Hong Kong Med J 2023 Apr;29(2):104.e1–9 | Epub 14 Apr 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
EDITORIAL
Postgraduate medical education: see one, do one, teach one…and what else?
HY So, FCICM, FHKAM (Anaesthesiology)
Educationist, Hong Kong Academy of Medicine, Hong Kong SAR, China
This editorial is based on the Halnan Lecture, which was presented at the Tripartite Medical Education Conference on 15 January 2023 by Dr HY So, Educationist, Hong Kong Academy of Medicine.
Corresponding author: Dr HY So (sohy@ha.org.hk)
Abstract
Postgraduate medical education (PGME) faces many
challenges and must evolve. Three principles can guide
this evolution. First, PGME apprenticeship, a form of
situated learning, is guided by the four dimensions
of the Cognitive Apprenticeship Model: content,
method, sequence, and sociology. Second, situated
learning involves experiential learning and inquiry
processes; it is most effective for learners practicing
self-directed learning. The promotion of self-directed
learning requires consideration of its three dimensions:
process, person, and context. Finally, the need for competency-based PGME can be accomplished through holistic models, such as situated learning.
The implementation of this evolution should be
informed by the characteristics of the new paradigm,
inner and outer settings of the organisations, and
individuals involved. Implementation encompasses
communication to engage stakeholders, training
process redesign in accordance with the new
paradigm, faculty development to empower and
engage involved individuals, and research to enhance
the understanding of PGME.
Introduction
Postgraduate medical education (PGME), a mission
of the Hong Kong Academy of Medicine (HKAM),
is important for the development of competent
caring medical practitioners and for efforts to ensure
high-quality patient care.1 As the HKAM celebrates
its 30th anniversary, there is a need to examine
how it must evolve to accommodate changes in
the healthcare landscape, diverse patient needs,
the increasing complexity of medical practice, and
advances in educational practices.2 Despite the limited evidence available regarding PGME, some
principles can guide the necessary evolution. Here,
I focus on three themes: (1) PGME is situated
learning, (2) PGME should be self-directed, and (3)
PGME should be competency-based. Considering
the space limitations, I provide a broad framework;
readers can acquire additional information from
relevant articles included in the References.
Postgraduate medical education is
situated learning
Understanding situated learning
Postgraduate training in medicine mainly occurs in
the workplace through participation in clinical tasks.
This training approach can be regarded as a process
of apprenticeship after a doctor in training enters
a particular specialty or ‘community of practice’
(CoP; discussed in detail below).3 The principles
of this learning process include increasing learner engagement in the daily work of the community,
professional identity formation, and development of
the ability to communicate using the community’s
language and act according to the community’s
norms.4 Thus, learning is embedded in everyday
activities and is no longer considered ‘necessarily or
directly dependent on pedagogical goals or official
agenda’.4 This mode of learning is consistent with the
anthropological concept of ‘situated learning’.
The notion of ‘situated learning’ emerged
from the work of Lave,5 who identified distinct differences between learning in a school setting and
learning through everyday activities. In a school
setting, education focuses on individual learners;
it is dominated by cognitivism (ie, information
transmission and processing) and behaviourism
(ie, shaping of behaviour via reinforcement and
punishment). In this context, knowledge is perceived
as an ‘inert, self-sufficient, abstract, self-contained,
symbolic substance, which is transferred from
the teacher to the learner and becomes stored in
the learner’s memory for later use’.6 In contrast,
proponents of situated learning theory recognise
that learning is the active construction of knowledge
through social collaborations and a focus on social
relationships and interactions, rather than a focus
on individual learners. Thus, they view knowledge
as a tool. An individual can possess a tool without
being able to use it; use of the tool helps to increase
the individual’s understanding of the tool and the
relevant context (ie, situation). The specific learning that occurs is a function of three factors in the
context where that learning occurs: the people in
the context, the ‘tools’ used, and the specific activity itself.6
Three decades after Lave published her
seminal work, many researchers in health
professions education use situated learning theory
to guide curriculum design because they recognise
its potential advantages.7 Situated learning places
learners in realistic settings where socially acquired
knowledge is often valued, strategically utilises the
learner’s prior knowledge of a particular subject, and (most importantly) increases the likelihood
of knowledge application within similar contexts.7
For example, Lave asked adults to determine which
of two products in a grocery store was a ‘best buy’.
When participants actually went to a grocery store,
talked with people in their group, and physically
handled various items to compare sizes and shapes,
they correctly answered 98% of the math problems
involved in the experiment. In contrast, when
participants were provided the same math problems
in a paper-and-pencil test format, they correctly
answered 59% of the math problems.5
Cognitive Apprenticeship Model
As a form of apprenticeship, PGME requires
teaching methods that differ from school-based
learning approaches. ‘See one, do one, teach one’
is the method used in traditional apprenticeships.3 However, the learning of complex subjects, such as
PGME, involves components that are not readily
observable, as well as complex relationships and
interactions among teachers and learners. Thus,
Brown et al8 developed a complementary approach to the traditional teaching model, known as the
Cognitive Apprenticeship Model (CAM). The
CAM focuses on four dimensions that are present
in any learning environment: content, methods,
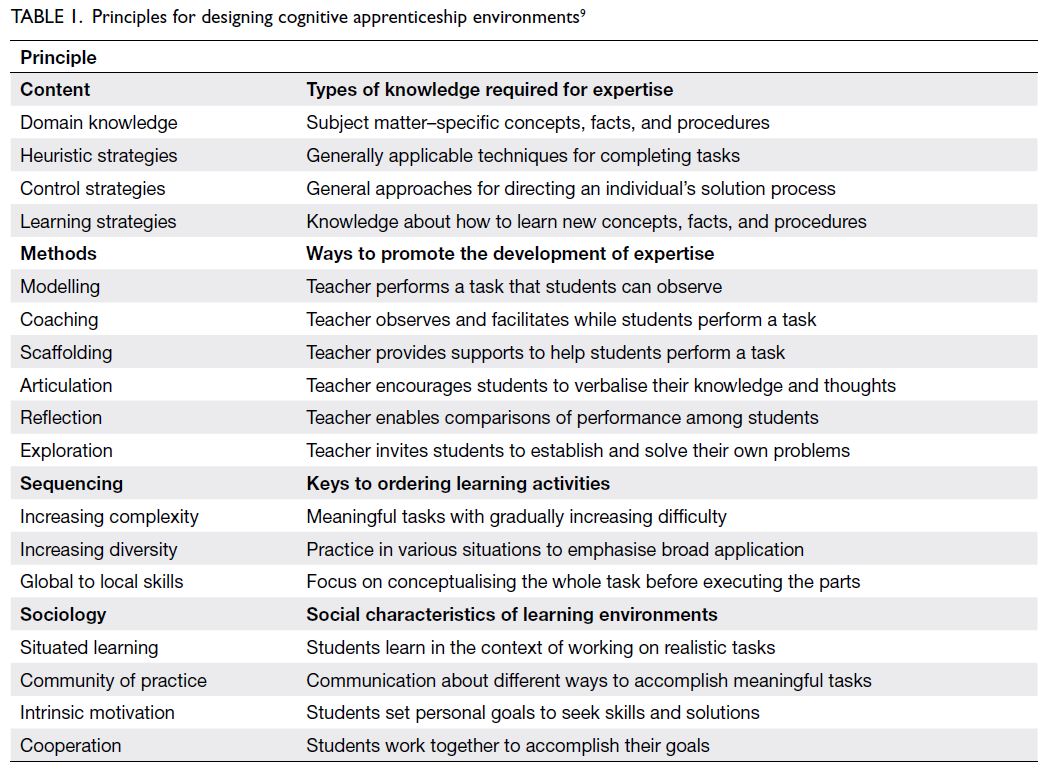
sequencing, and sociology (Table 1).9
Content
Domain knowledge constitutes the explicit concepts,
facts, and procedures associated with an area of
expertise; this type of knowledge is usually found
in textbooks and lectures. Proponents of situated
learning theory and CAM argue that a strong grasp
of domain knowledge is necessary but insufficient for
experts who seek to solve real-world problems. Such
experts must also acquire three types of strategic
knowledge: heuristic strategies, control strategies,
and learning strategies.9
Method
However, strategic knowledge is often tacit; experts
may utilise each type of strategic knowledge
without conscious awareness of such use. Therefore,
apprenticeship teaching methods are designed to
provide learners with opportunities to observe,
engage in, and discover the strategic knowledge
used by experts, within the relevant context. The
six teaching methods in CAM can be categorised
into three groups. The first three methods—modelling, coaching, and scaffolding—represent
the core of traditional apprenticeships. These
methods are intended to help students acquire
an integrated set of skills through observation
(‘see one’) and guided practice (‘do one’). The next
two methods—articulation and reflection—are
designed to help students focus their observations
and gain conscious control of their own problemsolving
strategies. The final method—exploration—aims to encourage learner autonomy in terms of
implementing expert problem-solving processes and
formulating problems.9 I want to emphasise the links
between these teaching methods and Kolb’s Cycle of
Experiential Learning. Situated learning constitutes
experiential learning via participation in clinical
tasks. Kolb10 described experiential learning as a
transformative process. When learners perform or
‘do’ a clinical task, they transform abstract knowledge
into concrete experience. However, learning is only
complete when learners reflect on their concrete
experience, then transform that experience back
into generalised and abstract knowledge to guide
future practice.10 When they are ready, learners can
independently apply this enhanced knowledge in
practice. Kolb’s Cycle supports the purpose of each
group of teaching methods in CAM; it also highlights
the value of facilitated reflection and feedback in
workplace-based learning, including workplace-based
assessment.11
Sequencing
The sequence in which clinical tasks are performed
affects learning efficacy. Cognitive Apprenticeship
Model offers three principles to guide sequencing.
First, tasks should progress from simple to complex,
requiring increasing amounts of skill and conceptual knowledge. Next, diversity should gradually increase
to allow learners to identify conditions in which
they should use various skills and strategies. Finally,
activities and tasks should progress from a global
perspective to a local perspective; thus, learners
should build a conceptual map of an activity before
considering its details (ie, specific tasks). The
establishment of a clear conceptual model of the
overall activity helps learners understand the part
they are performing, which improves their ability
to engage in progress monitoring and develop self-correction
skills.9
Sociology
Lastly, the social characteristics of learning
environments (ie, ‘sociology’) can affect motivation,
confidence, and orientation towards problems that
individuals encounter as they learn. The first element
of sociology, which is a core consideration, is ensuring
that learners perform tasks and solve problems in
an environment that reflects the real-world nature
of such tasks. The second element of sociology
is intrinsic motivation. Learning environments
should be created in manner that enables learners
to perform tasks because the tasks are intrinsically
related to their goals of interest, rather than because
the tasks are driven by extrinsic motivation (eg,
earning a good grade or pleasing the teacher). The
third element of sociology is the aforementioned
CoP, which comprises a group of people who share
a passion for something they do and learn how to
do it better during repeated interactions; learning
may be an intentional or incidental outcome of those
interactions. Communities of practice have three
key characteristics: a shared domain of interest;
engagement in joint activities, information sharing,
and relationship building among members; and the
development of a shared repertoire of resources for
practice.7 Key components of situated learning are
relationships among CoP members and engagement
in active communication about skills related to their
expertise. Full members of the CoP (ie, specialists)
provide guidance to doctors in training; they also
learn from each other through these interactions.
The final element of sociology is cooperation:
learners should work together in a manner that
fosters cooperative problem solving. There are many
ways in which peer learners can help each other to
learn; for example, senior learners can guide junior
learners in practice, giving and receiving peer
feedback, or solving problems together. Learning via
collaboration is a powerful motivator and a powerful
mechanism for the expansion of learning resources.9
There is evidence that learners can receive diverse
benefits from peer-assisted learning.12 Thus, it
is important to empower doctors in training via
teaching and feedback, rather than waiting until
their specialty training is completed.
Implementation considerations
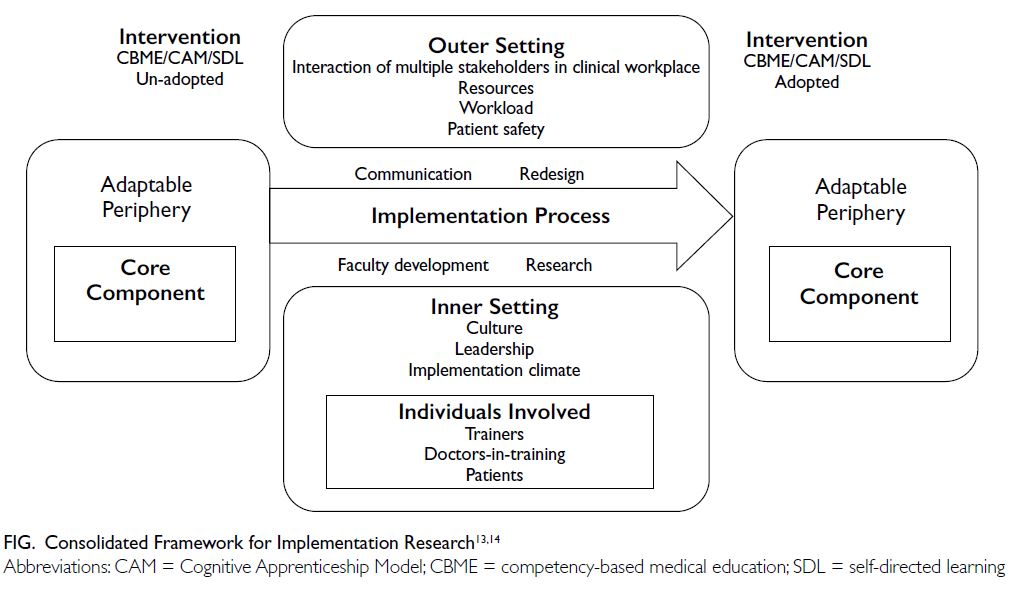
I will use the Consolidated Framework for
Implementation Research (CFIR) model to guide
this portion of the discussion (Fig).13 14 The CFIR,
a conceptual model for implementing change
or intervention, consists of five domains. The
implementation process, one of the domains, should
be informed by considerations of the other four
domains: characteristics of the ‘intervention’, inner
setting, outer settings, and individuals involved in
the intervention.13
Intervention
In this discussion, the intervention is the new
model of learning: CAM. Damschroder et al13
identified multiple intervention characteristics that
may influence the difficulty encountered during
implementation. Model complexity and resource
implications, particularly in terms of workforce,
could be key challenges. Stakeholder engagement via
communication is essential to highlight the potential
benefits of this new mode of learning. Testing on a
small scale and exploring adaptation to the Hong
Kong context would also facilitate implementation.13
Inner setting
The implementation of this new mode of learning
must be led by an organisation (eg, a college).
Leadership, culture, organisational implementation
climate, and relevant experiences may affect the
implementation of this paradigm shift14; evaluation
and management of these factors are potential challenges. Sharing and collaboration among colleges may be useful strategies.
Outer settings
Postgraduate medical education occurs in the clinical
setting where challenges can arise from interactions
among trainers, doctors in training, the HKAM
and colleges, employers, regulators, and patients
and the caregivers. Two key challenges in this outer
setting are patient safety and the tension between
service and training.3 Patient safety concerns have
led to a substantial increase in the use of simulation
in medical education, based on the rationale that
simulated practice accelerates the learning curve
while providing a safe environment for skills rehearsal
and opportunities to learn from error.3 Simulation
should be integrated into postgraduate specialty
curricula as a core delivery vehicle to complement
workplace-based learning for both individual skill
development and interprofessional team-based
training.15 The other key issue is that doctors in
training and their trainers are both clinic employees;
thus, a managed tension exists between service and
training, which requires ongoing dialogue among
stakeholders to ensure appropriate balance.3
Individuals involved
The individuals involved, especially the trainers
and doctors in training, are part of the inner setting
but regarded as a separate domain under the CFIR.
Although PGME is ‘situated’, it does not necessarily
indicate that effective methods are used to facilitate situated learning. Most clinical teachers are not
trained; they simply use teaching methods that
they experienced in schools.16 Therefore, faculty
development (discussed in detail below) is essential.
Moreover, there has been some discussion regarding
colleges in which not many of their specialists are
motivated to teach. However, situated learning
depends on interactions among CoP members;
learning opportunities can only be maximised
through the engagement and empowerment of
all members. Accordingly, faculty development
should not be restricted to a selected group, and
the objective of such development should not be
limited to the acquisition of teaching skills; it should
be oriented towards motivating participants to
establish a professional identity in which they serve
as a clinical teacher.17 Doctors in training cannot be
passive learners in this process. In addition to active
participation in clinical tasks, they must actively seek
out opportunities (eg, reading medical literature,
attending workshops and conferences, and receiving
mentorship and guidance from experienced
practitioners) to enhance their knowledge and skills,
then use those enhancements to improve their
clinical expertise. Furthermore, in contrast to the
school setting, situated learning is not organised
according to a curriculum, especially because clinical
encounters are not always predictable. Accordingly,
doctors in training must assume responsibility for
their own learning.18 However, there is evidence that
self-directed learning (SDL) is uncommon among
learners in Hong Kong.19 This is the second theme
that I will address.
Postgraduate medical education
should be self-directed
Understanding self-directed learning
The notion that doctors in training must assume
responsibility for their own situated learning is
essential to the concept of SDL. The origin of SDL
is closely linked to adult learning theory.18 Knowles20
defined SDL as a process in which individuals take
initiative (with or without assistance from others) to determine their learning needs, formulate goals,
identify human and material resources for learning,
choose and implement appropriate learning
strategies, and evaluate learning outcomes.
Self-directed learning also requires a paradigm
shift. Traditional teaching (ie, pedagogy) is teacher-directed
and focuses on content delivery. A major
problem with such an educational process is that
learners can become accustomed to habitually
reinforced patterns of perception, thinking,
judgement, feeling, and behaviour; these patterns
may lead to inflexible behaviour and a lack of
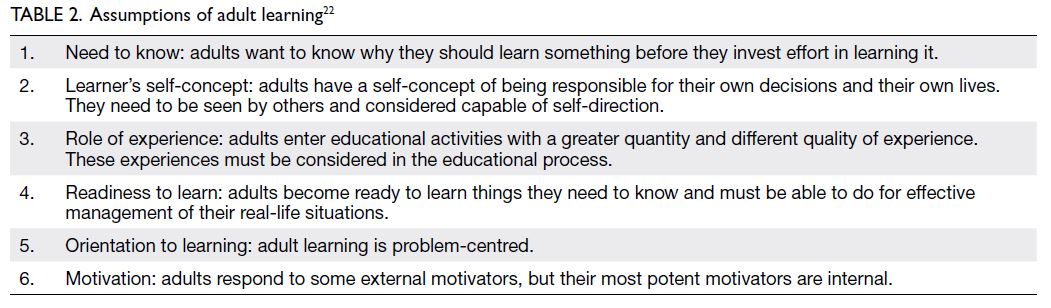
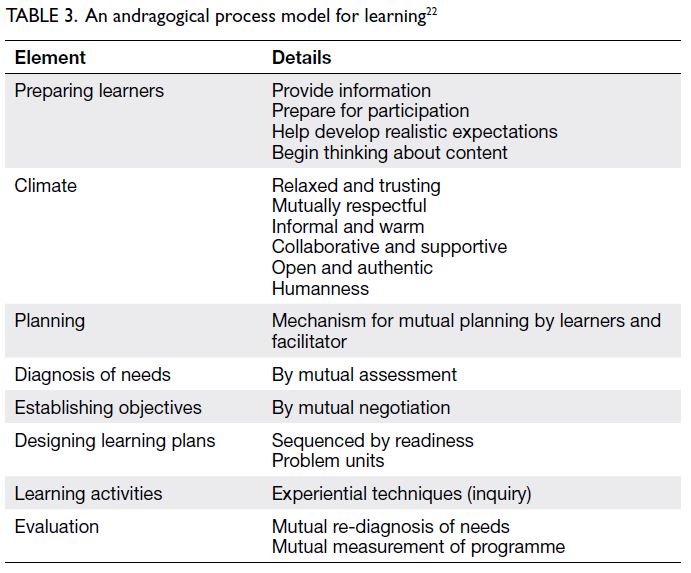
motivation for SDL.21 The direction of adult learning (ie, andragogy) involves engaging learners in an
inquiry process. Based on the six assumptions of
adult learning (Table 2), Knowles et al22 described
a process which teachers can use to facilitate such
inquiry (Table 3). It has been argued that SDL is a
universally necessary competency in a changing
world, particularly for individuals in complex fields
such as medicine.21 Indeed, the Accreditation Council for Graduate Medical Education has
recommended that doctors in training become
self-directed learners, use innovative tools (eg,
computerised diaries and portfolios) to evaluate
their own learning, and facilitate learning in other
individuals.23
More recently, Hase and Kenyon24 expanded
the concept of SDL and proposed the notion of
heutagogy (ie, self-determined learning) as a learning
paradigm for the information age. Although the
concept is complex, it can be summarised as follows:
modern technology enables explorations of existing
knowledge, connections with experts, collaborations
with peers, reflections on personal experiences,
and the creation and sharing of knowledge. This
technology makes learning flexible, allowing
learners to learn at their preferred time and in their
preferred manner.22 Accordingly, e-learning utilising
this technology should be viewed as an approach
to re-define the learning experience, rather than
as a simple substitute for more traditional learning
methods.25 This learning paradigm is relevant to PGME and lifelong learning.
Dimensions of self-directed learning and
implications for implementation
The definition established by Knowles et al22
implies a process to facilitate SDL. However, there
is increasing recognition that, in addition to the
process component, the construct of SDL has
multiple dimensions.18 22 26 Additionally, Ricotta et al26
suggested that the application of SDL in clinical
settings would require approaches that differ from
classroom methods because of its more rapid pace
and the need to consider patient safety. Here, I
will address the three dimensions described in
two models of SDL in medical education: process,
person, and context.18 26
Process
As mentioned above, trainers must utilise
appropriate strategies to facilitate the inquiry
process. In addition to the process described by
Knowles et al22 (Table 3), Sawatsky et al18 and
Ricotta et al26 described learning processes in SDL;
although the three groups of authors used different
terminology in their descriptions, all processes are
conceptually similar. The fundamental requirements
of strategies to facilitate SDL should focus on learner
engagement, emphasise curiosity, support inquiry-based
approaches, and promote exploration.26
Person
Self-directed learning is a question of the extent
to which learners maintain active control of the
learning process.27 Thus, the use of appropriate
facilitation processes is necessary but not sufficient to fulfil the goals of SDL. Learners must thoroughly
grasp essential learning skills and develop personal
attributes necessary to control the inquiry process.
Feedback literacy is a particularly important
learning skill because reflection and feedback are
indispensable components of experiential learning.
Carless28 defined feedback as an interactive process
in which students interpret and use various inputs
to enhance their work. The utilisation of feedback,
combined with engagement in actions that close the
feedback loop, is an active process. In his model of
feedback literacy, Carless28 established three pre-conditions:
appreciation of feedback, formation of
judgements, and management of affect. Trainers can
help foster feedback literacy through strategies such
as peer feedback.
The personal attributes of curiosity,
perseverance, flexibility, and integrity are
prerequisites for individuals who wish to engage
in SDL. Motivation is a key factor which energises
and connects these attributes.26 The predispositions
of doctors in training towards SDL will gradually
change as they develop confidence in SDL and
gain a more sophisticated knowledge framework.18
Trainers should assess learner readiness and cultivate
SDL through the adoption of teaching strategies
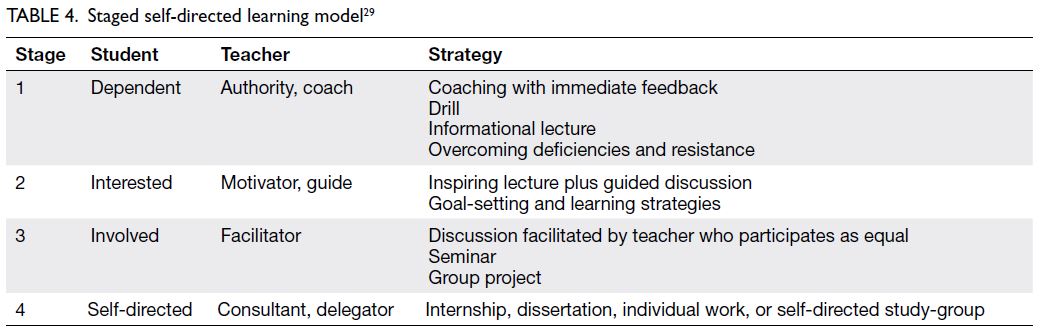
appropriate for each stage (Table 4).29
Context
The personal attributes described above must
be developed in an effective and safe learning
environment. Importantly, these attributes may
be threatened by approaches that emphasise
professional examinations and competition among
doctors in training. The cultivation of SDL requires
a paradigm shift from a traditionally competitive
learning environment to an environment that
encourages humility and accepts failure.26 Trainers
should establish psychological safety, encourage
curiosity, and normalise cognitive dissonance. At
the organisational level, a curiosity-focused culture
can facilitate learning activities. The acceptance
of uncertainty and promotion of inquiry-based
approaches help learners to become motivated
and prepared to pursue SDL. The creation of an
environment that supports SDL development
requires new strategies, prioritisation of learner
engagement, and encouragement of questioning.26
Postgraduate medical education
should be competency-based
Understanding competency-based medical
education
Building on the above discussion regarding the
learning environment and methods necessary
for PGME, I will explore the desired outcomes.
Although the concept of outcome-based or competency-based education emerged nearly a century ago, its popularisation in medical
education began in the 1990s when leaders in the
Canadian medical profession observed widespread
dissatisfaction in many areas.30 31 They attributed
this dissatisfaction to forces such as the availability
of medical information on the internet, patient
consumerism, government regulations, financial
imperatives, litigation, technology, and an overall
explosion of medical knowledge; thus, they
concluded that medical education could no longer
be planned with a focus solely on the latest aspects
of medical diagnosis and treatment.31 Modern
professional training should create doctors who can
accommodate rapid advances in medicine, recognise
patient perspectives, appreciate the skills of other
health professionals, and work effectively in teams.32
Therefore, training programmes should address
clinical skills and knowledge, along with other
aspects of clinical competence required among
doctors (eg, communication skills, attitude, team
working, audit, research, teaching, and SDL).32 The
Royal College of Physicians and Surgeons of Canada
included seven competencies under the CanMEDS
framework.33 34 Similar developments soon followed
in other countries.23 35 36 In 2010, the Hong Kong
Academy of Medicine published a position statement
indicating that the ‘Hong Kong Specialist’ should
demonstrate competency in seven broad domains:
professional expertise, health promoter, inter-personal
communication, team working, academic,
manager-leader, and professionalism.37
Implementation process
A common approach to teaching multiple
competencies involves dividing them into individual
units, then teaching them separately using methods
that are appropriate for each competency. Among
educationists, this is known as the ‘atomistic
approach’, which is difficult to implement because
the curriculum is already very full. Moreover, this approach is ineffective in situations that involve
complex learning because the competencies are
closely related to each other and the whole is more
than the sum of its parts—it contains the elements
and the relationships among those elements.38 A
holistic approach using real-world tasks avoids
potential problems regarding compartmentalisation
and fragmentation.38 In the setting of PGME, situated learning and CAM are appropriate methods.
Accordingly, the three themes discussed here are
closely linked together and can be regarded as a
single paradigm for modern PGME.
The implementation process of this new
paradigm, one of the five domains of the CFIR (Fig),13 14
consists of four strategies based on implementation
research and theories: communication, redesign,
faculty development, and research.31
Communication
The new paradigm is very different from current
practice; it is also complex and involves significant
resource investments. Successful implementation
heavily relies on effective communication to
engage stakeholders in both the inner and outer
settings. Frank and Danoff31 suggested the use of a
social marketing–based communication plan. The
framework of social marketing includes concepts
of exchange theory, audience segmentation,
competition, consumer orientation, and continuous
monitoring.39
Redesign
The Academy and the colleges are responsible for
setting educational standards for PGME objectives,
training programme accreditation, assessment,
professional examinations, and continuing medical
education standards; thus, they should redesign
the relevant educational standards to incorporate
a foundation that involves all competencies.31 This
integrative approach would include efforts to align
curricular objectives with experiential training in the clinical workplace.40 The incorporation of workplace-based
assessment into the curriculum is an example
of such integration.41
Faculty development
Steinert42 defined faculty development as all
activities that health professionals pursue to
improve their knowledge, skills, and behaviours as
teachers and educators, leaders and managers, and
researchers and scholars, in both individual and
group settings. The engagement and empowerment
of all CoP members in teaching and learning are
prerequisites for implementing community-based
medical education via situated learning. Steinert
et al17 recommended that the process of faculty
development mirror the process of PGME itself: it
should utilise SDL and view learning as a process of
inquiry through experiential learning, rather than
as a process of direct transmission. It should also
utilise situated learning theory and view teaching
skills as tools to be used in specific contexts, rather
than objects that can be acquired. Thus, although
workshops may be a useful starting point, there is a
need to focus on longitudinal development via faculty
development communities.17 As mentioned above,
the objective of faculty development should not be
limited to teaching skill acquisition; it should include
the establishment of a professional identity as a
clinical educator, as well as motivation for teaching.17
Similarly, faculty development should promote a
culture of change and further development of PGME
through innovation, research, and organisational
transformation.17 42
Research
Finally, the field of PGME is comparatively new
and does not have a strong academic presence.
Most of its practical approaches are derived from
undergraduate medical education or general
education. However, there are some concerns,
learning methods, and practices with uniquely
‘postgraduate’ origins.3 Considerable research
efforts are necessary to provide evidence that can
drive further improvements in PGME, and resources
are needed to support such efforts.3 31
Conclusion
Health professionals are expected to possess a diverse set of competencies that fulfil current societal needs.
Apprenticeships using real-world clinical tasks
can provide effective competency-based medical
education. However, the traditional ‘see one, do
one, teach one’ approach is inadequate for the
complex learning tasks involved in PGME. Instead,
learning in this environment involves the facilitation
of experiential learning and inquiry, rather than
simple content delivery. To achieve this shift in perspective, teaching methods from CAM and SDL
must be adopted. The cultivation of SDL requires
appropriate context, as well as a CoP with members
who possess teaching skills and attitudes that differ
from traditional teaching. Faculty development is
important for the successful implementation of this
new paradigm; it should be grounded in the same
principles of experiential learning, situated learning,
and SDL. This approach will equip members of the
CoP with essential skills, while supporting effective
communication and engagement. Moreover, it will
cultivate the talent necessary to redesign standards
and practices, while encouraging interest and active
participation in research efforts to advance PGME.
Author contributions
The author was solely responsible for drafting of the
manuscript, approved the final version for publication, and
takes responsibility for its accuracy and integrity.
Funding/support
This editorial received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of interest
The author has disclosed no conflicts of interest.
References
1. McLean M, Cilliers F, Van Wyk JM. Faculty development: yesterday, today and tomorrow. Med Teach 2008;30:555-84. Crossref
2. Patel M. Changes to postgraduate medical education in the 21st century. Clin Med (Lond) 2016;16:311-4. Crossref
3. Swanwick T. Postgraduate medical education: the same, but different. Postgrad Med J 2015;91:179-81. Crossref
4. Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge: Cambridge University Press; 1991. Crossref
5. Lave J. Cognition in Practice: Mind, Mathematics and Culture in Everyday Life. Cambridge: Cambridge University Press; 1988. Crossref
6. Durning SJ, Artino AR. Situativity theory: a perspective on how participants and the environment can interact: AMEE guide no. 52. Med Teach 2011;33:188-99. Crossref
7. O’Brien BC, Battista A. Situated learning theory in health professions education research: a scoping review. Adv Health Sci Educ Theory Pract 2020;25:483-509. Crossref
8. Brown JS, Collins A, Duguid P. Situated cognition and the culture of learning. Educ Res 1989;18:32-42. Crossref
9. Collins A, Kapur M. Cognitive apprenticeship. In: Sawyer RK, editor. The Cambridge Handbook of the Learning Sciences. 2nd ed. Cambridge: Cambridge University Press; 2014:109-27. Crossref
10. Kolb DA. Experiential Learning: Experience as the Source of Learning and Development. Upper Saddle River, NJ: Pearson Education Ltd; 2015.
11. Saedon H, Salleh S, Balakrishnan A, Imray CH, Saedon M. The role of feedback in improving the effectiveness of workplace based assessments: a systematic review. BMC Med Educ 2012;12:25. Crossref
12. Brierley C, Ellis L, Reid ER. Peer-assisted learning in medical education: A systematic review and meta-analysis.
Med Educ 2022;56:365-73. Crossref
13. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services
research findings into practice: a Consolidated Framework
for advancing implementation science. Implement Sci
2009;4:50. Crossref
14. Carney PA, Crites GE, Miller KH, et al. Building and executing a research agenda toward conducting implementation science in medical education. Med Educ Online 2016;21:32405. Crossref
15. Issenberg SB, Mcgaghie WC, Petrusa ER, Lee Gordon D, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach 2005;27:10-28. Crossref
16. MacDougall J, Drummond MJ. The development of medical teachers: an enquiry into the learning histories of 10 experienced medical teachers. Med Educ 2005;39:1213-20. Crossref
17. Steinert Y, Mann K, Anderson B, et al. A systematic review of faculty development initiatives designed to enhance teaching effectiveness: a 10-year update: BEME Guide no. 40. Med Teach 2016;38:769-86. Crossref
18. Sawatsky AP, Ratelle JT, Bonnes SL, Egginton JS, Beckman TJ. A model of self-directed learning in internal medicine residency: a qualitative study using grounded theory. BMC
Med Educ 2017;17:31. Crossref
19. Frambach JM, Driessen EW, Chan LC, van der Vleuten CP. Rethinking the globalisation of problem-based learning:
how culture challenges self-directed learning. Med Educ
2012;46:738-47. Crossref
20. Knowles MS. Self-Directed Learning: A Guide for Learners and Teachers. Chicago: Associated Press; 1975.
21. Morris TH. Self-directed learning: a fundamental competence in a rapidly changing world. Int Rev Educ 2019;65:633-53. Crossref
22. Knowles MS, Holton III EF, Swanson RA. The Adult Learner: The Definitive Classic in Adult Education and Human Resource Development. 5th ed. Woburn, Mass: Butterworth-Heinemann; 2005.
23. Accreditation Council for Graduate Medical Education. Common program requirements. 2022. Available from: https://www.acgme.org/what-we-do/accreditation/common-program-requirements/. Accessed 17 Mar 2023.
24. Hase S, Kenyon C. Self-Determined Learning: Heutagogy in Action. London: Bloomsbury Academic; 2015.
25. Hamilton ER, Rosenberg JM, Akcaoglu M. The Substitution Augmentation Modification Redefinition (SAMR) Model:
a critical review and suggestions for its use. TechTrends
2016;60:433-41. Crossref
26. Ricotta DN, Richards JB, Atkins KM, et al. Self-directed learning in medical education: training for a lifetime of discovery. Teach Learn Med 2022;34:530-40. Crossref
27. Loeng S. Self-directed learning: a core concept in adult education. Educ Res Int 2020;2020:3816132. Crossref
28. Carless D. From teacher transmission of information to student feedback literacy: activating the learner role in
feedback processes. Act Learn High Educ 2020;23:143-53. Crossref
29. Grow GO. Teaching learners to be self-directed. Adult Educ Q 1991;41:125-49. Crossref
30. Harden RM, Crosby JR, Davis MH. AMEE Guide No. 14: Outcome-based education: Part 1—an introduction to
outcome-based education. Med Teach 1999;21:7-14. Crossref
31. Frank JR, Danoff D. The CanMEDS initiative: implementing an outcomes-based framework of physician competencies. Med Teach 2007;29:642-7. Crossref
32. Long G, Gibbon WW. Postgraduate medical education: methodology. Br J Sports Med 2000;34:236-7. Crossref
33. Frank JR. The CanMEDS 2005 Physician Competency Framework. Ottawa: The Royal College of Physicians and Surgeons of Canada; 2005.
34. Snell L, Sherbino J, Frank J. CanMEDS 2015 Physician Competency Framework. Ottawa: Royal College of Physicians and Surgeons of Canada; 2015.
35. Assessment and accreditation of specialist medical programs. Available from: https://www.amc.org.au/accreditation-and-recognition/assessment-accreditation-specialist-medical-programs-assessment-accreditation-specialist-medical-programs/. Accessed 15 Dec 2022.
36. The consensus statement on the role of the doctor. Available from: https://www.medschools.ac.uk/media/1922/role-of-the-doctor-consensus-statement.pdf. Accessed 15 Dec 2022.
37. Hong Kong Academy of Medicine Position Paper on Postgraduate Medical Education. 2010. Available from: https://www.hkam.org.hk/sites/default/files/HKAM_position_paper.pdf. Accessed 17 Mar 2023.
38. van Merriėṅboer JJ, Kirschner PA. A new approach to instruction. In: an Merriėṅboer JJ, Kirschner PA, editors. Ten Steps to Complex Learning: A Systematic Approach to Four-Component Instructional Design. New York: Routledge; 2018: 5-8. Crossref
39. Grier S, Bryant CA. Social marketing in public health. Annu Rev Public Health 2005;26:319-39. Crossref
40. Caverzagie KJ, Nousiainen MT, Ferguson PC, et al. Overarching challenges to the implementation of competency-based medical education. Med Teach 2017;39:588-93. Crossref
41. Lockyer J, Carraccio C, Chan MK, et al. Core principles of assessment in competency-based medical education. Med
Teach 2017;39:609-16. Crossref
42. Steinert Y. Faculty Development in the Health Professions: A Focus on Research and Practice. Dordrecht: Springer;
2014. Crossref