© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
COMMENTARY
Adult patients in paediatric intensive care units
Karen KY Leung, MB, BS, MRCPCH1; KL Hon, MD, FCCM1; Felix Oberender, MRCPCH, FCICM2; Patrick Ip, MB, BS, FRCPCH3; Joanna YL Tung, MB, BS, MRCPCH4
1 Paediatric Intensive Care Unit, Department of Paediatrics and Adolescent Medicine, Hong Kong Children’s Hospital, Hong Kong
2 Paediatric Intensive Care Unit, Monash Children’s Hospital Melbourne and Department of Paediatrics, Faculty of Medicine, Nursing and Health Sciences, Monash University, Australia
3 Department of Paediatrics and Adolescent Medicine, The University of Hong Kong, Hong Kong
4 Department of Paediatrics and Adolescent Medicine, Hong Kong Children’s Hospital, Hong Kong
Corresponding author: Dr KL Hon (ehon@hotmail.com)
Introduction
With advancement in technology and medical
care, approximately 1 in 10 paediatric patients with
chronic diseases and life-threatening conditions can
now survive into adulthood.1 Paediatricians caring
for critically ill adults in the paediatric intensive
care unit (PICU) should be aware of the potential
challenges that are unique to this group of patients.
We recently admitted to our PICU a patient in his 30s
with chronic renal disease and respiratory failure.
The patient had a complex history of end-stage
renal failure due to crescentic glomerulonephritis,
and previous peritoneal dialysis and cadaveric renal
transplant had been unsuccessful. He had received
subsequent haemodialysis under the care of the
paediatric nephrology unit. He had severe skeletal
deformities and multicentric carpotarsal osteolysis
syndrome likely due to a heterozygous mutation in
the MAFB gene.2 The patient developed respiratory
failure and necessitated admission to the PICU for
stabilisation.
In Hong Kong, many patients with chronic
childhood illnesses receive excellent multidisciplinary
care from territory-wide paediatric services. When
these patients reach adulthood, the transition
to adult services involves multiple stakeholders,
including paediatricians, adult physicians, allied
healthcare professionals, and the patient’s family, all
having to work together in the patient’s best interest.
This transition can involve several challenges. Firstly,
paediatricians and paediatric allied health providers
may be unfamiliar with adult diseases and must
continue the child’s care until they are transitioned
to adult services. Likewise, adult physicians are
often unfamiliar with paediatric conditions with
degenerative sequelae and may be reluctant to take
on the risks in managing these patients. Secondly,
there is a lack of comprehensive healthcare policy
on this subject matter, and this can affect healthcare
resource allocation and budgeting. Thirdly, there
is currently no standard paediatric transitional
programme or educational framework to prepare
patients and their families for transition into the adult healthcare services.3 Lastly, patients and
their families, who have become familiar with the
paediatric approach, might have difficulty adapting
to adult services or even lose confidence in their
medical professionals during the transition period.
Transitional care is widely defined as ‘the
purposeful, planned movement of adolescents and
young adults with chronic physical and medical
conditions from child-centred to adult-oriented
healthcare systems’.4 An effective transition process
can provide appropriate high-quality uninterrupted
medical care services for the patient, and a
communication platform for the main participants
in the patient’s treatment to enhance the patient’s
health, life outcomes, self-management, and
autonomy.4 5 6 7 8 9 In contrast, a premature transition
to adult-oriented therapy may lead to insufficient
preparation, resulting in transition failure, non-adherence
to treatment and poor engagement
with healthcare services subsequently, excess
morbidity, and even mortality.10 11 12 Therefore, a better
management strategy for chronically ill adolescents
is necessary to address the additional needs of
patients in adult life.11 Data on the overall number
of patients involved are scarce; however, registries of
subspecialty populations provide strong evidence to
support the general consensus that transitional care
is a growing challenge.13 14
Transitional care of paediatric patients to
adult care in Hong Kong should be easy to carry
out, as the majority of these patients with chronic
conditions are managed under the public healthcare
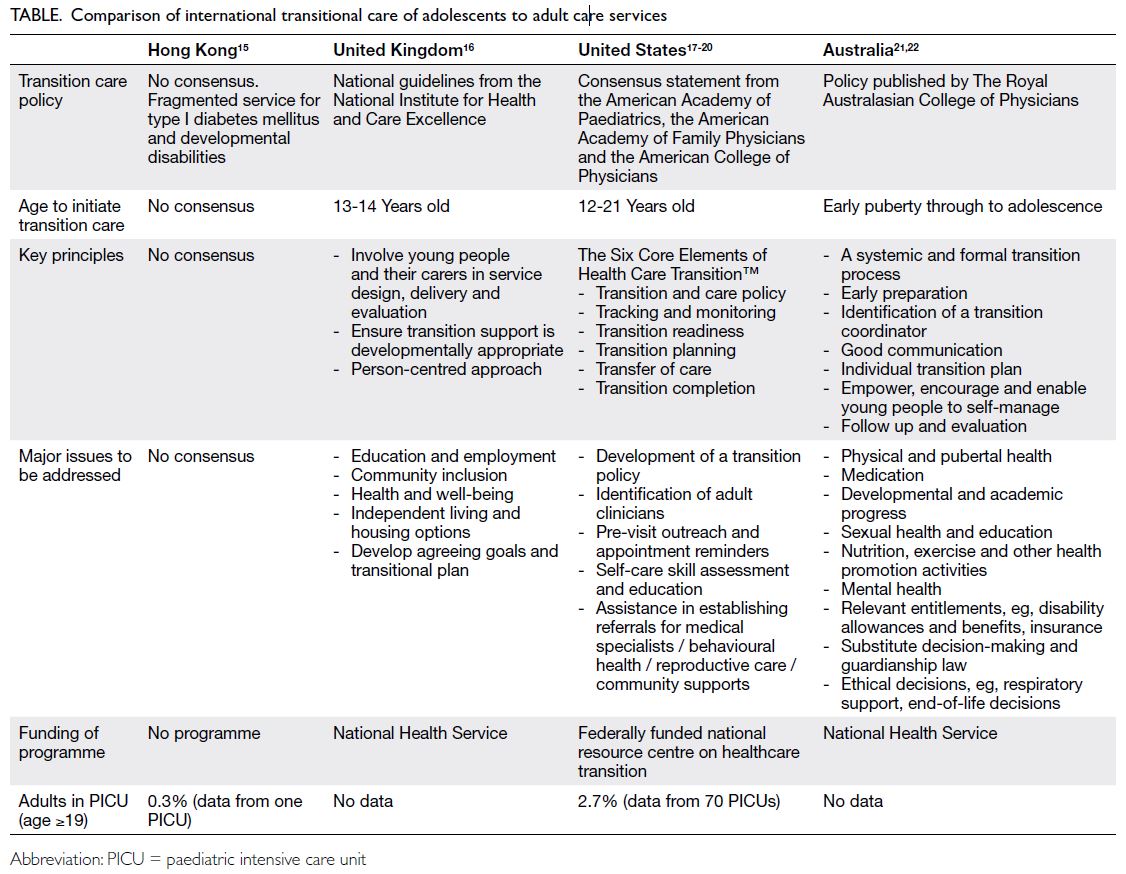
system. However, paediatric transitional care
services in Hong Kong are rather underdeveloped
and fragmented and, in comparison with other
countries, lack an agreed framework3 (Table 15 16 17 18 19 20 21 22).
In Hong Kong, only limited success in transition
care has been established, primarily in patients
with cerebral palsy, Down syndrome, and diabetes
mellitus. Notorious challenges are present for those
with oncologic diseases, congenital heart diseases,
chronic renal diseases on renal replacement, and
inborn errors of metabolism. Transitional care for most of these other chronic conditions remains
fragmented, and for solid organ transplant recipients
it is even less developed.8 9 In 2010, a Hong Kong study
reported that it was commonplace for paediatricians
to continue seeing chronically ill adolescents well
into adulthood11; sadly, this remains the case at the
time of writing. In the 2010 study, the majority of
adolescents (85.3%) and parents (82.5%) were willing
to be transferred to adult care; however, fewer than
10% had received any transitional information.11
It is evident that the main obstacle to a successful
transition is the lack of a structured transitional care
programme and healthcare system, not resistance of
patients and families.23
The outcomes of adult PICU patients are
often overlooked in paediatric clinical studies,
and there have been no local data or reports on
adults admitted to a PICU. In a large report of such
patients in the United States, patients aged 21 to 29 years had two-fold greater odds of PICU mortality
compared with adolescent patients, after adjusting
for Paediatric Index of Mortality score, sex, trauma,
and having a complex chronic condition. Being aged
≥30 years was associated with a 3.5-fold greater
odds of mortality.17 It is difficult to draw a general
conclusion on whether a PICU or an adult intensive
care unit can provide the best critical care for this
group of patients. Paediatricians are more familiar
with some childhood-onset chronic conditions than
adult physicians; however, paediatricians may not
have the expertise to optimise the care of adult-acquired
conditions. Therefore, some investigators
have suggested that PICUs should have plans and
protocols specifically focused on this group of adult
patients.17
Transitional care programmes should be
tailored to the specific medical condition to ensure
optimal care and outcomes. Adult congenital heart disease or cystic fibrosis, for example, are obvious
candidates for the establishment of centralised,
disease-specific services that would bring together
specific paediatric and adult expertise for small and
complex patient cohorts.24 25 Other more common
conditions such as cerebral palsy, asthma or type 1
diabetes will benefit from a broader framework that
can guide clinicians and patients through a successful
transition from paediatric to adult care in a variety
of healthcare settings. A successful transitional
programme should include the following factors:
(1) a structured and written policy; (2) patient and
family involvement in preparation and planning;
(3) adequate training for staff and sensitisation to
the needs of adolescent patients; (4) continuity of
care to adult service (eg, paediatricians and adult
physicians should develop and implement joint
recommendations on diagnosis and treatment); and
(5) financial support for special healthcare service
needs.1 In addition to transitional care for chronic
medical conditions, psychiatric disorders, including
attention deficit hyperactivity disorder or autism,
should also be addressed. Developing transitional
care programmes for adolescents is an important
healthcare policy, as it can improve adherence
to healthcare services, long-term outcomes for
the patient, and better utilisation of healthcare
resources.12
As survival rates improve for chronic childhood
conditions, it is inevitable that some adults with
rare childhood conditions, especially those with
congenital heart disease, might be admitted
to a PICU. The PICUs should have protocols,
infrastructures, and transition pathways specifically
focusing on this unique group of adults, who are
‘too old’ to be a paediatric patient, but might not be
best treated in an adult intensive care unit.17 From
initiating collaboration with adult physicians to
developing a structured transitional care programme
covering both in-patient and out-patient services,
paediatricians are ultimately responsible for the
clinical care and long-term outcomes of this group
of adult patients, so that they are not overlooked by
our healthcare system. This process should be an
integral practice of humanism, humanistic medicine,
and humanitarianism. The modern PICU may take
on an additional role as a ‘Progressive Integrative
Care Unit’.
Author contributions
All authors contributed to the concept or design of the study, acquisition of the data, analysis or interpretation of the
data, drafting of the manuscript, and critical revision of the
manuscript for important intellectual content.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, KL Hon was not involved in the peer review process. Other authors have disclosed no conflicts
of interest. Other authors have no conflicts of interest to
disclose.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. Mazur A, Dembinski L, Schrier L, Hadjipanayis A,
Michaud PA. European Academy of Paediatric consensus
statement on successful transition from paediatric to adult
care for adolescents with chronic conditions. Acta Paediatr
2017;106:1354-7. Crossref
2. Zankl A, Duncan EL, Leo PJ, et al. Multicentric carpotarsal
osteolysis is caused by mutations clustering in the amino-terminal
transcriptional activation domain of MAFB. Am J
Hum Genet 2012;90:494-501. Crossref
3. Lau KK. Transition care in Hong Kong. Hong Kong Med J 2016;22:408-9. Crossref
4. Blum RW, Garell D, Hodgman CH, et al. Transition from
child-centered to adult health-care systems for adolescents
with chronic conditions. A position paper of the Society
for Adolescent Medicine. J Adolesc Health 1993;14:570-6. Crossref
5. van Staa AL, Jedeloo S, van Meeteren J, Latour JM. Crossing
the transition chasm: experiences and recommendations
for improving transitional care of young adults, parents
and providers. Child Care Health Dev 2011;37:821-32. Crossref
6. Fair C, Cuttance J, Sharma N, et al. International and
interdisciplinary identification of health care transition
outcomes. JAMA Pediatr 2016;170:205-11. Crossref
7. Rosen DS, Blum RW, Britto M, Sawyer SM, Siegel DM,
Society for Adolescent Medicine. Transition to adult
health care for adolescents and young adults with chronic
conditions: position paper of the Society for Adolescent
Medicine. J Adolesc Health 2003;33:309-11. Crossref
8. McDonagh JE, Kelly DA. Transitioning care of the pediatric recipient to adult caregivers. Pediatr Clin North
Am 2003;50:1561-83. Crossref
9. Jin YT, Chen CM, Chien WC. Factors influencing
transitional care from adolescents to young adults with
cancer in Taiwan: a population-based study. BMC Pediatr
2016;16:122. Crossref
10. Reiss J, Gibson R. Health care transition: destinations
unknown. Pediatrics 2002;110:1307-14. Crossref
11. Wong LH, Chan FW, Wong FY, et al. Transition care for
adolescents and families with chronic illnesses. J Adolesc
Health 2010;47:540-6. Crossref
12. Gabriel P, McManus M, Rogers K, White P. Outcome
evidence for structured pediatric to adult health care
transition interventions: a systematic review. J Pediatr
2017;188:263-9.e15. Crossref
13. Bell SC, Mall MA, Gutierrez H, et al. The future of cystic
fibrosis care: a global perspective. Lancet Respir Med
2020;8:65-124. Crossref
14. Iyengar AJ, Winlaw DS, Galati JC, et al. The Australia and
New Zealand Fontan Registry: description and initial
results from the first population-based Fontan registry.
Intern Med J 2014;44:148-55. Crossref
15. Pin TW, Chan WL, Chan CL, et al. Clinical transition for adolescents with developmental disabilities in Hong Kong: a pilot study. Hong Kong Med J 2016;22:445-53. Crossref
16. National Institute for Health and Care Excellence, UK
Government. Transition from children’s to adults’ services
for young people using health or social care services. NICE
guideline [NG43]. 2016. Available from: https://www.nice.org.uk/guidance/ng43. Accessed 27 Aug 2020.
17. Edwards JD, Houtrow AJ, Vasilevskis EE, Dudley RA, Okumura MJ. Multi-institutional profile of adults
admitted to pediatric intensive care units. JAMA Pediatr
2013;167:436-43. Crossref
18. McManus M, White P, Schmidt A, et al. Health care gap affects 20% of United States population: transition
from pediatric to adult health care. Health Policy OPEN
2020;1:100007. Crossref
19. White PH, Cooley WC, Transitions Clinical Report
Authoring Group, American Academy of Pediatrics,
American Academy of Family Physicians, American
College of Physicians. Supporting the health care transition
from adolescence to adulthood in the medical home.
Pediatrics 2018;142:e20182587. Crossref
20. gotransition.org. Overview: transitioning youth to an adult
health care clinician. 2020. Available from: https://www.gottransition.org/6ce/?leaving-full-package. Accessed 27
Aug 2020.
21. The Royal Australasian College of Physicians. Transition
of young people with complex and chronic disability needs
from paediatric to adult health services. 2014. Available from:
https://www.racp.edu.au/docs/default-source/advocacy-library/transition-of-young-people-with-complex-and-chronic-disability-needs.pdf. Accessed 27 Aug 2020.
22. Agency for Clinical Innovation, Australia Government. Key
principles for transition of young people from paediatric
to adult health care. 2014. Available from: https://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0011/251696/Key_Principles_for_Transition.pdf. Accessed 27 Aug 2020.
23. Scal P, Evans T, Blozis S, Okinow N, Blum R. Trends in transition from pediatric to adult health care services for
young adults with chronic conditions. J Adolesc Health
1999;24:259-64. Crossref
24. Bassareo PP, Mcmahon CJ, Prendiville T, et al. Planning
transition of care for adolescents affected by congenital
heart disease: the Irish national pathway. Pediatr Cardiol
2022 Jun 23. Epub ahead of print. Crossref
25. Office D, Heeres I. Transition from paediatric to adult care in cystic fibrosis. Breathe (Sheff) 2022;18:210157. Crossref