© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Abscess formation following accidental ingestion
of fish bone with migration to the submandibular gland: a case report
Alan TL Lau, MB, ChB1; Raymond KY Tsang, MS, FHKAM (Otorhinolaryngology)2; Nikie HY Sun, MB, ChB3
1 Department of Otorhinolaryngology, Queen Mary Hospital, Hong Kong
2 Department of Surgery, The University of Hong Kong, Hong Kong
3 Department of Otorhinolaryngology, Queen Mary Hospital, Hong Kong
Corresponding author: Dr Alan TL Lau (ltl194@ha.org.hk)
Introduction
Deep neck space infection is associated with
significant morbidity and mortality, with the
submandibular space being a common site of
infection. Causes include odontogenic infections,
submandibular sialadenitis, lymphadenitis, trauma,
or surgery. This case report describes an uncommon
cause of fish bone migration to the submandibular
gland with consequent abscess formation. Apart
from fish bones, a variety of foreign bodies in salivary
glands has been described in previous case reports,
including toothbrush bristles, slivers of fingernails,
wood splinters, hairs or blades of grass.1
Case report
A 38-year-old woman with good past health
accidentally ingested a fish bone in September 2020.
She subsequently developed a sore throat, right
neck pain and swelling. She attended the emergency
department at Queen Mary Hospital 2 days later due
to progressive symptoms. On admission, she had a
fever of 38.1°C with blood pressure 161/80 mm Hg
and pulse 113 beats per minute. Physical examination revealed a palpable tender right upper neck swelling.
The right floor of mouth was oedematous and tender
on palpation. At the opening of the Wharton’s
duct, no foreign body was palpable, and no pus was
evident. Flexible laryngoscopy of the pharynx and
larynx was normal. An urgent computer tomography
with contrast revealed a 14-mm linear foreign body
at the right submandibular gland with surrounding
right submandibular abscess (Fig 1).
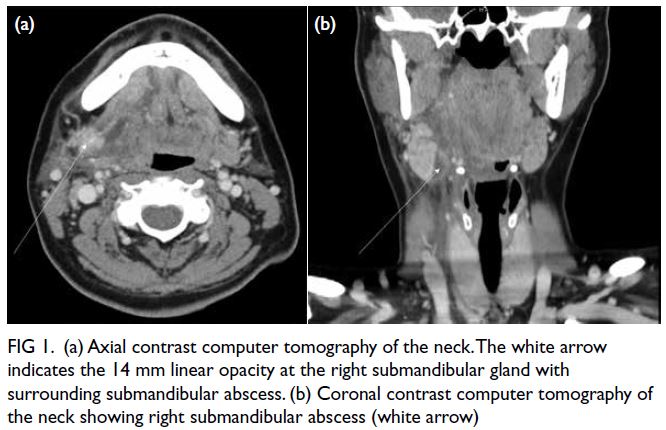
Figure 1. (a) Axial contrast computer tomography of the neck. The white arrow indicates the 14 mm linear opacity at the right submandibular gland with surrounding submandibular abscess. (b) Coronal contrast computer tomography of the neck showing right submandibular abscess (white arrow)
Emergency exploration under general
anaesthesia was performed. First, transoral
exploration was performed through an incision at
the right posterolateral floor of mouth to retrieve the
foreign body and drain the pus. In view of negative
transoral exploration, transcervical exploration
was performed. An abscess cavity was revealed
at the medial surface of the right submandibular
gland and pus was drained. Right submandibular
sialoadenectomy was performed and subsequently a
14-mm fish bone was found impacted at the medial
surface of the right submandibular gland (Fig 2). A
15Fr silicon drain was inserted to the wound bed.
The patient was monitored in the intensive care unit
postoperatively and was extubated the day following
surgery. Intravenous amoxicillin-clavulanate
(1.2 grams every 8 hours) was prescribed. Culture of
pus was negative. Fever and neck swelling subsided
and the drain was removed on postoperative day
3. The patient was discharged on postoperative
day 5 with diet well tolerated. At 2-week follow-up,
the neck and oral wound were well healed. The
hypoglossal nerve, lingual nerve and facial nerve
function was intact.

Figure 2. Specimen of right submandibular gland and fish bone. The length of the fish bone was 14 mm
Discussion
A fish bone can usually be retrieved easily via
endoscopy when lodged in the oral cavity, pharynx,
or oesophagus. Nonetheless, some patients with a
negative endoscopic finding may present later with
neck swelling and fever that may indicate a deep
neck space infection or migration of the foreign
body to the neck. Extraluminal migration of foreign vein, subcutaneous neck, the thyroid gland, and the
cervical spine has been reported in previous case
reports.2
Migration of fish bone to the submandibular
gland is uncommon. There have been two hypotheses
for such an event: direct trauma and retrograde
migration. Some theories suggest that continuous
flow of saliva from ducts into the oral cavity, the
duct orifice being mobile and able to twist in all
directions, and small diameter of duct at the orifice
render retrograde migration rare.1 In a previous
study of sialoendoscopic assessment of patients with
suspected obstruction in the ductal system of salivary
glands, 3.9% had sialoliths related to fish bone, with
the left submandibular gland being the dominant
site (92.3%). Compared with the submandibular
gland, foreign body at the parotid glands is much less
common.3
Foreign body at the submandibular gland can
have a variety of consequences. A patient with acute
right submandibular sialadenitis due to an impacted
fish bone has been reported who presented with
tender submandibular swelling.4 The patient had no
recall of foreign body ingestion. Plain radiograph of
the neck revealed a radiopaque foreign body. The
infection eventually required antibiotic treatment
and submandibular gland excision, with identification
of a fish bone at the excised gland. Another patient
presented with chronic sialadenitis. A fish bone–induced sialolith was successfully removed with
sialoendoscopy.5 A third patient presented with deep
neck space infection with abscess formation, as in
our patient.
Different techniques have been applied to
remove foreign body from the submandibular
gland.6 For sialoendoscopy, a higher success rate
has been observed with foreign bodies in the distal
duct while those located in the more proximal part
and secondary branches of the Wharton’s duct have been difficult to remove. Surgery may be required if
endoscopic treatment is not suitable, either using a
transoral approach or transcervical approach with
submandibular gland sialadenectomy. In this case
report, a transcervical approach was eventually
adopted.
Conclusion
The mainstay of treatment for submandibular abscess
is airway protection, antibiotic treatment, and
surgical drainage. Timely diagnosis and treatment
are key to success. Despite being a rare cause,
submandibular gland foreign body complicated
by abscess formation should be considered as a
differential diagnosis in patients with submandibular
swelling who report swallowing of a fish bone.
Author contributions
Concept or design: RKY Tsang.
Acquisition of data: NHY Sun.
Analysis or interpretation of data: ATL Lau.
Drafting of the manuscript: ATL Lau.
Critical revision of the manuscript for important intellectual content: RKY Tsang.
Acquisition of data: NHY Sun.
Analysis or interpretation of data: ATL Lau.
Drafting of the manuscript: ATL Lau.
Critical revision of the manuscript for important intellectual content: RKY Tsang.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
Dr Joseph CK Chung and Dr Sylvia SY Yu have made a
substantial contribution in terms of academic advice to the
publication of this case report.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The study was conducted in accordance with guidelines of the Hong Kong West Cluster Research Ethics Committee (IRB
Ref No.: UW21-094). Informed consent was obtained from the patient.
References
1. Su YX, Lao XM, Zheng GS, Liang, LZ, Huang XH, Liao GQ.
Sialoendoscopic management of submandibular gland
obstruction caused by intraglandular foreign body. Oral
Surg Oral Med Oral Pathol Oral Radiol 2012;114:e17-21. Crossref
2. Hsu CL, Chen CW. A prolonged buried fish bone mimicking Ludwig angina. Am J Otolaryngol 2011;32:75-6. Crossref
3. Xie L, Zheng L, Yu C, et al. Foreign body induced sialolithiasis treated by sialoendoscopic intervention. J
Craniofac Surg 2014;25:1372-5. Crossref
4. Riccio FJ, Scavo VJ. Unusual foreign body etiology of sialadenitis. Arch Otolaryngol 1967;86:210-2. Crossref
5. Iwai T, Sugiyama S, Hayashi Y, et al. Sialendoscopic removal of fish bone-induced sialoliths in the duct of the submandibular gland. Auris Nasus Larynx 2018;45:343-5. Crossref
6. Li P, Zhu H, Huang D. Detection of a metallic foreign body in the Wharton duct: a case report. Medicine (Baltimore) 2018;97:e12939. Crossref

