© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Delayed interval delivery in twin pregnancy in
Hong Kong: two case reports
Annie SY Hui, MRCOG1; Winnie WY Chan, MRCOG1; YM Wah, MRCOG1; L Wong, MRCOG1; Hugh Simon HS Lam, MD, FRCPCH2; TY Leung, MD, FRCOG1
1 Department of Obstetrics and Gynaecology, Prince of Wales Hospital, The Chinese University of Hong Kong, Hong Kong
2 Department of Paediatrics, Prince of Wales Hospital, The Chinese University of Hong Kong, Hong Kong
Corresponding author: Dr Annie SY Hui (anniehui@cuhk.edu.hk)
Case report
Case 1
A 40-year-old nulliparous woman carried the index dichorionic diamniotic (DCDA) twin pregnancy,
conceived in 2014 by in vitro fertilisation due to
unexplained infertility. Antenatal investigations
were all unremarkable.
At 26 weeks and 1 day of gestation she
presented to our local delivery suite with signs of
preterm labour. Examination revealed the cervix
to be fully dilated. Maternal corticosteroids for
foetal lung maturation, prophylactic antibiotics and
magnesium sulphate infusion for neuroprotection
were administered. Twin 1 (T1) was delivered
vaginally 4 hours after admission. The baby weighed
800 g, with Apgar scores (AS) of 6 at 1 minute and 8
at 5 minutes. The first blood gas showed a pH of 7.37.
Soon after, uterine contractions subsided
spontaneously and the cervix quickly closed. Twin 2
(T2) membranes remained intact. After counselling,
the couple opted for delayed interval delivery (DID),
aiming to enhance the lung maturity of T2. The cord
of T1 was ligated and placed in the vagina. Oral
nifedipine was added to maintain uterine quiescence.
Twelve hours later, the patient developed regular
uterine contractions with fever of 37.8°C. Vaginal
examination revealed a fully dilated cervix with
bulging membranes and shoulder presentation of
T2, converted manually to cephalic presentation
following uterine relaxation with the tocolytic
atosiban. Twin 2 was born vaginally with a twin-to-twin
delivery interval of 14 hours and weighing 780
g with AS of 4 at 1 minute, 5 at 5 minutes and 7 at 10
minutes and arterial cord gas of pH 6.94. A placental
swab grew Escherichia coli and a high vaginal swab
grew Pseudomonas aeruginosa. The placenta showed
acute chorioamnionitis.
Twin 1 had acute respiratory distress
syndrome and was intubated up to day 27 of life. The
baby was discharged at 4 months of age with severe
bronchopulmonary dysplasia. Mild speech delay
at 3 years of age required additional therapy. Twin
2 benefited from antenatal corticosteroid and was
weaned off mechanical ventilation on day 17 of life and discharged home at 3 months of age. Both twins
have normal growth and development at the age of 6
years.
Case 2
A 39-year-old woman carried the index
monochorionic diamniotic twin pregnancy, conceived
naturally in late 2019. Antenatal investigations and
ultrasound scans every 2 weeks were unremarkable
until 24 weeks and 5 days of gestation when she
was admitted with preterm prelabour rupture of
membranes. Maternal corticosteroids for foetal
lung maturation and prophylactic antibiotics were
administered. Maternal leukocytosis of 15.5 × 109/L
and raised C-reactive protein of 16.3 g/L were noted,
but high vaginal swab and mid-stream urine cultures
were negative. Three days later, she went into
spontaneous labour. Magnesium sulphate infusion
was commenced for neuroprotection. Twin 1 was
delivered vaginally and weighed 670 g. Apgar scores
were 6 at 1 minute and 8 at 5 minutes, and arterial
cord gas pH was 7.349.
Uterine contractions subsided afterwards and
the cervix closed. In view of extreme prematurity,
the couple opted for DID. High ligation of the cord
was performed (Fig). The patient continued to
receive intravenous ampicillin, metronidazole and
oral erythromycin with monitoring of vital signs.
There were no signs of sepsis, and serial blood
tests revealed that white cell count and C-reactive
protein had normalised after delivery of T1. Serial
cardiotocography of T2 showed normal foetal heart
rate pattern and ultrasound confirmed normal
middle cerebral artery peak systolic velocity. Nine
days later, at 26 weeks and 4 days gestation, preterm
prelabour rupture of membranes of T2 occurred.
Labour was induced by syntocinon infusion but
fresh per vaginal bleeding was noted 5 hours later.
Cardiotocography showed a non-reassuring pattern
but the cervix was only 3 cm dilated. Emergency
lower segment caesarean section was performed
for suspected foetal distress. Twin 2 was delivered
weighing 860 g with AS of 6 at both 1 and 5 minutes,
and arterial cord gas pH of 7.4.
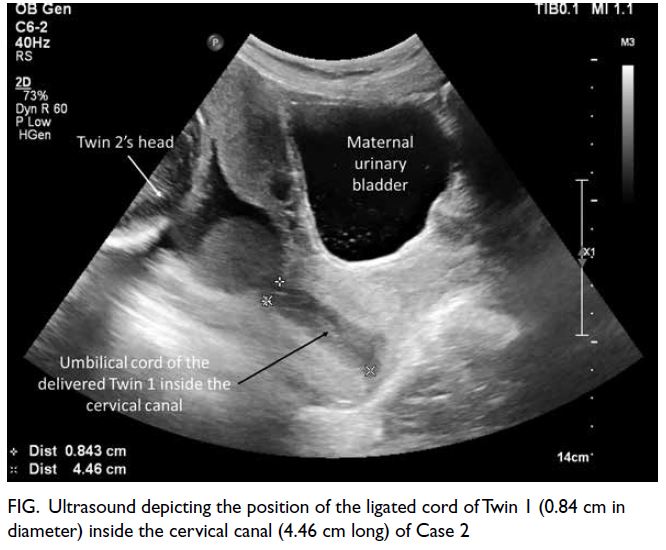
Figure. Ultrasound depicting the position of the ligated cord of Twin 1 (0.84 cm in diameter) inside the cervical canal (4.46 cm long) of Case 2
Apart from severe respiratory distress
syndrome, T1 had E coli septicaemia, a large left
subdural haematoma and right intraventricular
haemorrhage, disseminated intravascular
coagulopathy, and seizures. Despite intensive
treatment, T1 deteriorated and died on day 17 of life.
Twin 2 remained stable and was extubated to non-invasive
ventilation on day 9. Cranial ultrasounds
were normal. Twin 2 was discharged home at
3 months of age and remains well at 1 year of age at
the time of writing.
Discussion
To the best of our knowledge these two cases are the first reported DID in Hong Kong. Twin pregnancies
are at higher risk of preterm delivery and DID has
been proposed to improve survival of the second
twin. In a recent systematic review of 492 multifetal
pregnancies managed with DID, the reported twin-to-twin delivery interval ranged from 1 to 153 days
with a median of 29 days. Delayed interval delivery
was associated with significantly improved perinatal
survival of the remaining foetus compared with
the co-twin (odds ratio=5.22, 95% confidence
interval=2.95-9.25).1 A delay as short as one day may
be sufficient for steroid treatment to enhance foetal
lung maturation, as illustrated by Case 1: T1 had
respiratory distress syndrome and required a longer
duration of intubation and hospitalisation than T2.
Although T2 had acute foetal distress secondary to
in-utero infection and shoulder presentation, T2
recovered rapidly from the acute event with no long-term
sequelae.
The beneficial effect of DID is more often
described in DCDA twins (odds ratio=14.89,
95% confidence interval=6.19-35.84).1 Data on
monochorionic diamniotic twins are sparse since
monochorionicity is often regarded as a contra-indication
for DID due to the potential risk
associated with vascular anastomoses between the
twins.2 Nonetheless with complete occlusion of the
first twin’s umbilical vessels on delivery, the risk of
vascular instability for T2 should be minimised, as
illustrated in our Case 2.3 4 Interestingly in Case 2,
only T1 had in-utero infection with consequent E coli
septicaemia. It is possible that the inter-twin
membrane acted as a barrier and prevented or
delayed spread of infection to the second twin.
There are several elements to consider when
deciding to opt for DID. First, the underlying cause
of preterm labour is often unknown at the time of
presentation. If there is subclinical infection or
placental abruption, leaving the second twin in utero
may be detrimental. Second, a secondary ascending
infection may occur following delivery of the first
twin. Obstetricians should carefully consider the
risks and benefits of DID versus those of delivery
at periviable or extreme preterm gestation. Extra
precautions should be taken before and after opting
for DID, including a high ligature of the first twin’s
cord, antibiotic cover, and close surveillance of
maternal and foetal well-being.5
Author contributions
Concept or design: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: ASY Hui, TY Leung.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: ASY Hui, TY Leung.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was approved by the Joint Chinese University of Hong Kong–New Territories East Cluster Clinical Research
Ethics Committee (Ref No.: 2021.159). Both patients provided
informed consent for the publication of non-identifiable
information.
References
1. Cheung KW, Seto MT, Wang W, Lai CW, Kilby MD, Ng EH. Effect of delayed interval delivery of remaining fetus(es) in multiple pregnancies on survival: a systematic review
and meta-analysis. Am J Obstet Gynecol 2020;222:306-19.e18. Crossref
2. Minakami H, Honma Y, Izumi A, Sayama M, Sato I. Emergency cervical cerclage after the first delivery in a
twin pregnancy with dichorionic placenta. Am J Obstet
Gynecol 1995;173:345-6. Crossref
3. Ting YH, Poon LC, Tse WT, et al. Outcome of
radiofrequency ablation for selective fetal reduction
before vs at or after 16 gestational weeks in complicated monochorionic pregnancy. Ultrasound Obstet Gynecol
2021;58:214-20. Crossref
4. Lu J, Ting YH, Law KM, Lau TK, Leung TY. Radiofrequency ablation for selective reduction in complicated
monochorionic multiple pregnancies. Fetal Diagn Ther
2013;34:211-6. Crossref
5. Porreco RP, Farkouh LJ. Multifetal gestation: role of
delayed-interval delivery. Available from: https://www.uptodate.com/contents/multifetal-gestation-role-of-delayed-interval-delivery. Accessed 4 Oct 2021.

