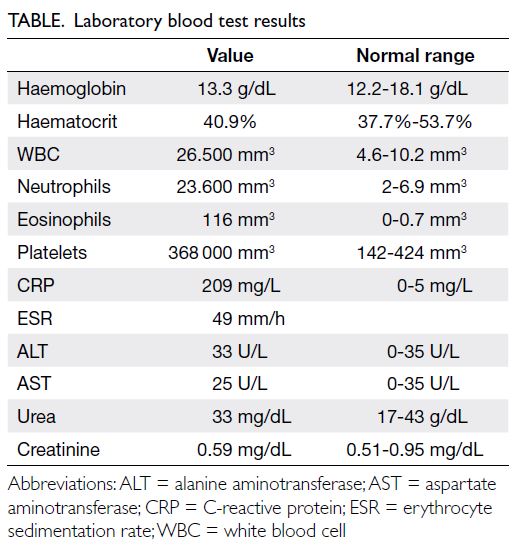
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
A rather difficult case of acute generalised
exanthematous pustulosis: would colchicine be a
treatment option?
Rabia Oztas Kara, MD; Bahar Sevimli Dikicier, MD; Mahizer Yaldiz, MD; Hande Tekmenler, MD
Department of Dermatology, Sakarya University Faculty of Medicine, Sakarya, Turkey
Corresponding author: Dr Rabia Oztas Kara (r.oztas.kara@gmail.com)
Case report
A 24-year-old lactating female patient presented
with redness, burning, and rash on the face and
body on the fifth day of hydroxychloroquine (HCQ)
treatment, prescribed after diagnosis of coronavirus
disease 2019 infection. Physical examination
revealed numerous non-follicular pustular lesions on
an erythematous background that started on the face
and neck and extended to the whole body, especially
in the folds and extremities, and in the palmoplantar
regions (Fig 1a). Conjunctival involvement was also
evident. Examination was otherwise unremarkable
and the patient was afebrile.

Figure 1. (a) Numerous non-follicular pustules on an erythematous base on the leg. (b) Non-follicular pustules recurring in areas of desquamation. (c) Complete recovery after desquamation
Laboratory examinations were likewise
unremarkable (Table). Histopathological examination
of punch biopsy of the leg lesions, subcorneal
pustule formation in the epidermis, oedema in the
papillary dermis, and lymphocytic infiltration in
the upper dermis was performed (Fig 2). There was
no individual or family history of psoriasis, and the
patient denied taking any medication except HCQ in the last 3 months. Based on these findings, the patient
was diagnosed with HCQ-induced (acute generalised
exanthematous pustulosis [AGEP]). Intravenous
methylprednisolone 60 mg/day, etodolac, topical
methylprednisolone, and moisturiser were
prescribed. An initial partial response was achieved
but on the 15th day of treatment, pustular lesions,
itching, and complaints of burning recurred and the
patient developed a fever of 38°C (Fig 1b). Blood
cultures grew Staphylococcus aureus, sensitive to
ciprofloxacin. Systemic ciprofloxacin 750 mg twice
a day (1500 mg daily) was started with the addition
of 0.5 mg colchicine thrice a day (1.5 mg daily). Her
general condition improved and the skin lesions
completely regressed with desquamation (Fig 1c).
Systemic methylprednisolone treatment was tapered
and stopped. Colchicine treatment was continued
for 1 month and the dose then decreased to 0.5 mg
twice a day for a further month before being stopped.
The patient continues to attend for follow-up and
remains well. A patch test for HCQ is planned when
lactation stops.
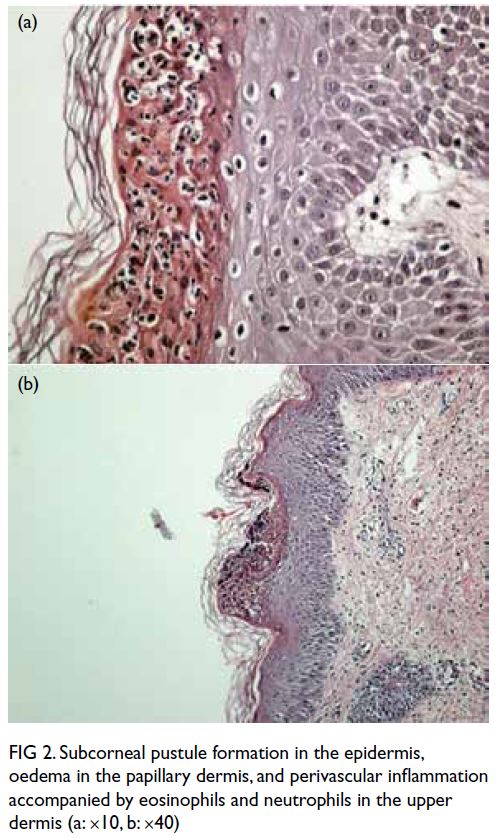
Figure 2. Subcorneal pustule formation in the epidermis, oedema in the papillary dermis, and perivascular inflammation accompanied by eosinophils and neutrophils in the upper dermis (a: ×10, b: ×40)
Discussion
Drugs constitute 90% of the aetiology of AGEP. The
remaining 10% are due to infection. Although the
pathogenesis of AGEP is not fully understood, the
accumulation of cytokines released by helper T cells
and drug-induced antigen-antibody complexes in
the skin is blamed.1
The cutaneous side-effects of
hydroxychloroquine include AGEP, urticaria,
pruritus, xerosis, maculopapular rash, psoriasis,
erythroderma, Stevens–Johnson syndrome, hair
loss, and hair whitening.2 Since hydroxychloroquine
is a weak base with a long half-life, it passes into
breast milk in minimal amounts.
In previously reported cases of HCQ-induced
AGEP, the duration of exposure to HCQ was
reported to be 2 to 30 days prior to symptom onset3
and time to recovery after stopping HCQ has been
reported to be 7 to 81 days.4 The long persistence of
symptoms can be explained by the long half-life of
HCQ, approximately 40 to 50 days.5
Acute generalised exanthematous pustulosis
cases due to HCQ have been reported during the
pandemic. The typical features of these cases are
a more prolonged course and a need for systemic
steroid treatment. In this patient, colchicine was
started because a complete response was not
obtained with systemic corticosteroid treatment.
Colchicine suppresses inflammation at many
stages. It has an antimitotic impact by binding to
tubulin, preventing its polymerisation into new
microtubules, inhibits neutrophil chemotaxis,
and reduces free oxygen radical production by
neutrophils. It is more useful in the treatment of neutrophilic dermatoses such as pustular conditions
with predominant neutrophilic infiltrates, eg,
pustular psoriasis. For this reason and the lack of
response to systemic corticosteroid treatment,
colchicine was added to our patient’s treatment
regimen.
We conclude that colchicine may be a
treatment option for AGEP, a rare side-effect of
HCQ, especially when it is resistant to systemic
corticosteroid. It can also be used as an effective
treatment during lactation due to its better safety
profile.
Author contributions
Concept or design: All authors.
Acquisition of data: R Oztas Kara, H Tekmenler.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: R Oztas Kara, H Tekmenler.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: R Oztas Kara, H Tekmenler.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: R Oztas Kara, H Tekmenler.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
The authors have no conflicts of interest to disclosure.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki. The patient provided informed consent for the
treatment/procedures and consent for publication.
References
1. Halevy S, Kardaun SH, Davidovici B, Wechsler J,
EuroSCAR and RegiSCAR Study Group. The spectrum
of histopathological features in acute generalized
exanthematous pustulosis: a study of 102 cases. Br J Dermatol 2010;163:1245-52. Crossref
2. Salido M, Joven B, D’cruz, DP, Khamashta MA, Hughes GR.
Increased cutaneous reactions to hydroxychloroquine
(Plaquenil) possibly associated with formulation change:
comment on the letter by Alarcón. Arthritis Rheum
2002;46:3392-6. Crossref
3. Liccioli G, Marrani E, Giani T, Simonini G, Barni S, Mori F.
The first pediatric case of acute generalized exanthematous
pustulosis caused by hydroxychloroquine. Pharmacology
2019;104:57-9. Crossref
4. Pearson KC, Morrell DS, Runge SR, Jolly P. Prolonged
pustular eruption from hydroxychloroquine: an unusual
case of acute generalized exanthematous pustulosis. Cutis
2016;97:212-6.
5. İslamoğlu ZG, Karabağli P. A case of recalcitrant acute
generalized exanthematous pustulosis with Sjogren’s
syndrome: successfully treated with low-dose cyclosporine.
Clin Case Rep 2019;7:1721-4. Crossref