.33 Our findings offer a rationale for triaging
appropriate patients towards telemedicine; they
also highlight the need for improving telemedicine
quality and access, as well as the importance of
ensuring that alternatives are available.
This study demonstrated that psychometric
analysis is a meaningful tool for identifying at-risk
populations of patients with cancer during the
pandemic. Patients in psychological high-risk
groups clearly demonstrated distinct perceptions,
expectations, and needs when simultaneously
confronted with a cancer diagnosis and the
COVID-19 pandemic. Without effective
management, such patients could experience long-lasting
psychiatric morbidities, as revealed during
the severe acute respiratory syndrome epidemic in
2003.34 35 Wang et al36 emphasised the importance
of mental healthcare attention and resources
for patients with cancer during the COVID-19
pandemic. Along with routine cancer care, targeted
psychotherapies and follow-up care for both the
acute impact and long-term sequelae of COVID-19
are needed.
Oncologists and patients with cancer have
different perceptions of cancer symptoms, treatment
priorities, and psychosocial needs.37 38 39 We found
that oncologists tended to underestimate patient
motivation to avoid treatment interruptions, as
well as patient risk acceptance, consistent with the
observation by Catania et al40 that patients with cancer were more concerned about their cancers
than about the pandemic. Moreover, compared with
oncologists, a greater proportion of our surveyed
patients expressed confidence in identifying
COVID-19 symptoms. These results illustrate
differences in priorities and perceptions of pandemic
severity, along with the challenge of balancing
disruptions to cancer treatment and maintaining
COVID-19–related safety.
Proposed interventions to minimise the impact of coronavirus disease 2019 on cancer patients
The following are some proposed interventions
to minimise the impact of COVID-19 on cancer patients:
1. Ensure that patients are informed about hospital safety measures for COVID-19 management, with details regarding rationale and efficacy.
2. Ensure that healthcare staff maintain appropriate physical distance from patients.
3. Operate prescription-only clinics and lengthen follow-up intervals for clinically stable patients.
4. Triage appropriate patients towards telemedicine; enhance general telehealth literacy by implementing user-friendly interfaces, step-by-step demonstrations, and support hotlines.
5. Establish a regularly updated COVID-19–related newsfeed that is customised for patients with cancer.
6. Work with dieticians, physiotherapists, and occupational therapists to create self-help pamphlets that can guide patients with cancer in coping with the effects of social distancing; facilitate the establishment of virtual support groups for patients with cancer.
7. Implement early allied health assessments and interventions for at-risk patients.
8. Ensure early psychological support, particularly for newly diagnosed patients.
9. Compassionately and flexibly enforce restrictive measures for newly diagnosed patients, individuals approaching the end of life, and selected at-risk patients.
10. Periodically review these measures as the pandemic progresses.
1. Ensure that patients are informed about hospital safety measures for COVID-19 management, with details regarding rationale and efficacy.
2. Ensure that healthcare staff maintain appropriate physical distance from patients.
3. Operate prescription-only clinics and lengthen follow-up intervals for clinically stable patients.
4. Triage appropriate patients towards telemedicine; enhance general telehealth literacy by implementing user-friendly interfaces, step-by-step demonstrations, and support hotlines.
5. Establish a regularly updated COVID-19–related newsfeed that is customised for patients with cancer.
6. Work with dieticians, physiotherapists, and occupational therapists to create self-help pamphlets that can guide patients with cancer in coping with the effects of social distancing; facilitate the establishment of virtual support groups for patients with cancer.
7. Implement early allied health assessments and interventions for at-risk patients.
8. Ensure early psychological support, particularly for newly diagnosed patients.
9. Compassionately and flexibly enforce restrictive measures for newly diagnosed patients, individuals approaching the end of life, and selected at-risk patients.
10. Periodically review these measures as the pandemic progresses.
Study strengths and limitations
To our knowledge, this is one of the first studies
to simultaneously explore perceptions of the real-world
impact of the COVID-19 pandemic among
patients with cancer and oncologists. Importantly,
the efforts of the multidisciplinary team to construct
the questions contributed to a multidimensional,
holistic understanding of issues and unmet needs
that affect patients with cancer at different stages of
their cancer care journeys. Because of the in-person
survey invitation and paper-and-pen methodology, our survey achieved a high response rate of 65%,
ensuring that the results are representative of the
surveyed population. However, sampling bias was
present because survey respondents were patients
who physically attended their clinic appointments;
data were missing for around 10% of patients
who declined to attend their clinic appointments.
Furthermore, this survey was conducted within a
short interval (2 weeks) towards the end of the first
wave of the COVID-19 pandemic in Hong Kong,
when there was a gradual easing of lockdown policies
and personal protective equipment availability began
to improve41; thus, this cross-sectional assessment
may not adequately reflect the evolution of patient
perceptions regarding the COVID-19 pandemic.
Other key limitations of the study include its
inclusion of patients from a single cancer centre, as
well as the exclusion of patients who could not read
Chinese or English and patients who underwent
treatment in private clinics. There is a need to repeat
the study at various time points throughout the
pandemic; future analyses should focus on other
affected countries and patient populations.
Conclusion
This multidisciplinary survey concerning the effects
of the COVID-19 pandemic impact revealed key
care priorities among patients with cancer, as well
as their unmet needs; in particular, it highlighted the
importance of distinct priorities and needs among
socio-economically underprivileged groups and
patients with diverse psychological phenotypes.
Oncologists should be aware that their own
perceptions of pandemic-related effects differ from
their patients’ perceptions. These findings should
be carefully considered as multidisciplinary teams
modify their delivery of cancer care services during
and after the pandemic.
Author contributions
Concept or design: KKH Bao, KM Cheung, JCH Chow.
Acquisition of data: All authors.
Analysis or interpretation of data: KKH Bao, KM Cheung, JCH Chow.
Drafting of the manuscript: KKH Bao, KM Cheung, JCH Chow.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: KKH Bao, KM Cheung, JCH Chow.
Drafting of the manuscript: KKH Bao, KM Cheung, JCH Chow.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
We thank all multidisciplinary team members and
participating patients for their efforts and contributions.
Declaration
This research has been presented in part as poster
presentations at the following conferences:
1. ESMO Congress 2020, virtual, 19-21 Sep 2020 (title: Cancer patients’ perspectives on the real-world impact of COVID-19 pandemic: a multidisciplinary survey)
2. ESMO Asia Congress 2020, virtual, 20-22 Nov 2020 (title: Psychometric interplay of the perception of the real-life impact of COVID-19 pandemic: a cross-sectional survey of patients with newly diagnosed malignancies)
1. ESMO Congress 2020, virtual, 19-21 Sep 2020 (title: Cancer patients’ perspectives on the real-world impact of COVID-19 pandemic: a multidisciplinary survey)
2. ESMO Asia Congress 2020, virtual, 20-22 Nov 2020 (title: Psychometric interplay of the perception of the real-life impact of COVID-19 pandemic: a cross-sectional survey of patients with newly diagnosed malignancies)
Funding/support
This research was supported by the Hong Kong Hospital
Authority Kowloon Central Cluster Research Grant 2020 (Ref No.: KCC/RC/G/2021-B01).
Ethics approval
The study was approved by the Kowloon Central/Kowloon
East Cluster Clinical Research Ethics Committee of Hospital
Authority, Hong Kong (Ref No.: KC/KE-20-0126/ER-1). All
eligible respondents explicitly agreed to join the panel and
provided informed consent to participate in the study.
References
1. World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. Available from: https://covid19.who.int. Accessed 7 Nov 2020.
2. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN
estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. Crossref
3. Jazieh AR, Akbulut H, Curigliano G, et al. Impact of the COVID-19 pandemic on cancer care: a global collaborative
study. JCO Glob Oncol 2020;6:1428-38. Crossref
4. Chen-See S. Disruption of cancer care in Canada during COVID-19. Lancet Oncol 2020;21:e374. Crossref
5. Sud A, Torr B, Jones ME, et al. Effect of delays in the
2-week-wait cancer referral pathway during the COVID-19
pandemic on cancer survival in the UK: a modelling study.
Lancet Oncol 2020;21:1035-44. Crossref
6. Prvu Bettger J, Thoumi A, Marquevich V, et al. COVID-19: maintaining essential rehabilitation services across the
care continuum. BMJ Glob Health 2020;5:e002670. Crossref
7. Thibault R, Coëffier M, Joly F, Bohé J, Schneider SM, Déchelotte P. How the Covid-19 epidemic is challenging
our practice in clinical nutrition—feedback from the field.
Eur J Clin Nutr 2021;75:407-16. Crossref
8. Maringe C, Spicer J, Morris M, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in
diagnosis in England, UK: a national, population-based,
modelling study. Lancet Oncol 2020;21:1023-34. Crossref
9. Liu S, Yang L, Zhang C, et al. Online mental health services in China during the COVID-19 outbreak. Lancet
Psychiatry 2020;7:e17-8. Crossref
10. Price M, Szafranski DD, van Stolk-Cooke K, Gros DF. Investigation of abbreviated 4 and 8 item versions of the
PTSD Checklist 5. Psychiatry Res 2016;239:124-30. Crossref
11. Beck KR, Tan SM, Lum SS, Lim LE, Krishna LK. Validation of the emotion thermometers and hospital anxiety and
depression scales in Singapore: screening cancer patients
for distress, anxiety and depression. Asia Pac J Clin Oncol 2016;12:e241-9. Crossref
12. Carleton RN, Norton MA, Asmundson GJ. Fearing the unknown: a short version of the Intolerance of Uncertainty
Scale. J Anxiety Disord 2007;21:105-17. Crossref
13. Geier TJ, Hunt JC, Hanson JL, et al. Validation of abbreviated four- and eight-item versions of the PTSD
checklist for DSM-5 in a traumatically injured sample. J
Trauma Stress 2020;33:218-26. Crossref
14. Schubart JR, Mitchell AJ, Dietrich L, Gusani NJ. Accuracy of the Emotion Thermometers (ET) screening tool in patients undergoing surgery for upper gastrointestinal malignancies. J Psychosoc Oncol 2015;33:1-14. Crossref
15. Office of the Government Economist Financial Secretary’s
Office. Census and Statistics Department. Hong Kong SAR Government. Hong Kong Poverty Situation Report 2018.
Available from: https://www.povertyrelief.gov.hk/eng/pdf/Hong_Kong_Poverty_Situation_Report_2018(2019.12.13).pdf. Accessed 17 Mar 2023.
16. Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States:
2010-2020. J Natl Cancer Inst 2011;103:117-28. Crossref
17. Tan-Torres Edejer T, Hanssen O, Mirelman A, et al. Projected health-care resource needs for an effective response to COVID-19 in 73 low-income and middle-income countries: a modelling study. Lancet Glob Health 2020;8:e1372-9. Crossref
18. Casero-Ripollés A. Impact of Covid-19 on the media system. Communicative and democratic consequences of
news consumption during the outbreak. El profesional de
la información 2020;29:e290223. Crossref
19. Curigliano G, Banerjee S, Cervantes A, et al. Managing cancer patients during the COVID-19 pandemic: an
ESMO multidisciplinary expert consensus. Ann Oncol
2020;31:1320-35. Crossref
20. Matsuyama RK, Wilson-Genderson M, Kuhn L, Moghanaki D, Vachhani H, Paasche-Orlow M. Education
level, not health literacy, associated with information needs
for patients with cancer. Patient Educ Couns 2011;85:e229-36. Crossref
21. Pennycook G, McPhetres J, Zhang Y, Lu JG, Rand DG. Fighting COVID-19 misinformation on social media:
experimental evidence for a scalable accuracy-nudge
intervention. Psychol Sci 2020;31:770-80. Crossref
22. Di Corrado D, Magnano P, Muzii B, et al. Effects of social distancing on psychological state and physical activity
routines during the COVID-19 pandemic. Sport Sci Health
2020;16:619-24. Crossref
23. Ammar A, Brach M, Trabelsi K, et al. Effects of COVID-19 home confinement on eating behaviour
and physical activity: results of the ECLB-COVID19
International Online Survey. Nutrients 2020;12:1583. Crossref
24. Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: the
need for prevention and early intervention. JAMA Intern
Med 2020;180:817-8. Crossref
25. Ruiz-Roso MB, Knott-Torcal C, Matilla-Escalante DC, et al. COVID-19 lockdown and changes of the dietary pattern
and physical activity habits in a cohort of patients with type
2 diabetes mellitus. Nutrients 2020;12:2327. Crossref
26. Ceolin G, Moreira JD, Mendes BC, Schroeder J, Di Pietro PF, Rieger DK. Nutritional challenges in older adults during the COVID-19 pandemic [in Spanish]. Rev Nutrição
2020;33:e200174.Crossref
27. Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease
2019 (COVID-19). J Telemed Telecare 2020;26:309-13. Crossref
28. Scherrenberg M, Wilhelm M, Hansen D, et al. The future is now: a call for action for cardiac telerehabilitation in
the COVID-19 pandemic from the secondary prevention
and rehabilitation section of the European Association of
Preventive Cardiology. Eur J Prev Cardiol 2021;28:524-40. Crossref
29. Turolla A, Rossettini G, Viceconti A, Palese A, Geri T.
Musculoskeletal physical therapy during the COVID-19
pandemic: is telerehabilitation the answer? Phys Ther
2020;100:1260-4. Crossref
30. Norman CD, Skinner HA. eHealth literacy: essential skills for consumer health in a networked world. J Med Internet
Res 2006;8:e9. Crossref
31. Jasemian Y. Elderly comfort and compliance to modern telemedicine system at home. 1st International ICST
Workshop on Connectivity, Mobility and Patients’ Comfort.
2008. Available from: https://eudl.eu/doi/10.4108/icst.pervasivehealth2008.2516. Accessed 5 May 2020. Crossref
32. Bujnowska-Fedak MM, Grata-Borkowska U. Use of telemedicine-based care for the aging and elderly:
promises and pitfalls. Smart Homecare Technol Telehealth
2015;3:91-105. Crossref
33. Chesser A, Burke A, Reyes J, Rohrberg T. Navigating the digital divide: a systematic review of eHealth literacy in
underserved populations in the United States. Inform
Health Soc Care 2016;41:1-19. Crossref
34. Chua SE, Cheung V, McAlonan GM, et al. Stress and psychological impact on SARS patients during the
outbreak. Can J Psychiatry 2004;49:385-90. Crossref
35. Mak IW, Chu CM, Pan PC, Yiu MG, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp
Psychiatry 2009;31:318-26.Crossref
36. Wang Y, Duan Z, Ma Z, et al. Epidemiology of mental health problems among patients with cancer during COVID-19 pandemic. Transl Psychiatry 2020;10:263. Crossref
37. Newell S, Sanson-Fisher RW, Girgis A, Bonaventura A. How well do medical oncologists’ perceptions reflect
their patients’ reported physical and psychosocial
problems? Data from a survey of five oncologists. Cancer
1998;83:1640-51. Crossref
38. Sakai H, Umeda M, Okuyama H, Nakamura S. Differences in perception of breast cancer treatment between patients,
physicians, and nurses and unmet information needs in
Japan. Support Care Cancer 2020;28:2331-8. Crossref
39. Söllner W, DeVries A, Steixner E, et al. How successful are oncologists in identifying patient distress, perceived
social support, and need for psychosocial counselling? Br J
Cancer 2001;84:179-85. Crossref
40. Catania C, Spitaleri G, Del Signore E, et al. Fears and perception of the impact of COVID-19 on patients with
lung cancer: a mono-institutional survey. Front Oncol
2020;10:584612. Crossref
41. Coronavirus.gov. Hong Kong SAR Government. Together, We Fight the Virus. Available from: https://www.coronavirus.gov.hk/eng/index.html. Accessed 7 Nov 2020.