Hong Kong Med J 2022 Dec;28(6):496.e1–2
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Depicting multiple schwannomas—a tale of two
magnetic resonance neurogram techniques
HS Leung, MB, BS, FRCR1; JM Abrigo, FRCR, MD1; Eric HL Lau, FHKCORL, FHKAM (ORL)2; Winnie CW Chu, FHKCR, MD1
1 Department of Imaging and Interventional Radiology, The Chinese University of Hong Kong, Hong Kong
2 Department of Otorhinolaryngology, Head and Neck Surgery, The Chinese University of Hong Kong, Hong Kong
Corresponding author: Dr HS Leung (lhs655@ha.org.hk)
A 40-year-old female with unremarkable past health
and no known family history of neurofibromatosis
presented with a 3-year history of non-specific
discomfort at the right submandibular region
and upper neck. No facial nerve dysfunction was
evident clinically. Ultrasound of the major salivary
glands revealed a soft tissue nodule posterior
to the right submandibular gland. Fine needle
aspiration cytology findings were compatible with
schwannoma. Subsequent magnetic resonance
imaging (MRI) revealed a cluster of nodules within
the deep lobe of the right parotid gland with a linear
orientation. Further delineation with high-resolution
MRI and neurography sequences with acquisition of
double-echo steady state (DESS) [Fig 1] and post-contrast
constructive interference in steady state
(CISS) [Fig 2] sequences delineated these nodules
arising eccentrically from the main trunk, inferior division and the marginal mandibular branch of
the facial nerve, respectively. The patient continues
with imaging surveillance while awaiting workup of
underlying neurofibromatosis or schwannomatosis.
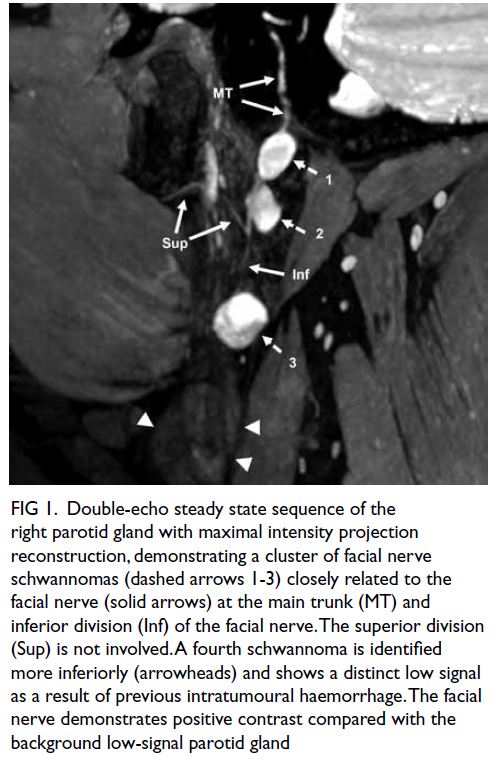
Figure 1. Double-echo steady state sequence of the right parotid gland with maximal intensity projection reconstruction, demonstrating a cluster of facial nerve schwannomas (dashed arrows 1-3) closely related to the facial nerve (solid arrows) at the main trunk (MT) and inferior division (Inf) of the facial nerve. The superior division (Sup) is not involved. A fourth schwannoma is identified more inferiorly (arrowheads) and shows a distinct low signal as a result of previous intratumoural haemorrhage. The facial nerve demonstrates positive contrast compared with the background low-signal parotid gland
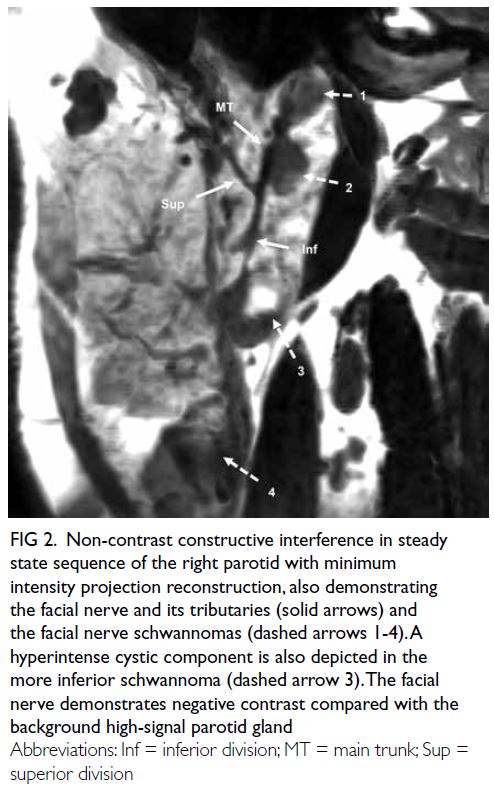
Figure 2. Non-contrast constructive interference in steady state sequence of the right parotid with minimum intensity projection reconstruction, also demonstrating the facial nerve and its tributaries (solid arrows) and the facial nerve schwannomas (dashed arrows 1-4). A hyperintense cystic component is also depicted in the more inferior schwannoma (dashed arrow 3). The facial nerve demonstrates negative contrast compared with the background high-signal parotid gland
In the early era of MRI imaging, depiction of the
extracranial intraparotid portion of the facial nerve
was difficult, if not impossible, with conventional
sequences. With advances in technology, higher
resolution and newer imaging protocols allow clear
delineation of intraparotid facial nerves. The use of
high-resolution, three-dimensional and gradient
echo–based techniques such as DESS1 and CISS2
allows clear delineation of the facial nerve from the
parotid parenchyma and any adjacent facial nerve
tumours, with a reasonable acquisition time of
around 5 minutes. Both sequences have been proven
useful in depicting the facial nerve and its branches,1 2
although there has not been any direct comparison of the efficacy of these sequences in facial nerve
depiction. Nonetheless these two sequences are
synergistic in the delineation of the facial nerve
tributaries due to their differences in contrast
characteristics. For DESS sequence, the facial nerve
demonstrates positive contrast compared with the
low-signal parotid gland; while in CISS, the facial
nerve shows negative contrast compared with
the high-signal parotid gland that is accentuated
after contrast injection. The use of reconstruction
techniques such as maximal intensity projection for
DESS, or minimum intensity projection for CISS,
can further improve visualisation of the peripheral
nerve branches.
Dedicated magnetic resonance neurogram
sequence for facial nerves is especially important in
patients with salivary gland neoplasms, since facial
nerve injury and consequent facial nerve weakness
remain an important postoperative complication,3
and prior understanding of facial nerve anatomy
is potentially helpful in reducing its incidence. It is
also useful in predicting histology of nerve sheath
tumours since schwannomas, as in our case, typically
arise eccentrically from a nerve with displacement of
its fascicles.4 Furthermore, such techniques can be
applied to other extracranial nerves5 in the diagnosis
of cranial neuropathies or in interventional planning
for tumours in the head and neck region. Gradient
echo–based DESS and CISS sequences partially
overcome the problem of long acquisition time in
conventional spin echo–based magnetic resonance
neurogram; nonetheless images can be significantly
compromised by susceptibility artefacts if adjacent
implants are present. The latter remains a major
obstacle that needs to be addressed.
Author contributions
Concept or design: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: HS Leung, JM Abrigo.
Drafting of the manuscript: HS Leung.
Critical revision of the manuscript for important intellectual content: JM Abrigo, EHL Lau, WCW Chu.
Acquisition of data: All authors.
Analysis or interpretation of data: HS Leung, JM Abrigo.
Drafting of the manuscript: HS Leung.
Critical revision of the manuscript for important intellectual content: JM Abrigo, EHL Lau, WCW Chu.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors would like to acknowledge Mr Chi-kin Wong and Mr Chung-yee Cheung, radiographers of Gerald Choa
Neuroscience Centre for their assistance in MRI scanning and
devising MRI protocols.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Ethics approval has been obtained from the Joint Chinese University of Hong Kong–New Territories East Cluster
Clinical Research Ethics Committee (CREC Ref No.:
2021.639). Patient consent for publication was obtained.
References
1. Kim Y, Jeong HS, Kim HJ, Seong M, Kim Y, Kim ST.
Three-dimensional double-echo steady-state with water
excitation magnetic resonance imaging to localize the
intraparotid facial nerve in patients with deep-seated
parotid tumors. Neuroradiology 2021;63:731-9. Crossref
2. Guenette JP, Ben-Shlomo N, Jayender J, et al. MR imaging
of the extracranial facial nerve with the CISS sequence.
AJNR Am J Neuroradiol 2019;40:1954-9. Crossref
3. Jin H, Kim BY, Kim H, et al. Incidence of postoperative
facial weakness in parotid tumor surgery: a tumor subsite
analysis of 794 parotidectomies. BMC Surg 2019;19:199. Crossref
4. Soldatos T, Fisher S, Karri S, Ramzi A, Sharma R, Chhabra A. Advanced MR imaging of peripheral nerve sheath tumors
including diffusion imaging. Semin Musculoskelet Radiol
2015;19:179-90. Crossref
5. Chhabra A, Bajaj G, Wadhwa V, et al. MR neurographic evaluation of facial and neck pain: normal and abnormal
craniospinal nerves below the skull base. Radiographics
2018;38:1498-513. Crossref

