Hong Kong Med J 2022;28(6):457–65 | Epub 7 Dec 2022
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE (HEALTHCARE IN MAINLAND CHINA)
Correlation between primary family caregiver
identity and maternal depression risk in poor rural China
N Wang, PhD; M Mu, MSc; Z Liu, MSc; Z Reheman, MSc; J Yang, PhD; W Nie, MSc; Y Shi, PhD; J Nie, PhD
Center for Experimental Economics in Education, Shaanxi Normal University, Xi’an, China
Corresponding author: Dr J Yang (jyang0716@163.com)
Abstract
Introduction: Prenatal and postpartum depression
are important public health challenges because
of their long-term adverse impacts on maternal
and neonatal health. This study investigated the
risk of maternal depression among pregnant and
postpartum women in poor rural China, along with
the correlation between primary family caregiver
identity and maternal depression risk.
Methods: Pregnant women and new mothers
were randomly selected from poor rural villages
in the Qinba Mountains area in Shaanxi. Basic
demographic information was collected regarding
the women and their primary family caregivers.
The Edinburgh Postnatal Depression Scale was used
to identify women at risk of depression, and the
Perceived Social Support Scale was used to evaluate
perceived family support.
Results: This study included 220 pregnant women and
473 new mothers. The mean proportions of women
at risk of prenatal and postpartum depression were
19.5% and 18.6%, respectively. Regression analysis
showed that identification of the baby’s grandmother
as the primary family caregiver was negatively
correlated with maternal depression risk (β=-0.979,
95% confidence interval [CI]=-1.946 to -0.012,
P=0.047). However, the husband’s involvement in that role was not significantly correlated with
maternal depression risk (β=-0.499, 95% CI=-1.579
to 0.581, P=0.363). Identification of the baby’s
grandmother as the primary family caregiver was
positively correlated with family support score
(β=0.967, 95% CI=-0.062 to 1.996, P=0.065).
Conclusion: Prenatal and postpartum depression
are prevalent in poor rural China. The involvement
of the baby’s grandmother as the primary family
caregiver may reduce maternal depression risk, but
the husband’s involvement in that role has no effect.
New knowledge added by this study
- Prenatal and postpartum depression are prevalent in poor rural areas of China. Despite evidence regarding the importance of family support during prenatal and postpartum periods, husbands in poor rural China did not provide effective support.
- There was a persistent risk of maternal depression during both prenatal and postpartum periods.
- Maternal depression persists in the absence of external interventions.
- High-quality family support is necessary to ensure that pregnant women maintain good mental health. Compared with husbands, grandmothers may be better primary caregivers because they are experienced in terms of parenting and housework.
- Husbands in poor rural China should receive training that enables them to provide effective maternal care.
Introduction
Maternal depression is a common mental health
problem during the prenatal and postpartum
periods. The World Health Organization estimates
that approximately 10% of pregnant women and
13% of postpartum women worldwide have mental health problems, mainly depression.1 In China, the
prevalence of maternal depression ranges from
8.2% to 28.5%.2 3 4 5 6 7 Women in urban areas have access
to specialised maternity care services and mental
health services that can help manage these mental
health problems and difficulties.8 However, these commercialised services are usually expensive and
distant from poor rural areas of China. Therefore, it is
particularly important for pregnant and postpartum
women in poor rural areas to rely on family and
social relationships for reasonable care and support.
There is evidence that the level of perceived
social support, particularly family support, is
associated with a woman’s mental health status
during pregnancy.9 10 China’s rapid societal and
economic development have resulted in substantial
changes to family structure in both urban and rural
areas. For example, modern couples are more likely
to live with only their children, rather than with
family members from multiple generations.11 When
grandparents are absent from a family’s daily life,
the role of the husband becomes more important
because he must be more engaged in housework12 and provide greater support.
The changes in primary family caregiver
identity during prenatal and postpartum periods
reflect this transformation of family structure.13 The
results of multiple studies in developed countries
and the urban areas of China have suggested that
husbands are able to care for their wives and children
during pregnancy and after delivery; moreover, a
husband’s companionship has a positive impact on
the mental health status of his pregnant wife.2 10 14 However, in poor rural areas, no consensus has been
reached concerning whether a husband can provide
effective family support for his pregnant wife.15 For
example, husbands usually have lower awareness
of maternity care because of limited education
and limited housework experience. However, in a
traditional Chinese family with patrilocal features,
the husband is the main worker and is responsible
for the economic well-being of the family,16 whereas
the wife stays at home and cares for the family. This
stereotype of traditional household arrangement
prevents some men from providing maternal care,
regardless of their presence at home. Accordingly,
grandmother, the mother of the baby’s mother,
becomes a possible caregiver for the mother and
baby,17 although this may lead to mother-in-law conflict.18
Here, using data from a large-scale survey
of pregnant and postpartum women in poor rural
areas, we analysed the status of maternal mental
health in poor rural areas, with family support as an
intermediate variable, to understand the correlation
between primary family caregiver identity and
maternal depression risk.
Methods
Sampling
The data analysed in this study were collected
during a survey of maternal and neonatal health
and nutrition statuses among residents of poor rural
villages in the Qinba Mountains area; the survey
was conducted by Shaanxi Normal University from
March 2019 to April 2019. The Qinba Mountains
area spans six provinces including Gansu, Sichuan,
Shaanxi, Chongqing, Henan, and Hubei. Its primary
portion is situated in Shaanxi’s southern region. In
2019, the per capita annual disposable income in the
Qinba Mountains area was RMB 11 443, similar to
that of rural residents in poverty-stricken counties
(RMB 11 567).19 In 2018, the mean poverty rate in
this area was 3.6%; for comparison, the national
mean was 1.7% and the rate in poverty-stricken
counties was 4.5%.20 This study included women aged
≥18 years who were either pregnant (≥4 weeks of
gestation) or in the postpartum period (0-6 months
after delivery).
The following multilevel cluster-based random
sampling method was used in this study. First, 13
national-level poor counties in two prefectures in
the Qinba Mountains area were selected. Then, a
list of villages was obtained for each county, and the
total numbers of pregnant women and households
with babies aged ≤6 months in each village were
counted with assistance from local government
officials. Considering the financial limitations and
overall feasibility of the study, villages with a small
sample size (<3) or large sample size (>15) were excluded. Finally, we used Stata 15.0 (Stata Corp,
College Station [TX], United States) to analyse the
data. The sample size was estimated to achieve, for
an average incidence of independent variables of
0.15 in consideration of our pilot study, a sampling
standard error (SE) of 0.03 with a 95% confidence
interval (CI). The final 131 villages were randomly
selected as sample villages, and all households in
the sample villages that met the above criteria were
considered eligible for the study.
Data collection
The data used in this study were collected through
face-to-face interviews. To ensure accuracy and
consistency during data collection, enumerators
were selected from a group of interested university
students in Xi’an. The enumerators underwent
extensive training, then completed a pilot study
with 20 participants prior to formal data collection.
Each eligible participant received a consent form
with information regarding programme objectives,
procedures, potential risks, and benefits, as well as
an explanation of privacy protection. Participants
provided oral consent for inclusion in the study
before engaging in a face-to-face interview with a
single enumerator. Each interview only involved
the participant, and interruptions from other family
members were avoided.
Assessments
Basic participant information
A questionnaire was used to collect basic participant
information, including their age, education level,
and self-rated health status, along with whether the
baby had been born and whether it was the firstborn
child. The women were also asked whether they had
access to any support groups where mothers could
seek help and exchange information concerning
parenting experiences. Furthermore, they were
asked nine yes/no questions regarding family assets
(eg, possession of a computer, an air conditioner, and
a car). The above questions were also included in our
questionnaire to better understand maternal social
interactions and household assets in order to control
for them in the regression analysis and thus produce
more accurate regression results. Each participant’s
decision-making power was measured using a
scale of eight items compiled by Peterman et al.21
A higher score on the decision-making power
scale was presumed to indicate greater autonomy
concerning childcare and the management of other
family issues.
Primary family caregivers
A questionnaire was used to collect information
about all family members living in the participant’s
home for >3 months, who were more likely to be the primary caregivers and to have an impact on
maternity. Each participant was asked to identify
the family member who served as the primary
family caregiver, providing the most care for the
participant and her baby during the prenatal and
postpartum periods. Considering the sample size
and sample distribution, three primary family
caregiver categories were used in this study: the
husband, the baby’s grandmother (the mother of the
baby's mother or the baby's father), and other family
members or no caregivers.
Edinburgh Postnatal Depression Scale
The Edinburgh Postnatal Depression Scale (EPDS)
is a 10-item scale used to identify women at risk of
maternal depression.22 23 The total EPDS score ranges
from 0 to 30, where a higher score indicates a greater
risk of depression. Although the original cut-off
value was an EPDS score of ≥13 points, we used the
standard cut-off value in China (≥9.5 points24 25) as
an indicator of sufficient depression risk to merit
psychiatric examination and possible treatment.
Previous research has demonstrated that the EPDS
has satisfactory reliability and validity. Specifically,
Wang et al26 reported that the EPDS had a content
validity ratio of 0.93 and good internal consistency
(Cronbach’s α coefficient of 0.76). The correlation
coefficients between the 10 individual item scores
and the total score ranged from 0.37 to 0.67, with P
values <0.01.
Perceived Social Support Scale
The Perceived Social Support Scale, developed by
Zimet et al27 and translated into Chinese by Jiang,28
is a 12-item self-assessment questionnaire that
measures three sources of social support (ie, three
subscales): family support, friends’ support, and
other people’s support. Responses to questionnaire
items are recorded using a seven-point Likert scale
that ranges from ‘completely negative’ to ‘completely
positive’ (1-7 points), indicating the respondent’s
level of agreement with each item. The total score
is 84 points (28 points per subscale), and a higher
score indicates the receipt of greater social support.
The Cronbach’s α coefficient of the scale is 0.88; the
Cronbach’s α coefficients for family support, friends’
support, and other people’s support subscales are
0.81, 0.85, and 0.91, respectively.27 Because this study
focused on family support, only the family support
subscale was used as an intermediate variable to
analyse the correlation between primary family
caregiver identity and maternal depression risk.
Statistical methods
STATA 15.1 software was used to clean the data and
perform statistical analysis. Descriptive statistical
analysis was performed and presented as mean ± standard deviation. F-test and t test were used
to detect differences in depression scores among
subgroups of women with different characteristics.
Multiple linear regression was used to explore
correlations between primary family caregiver
identity and maternal depression risk or family
support score. P values <0.05 were considered
statistically significant. Additionally, we adjusted the
SE at the village level and calculated coefficients with
greater precision because individual values within
the same village are correlated, which might result in
biased SE in multiple linear regression.
Results
In total, 715 women were interviewed, including 220
pregnant women and 495 new mothers. Twenty-two
samples with missing values were excluded to
ensure sample uniformity throughout the analysis
procedure. Finally, analyses in this study were based
on the data of 693 participants (220 pregnant women
and 473 new mothers) and the questionnaire return
efficiency was 96.9%, which is the percentage of
survey responses that were valid.
Maternal depression risk in poor rural areas
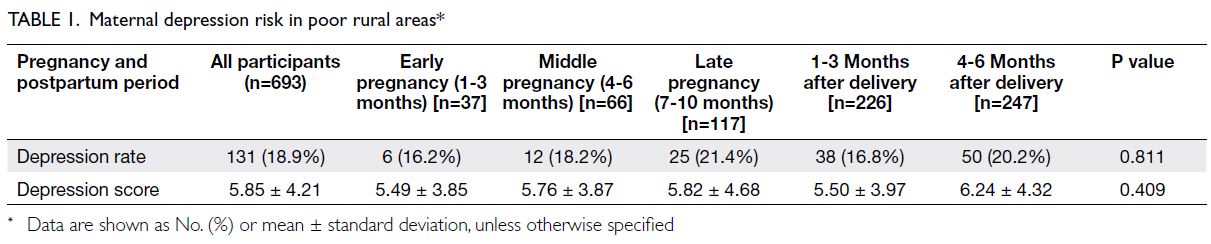
Among the 220 pregnant women, 37 (16.8%), 66
(30.0%), and 117 (53.2%) were in the early, middle,
and late stages of pregnancy, respectively (Table 1).
In total, 226 of the 473 new mothers (47.8%) had
babies aged 1 to 3 months, whereas 247 new mothers
(52.2%) had babies aged 4 to 6 months.
The mean maternal EPDS score was 5.85
and the proportion of women at risk of depression
was 18.9% (131/693). The proportion of women at
risk of depression was generally stable regardless
of pregnancy stage. Specifically, the proportion of
women at risk of depression during early pregnancy
was 16.2% (6/37); during middle and late pregnancy,
the proportions of women at risk were slightly
increased. The proportions of women at risk of
depression were 16.8% (38/226) and 20.2% (50/247)
at 1-3 months and 4-6 months after delivery,
respectively. However, the maternal EPDS scores
and proportions of women at risk of depression did
not significantly differ according to pregnancy stage
or time since delivery.
Univariate analysis of maternal depression
risk
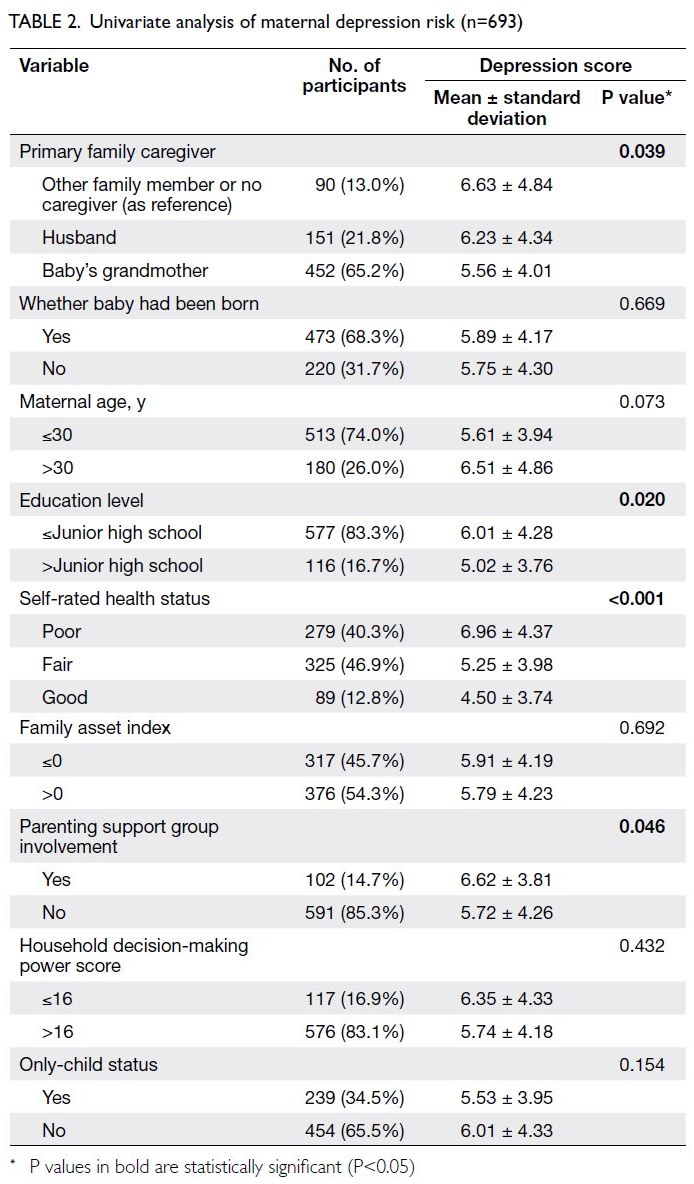
Overall, the mean participant age was 28.13 ± 4.70
years. In total, 239 women (34.5%; mean age, 25.52
± 3.95 years) reported that the current pregnancy
or ≤6-month-old baby was their firstborn child. The
remaining 454 women (65.5%; mean age, 29.50 ± 4.49
years) were experienced mothers who have already
had children and are familiar with caring for them.
Overall, 116 women (16.7%) had an education level
above junior high school. The self-rated health status
was good in 89 women (12.8%), and 102 women
(14.7%) were involved in a parenting support group.
Table 2 summarises the participant characteristics.
As shown in Table 2, the participants were
clustered into three groups according to primary
caregiver identity: the husband for 151 women
(21.8%), the baby’s grandmother for 452 women
(65.2%), and other family members or no caregiver
for 90 women (13.0%). The mean EPDS scores
of women in the three groups were 6.23 ± 4.34,
5.56 ± 4.01, and 6.63 ± 4.84, respectively (P=0.039).
Additionally, univariate analysis revealed statistically
significant differences in depression scores according
to education level, self-rated health status, and
parenting support group involvement. There were no
statistically significant differences in other variables.
Correlation between primary family
caregiver identity and maternal depression
risk
As shown in Table 3, identification of the baby’s
grandmother as the primary family caregiver was
significantly negatively correlated with EPDS score
(β=-0.979, 95% CI=-1.946 to -0.012, P=0.047).
However, identification of the husband as the family
caregiver was not significantly correlated with EPDS
score (β=-0.499, 95% CI=-1.579 to 0.581, P=0.363).
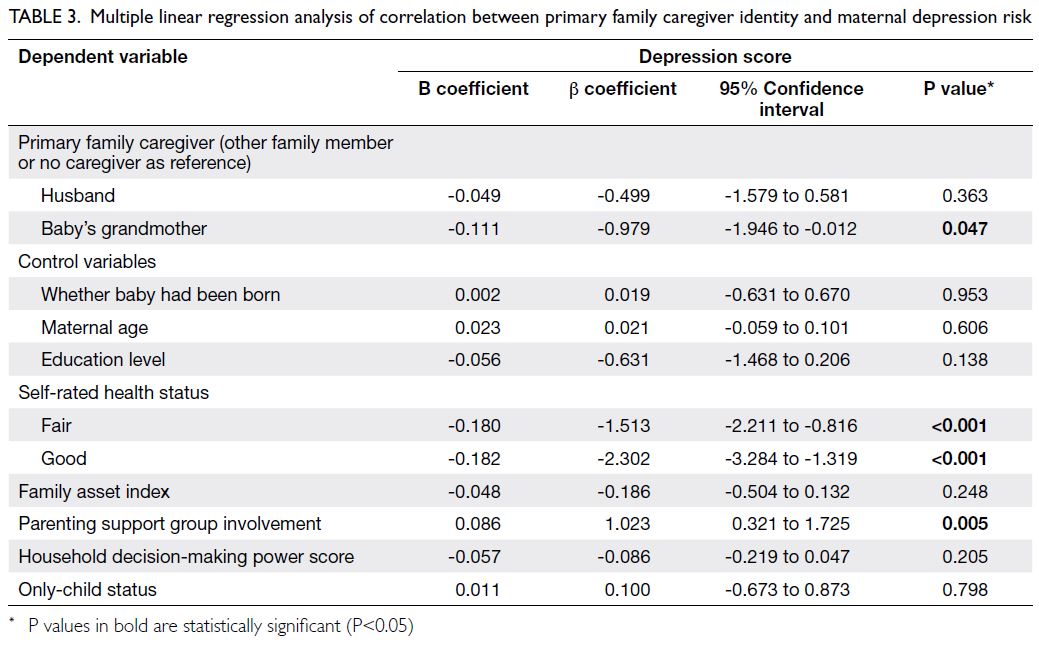
Table 3. Multiple linear regression analysis of correlation between primary family caregiver identity and maternal depression risk
Correlation between primary family
caregiver identity and family support score
As shown in Table 4, after adjustment for other
variables, there was no significant correlation between
identification of the husband as the primary family
caregiver and the family support score (β=0.375,
95% CI=-0.704 to 1.455, P=0.493). However, identification of the baby’s grandmother as the
primary family caregiver was significantly positively
correlated with family support score (β=0.967,
95% CI=-0.062 to 1.996, P=0.065). Furthermore,
identification of the baby’s grandmother as the
primary family caregiver had the largest standardised
regression coefficient among the three caregiver
categories, indicating that pregnant and postpartum
women felt the greatest family support when
the baby’s grandmother was the primary family
caregiver.
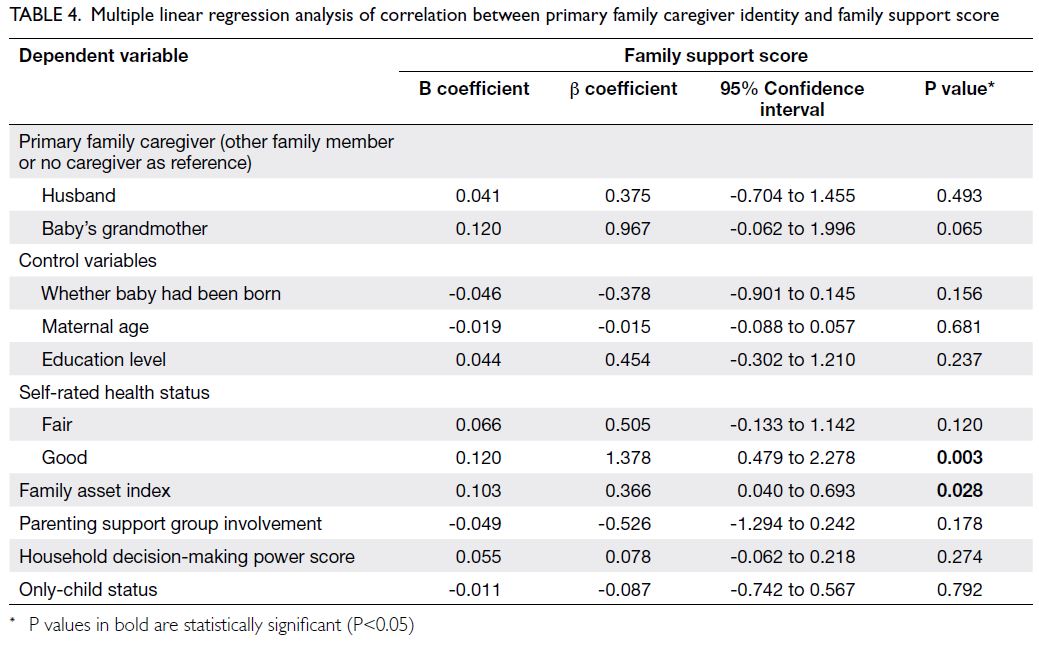
Table 4. Multiple linear regression analysis of correlation between primary family caregiver identity and family support score
Discussion
Maternal depression risk in poor rural areas
In this study, the overall proportion of women at
risk of maternal depression was 18.9%, including a
mean proportion of 19.5% among pregnant women
and a mean proportion of 18.6% among women
≤6 months postpartum. This overall proportion of
women at risk of maternal depression is much higher
than the proportion in a western urban area of China
(12.4%)29 and comparable with the proportions in
low- and middle-income countries such as Ethiopia
(19.9%)30—both previous studies also used the EPDS
to identify women at risk of maternal depression. The
high proportion in the present study may be related
to the location (poor rural areas): compared with
women in urban areas, women in poor rural areas are
more likely to have a lower socio-economic status.31
The lack of knowledge regarding mental health
and its services in rural areas also makes women
in such areas more likely to become depressed if
they do not receive timely treatment for mental
health problems.32 Therefore, the mental health
of rural mothers should receive greater attention
from their family members and the relevant health
departments.
This study also revealed a persistent risk of
depression during the prenatal and postpartum
periods (Table 1). Notably, the proportion did not
substantially decrease by 6 months after delivery.
Yue et al33 investigated the mental health of
caregivers for babies aged 6 to 36 months in a rural
area in western China. Their results showed that the
proportion of caregivers at risk of depression was
similar to the proportion in the present study. These
findings suggest that maternal depression persists
in the absence of external intervention. Thus, there
is an urgent need for timely external mental health
interventions among pregnant women and mothers
of young children. The present study also showed
that the maternal depression risk in poor rural areas
is influenced by factors such as a woman’s education
level, self-rated health status, and parenting support
group involvement. These results are consistent with
the findings by Zhou et al,7 Lancaster et al,10 and
Lee et al.18
Correlation between primary family
caregiver identity and maternal depression risk
Our results showed that identification of the
husband as the primary family caregiver was not
significantly correlated with maternal depression
risk in poor rural areas (Table 3). This finding
was considerably different from the results of
previous studies in urban areas. Xie et al34 found
that insufficient or poor-quality emotional support
from the husband was significantly associated with
an increased risk of postpartum depression among mothers in Changsha, Hunan Province, China. In
contrast, Wan et al2 found that the proportions of
women at risk of maternal depression were 1.9- to
2.6-fold higher among women without support from
the husband before and after delivery than among
women with support from the husband, based on
a study of mothers in Beijing, China. The results of these studies suggest that the husband’s involvement
as the primary family caregiver can reduce the risk
of maternal depression in urban areas, but this effect
was not apparent in poor rural areas.
We also found that maternal depression risk was
significantly lower when the baby’s grandmother was
identified as the primary family caregiver (Table 3). Our results are consistent with the findings by Wan
et al2 in a study of 342 pregnant women in Beijing,
China: during the ‘confinement’ period, care and
support from the baby’s grandmother(s) were
important for relieving depression. However, Lee
et al18 showed that mother-in-law conflict remains
prominent in China, which may have negative
emotional outcomes for grandmothers and new
mothers. Although pregnant and postpartum women
in poor rural areas may experience similar conflict,
our findings suggest that support from the baby’s
grandmother(s) remains predominantly positive.
Correlation between family support and
maternal depression risk
We attempted to determine why support from
the husband did not reduce maternal depression
risk in poor rural areas through the analysis of an
intermediary variable. Initially, we hypothesised
that the positive effect of the husband acting as the
primary family caregiver would be offset by the loss
of income caused by the husband’s inability to seek
work opportunities in other locations. However,
data analysis revealed that the husband’s role as
the primary caregiver had no impact on the family
income and family asset index (online supplementary Table 1). Thus, we explored the effect of family
support. Multiple previous studies demonstrated
that family support influenced maternal depression
risk14; consistent with those findings, our analysis
showed that family support was significantly
negatively correlated with maternal depression risk
(online supplementary Table 2).
There may be two main reasons for this
negative correlation. First, husbands in poor rural
areas have insufficient knowledge and skills related
to maternal care.16 Husbands do not have first-hand
experience in childbirth and can only acquire it
through education. However, compared with men
in urban areas, men in poor rural areas have lower
levels of education and may be less inclined to learn
on their own, making it more difficult to acquire such
knowledge and skills.35 In contrast, grandmothers are
more experienced overall, which may enable them to
provide more effective family support. For example,
based on their own experience, grandmothers can
help new mothers to prepare for and manage pain
that sometimes occurs during breastfeeding, which
can alleviate anxiety and provide a feeling of greater
support.17 Second, in poor rural areas, husbands
may lack sufficient time and energy to provide
effective family care. Compared with families in
urban areas, families in poor rural areas are more
economically disadvantaged33; therefore, husbands
in such families may prioritise financial stability and
be unable to expend time or energy in support of
maternal care, despite their physical presence in the
home. In contrast, the baby’s grandmother(s) may have sufficient time and energy to provide effective
maternal care (eg, by feeding the baby and changing
its diapers), thus relieving the mother’s psychological
stress.
The findings in this analysis of women in poor
rural areas differ from the results of studies in urban
areas, indicating important differences in family
structure between urban and rural areas. There is
evidence that a gradual transformation of the family
is underway in urban areas, whereby husbands have
begun to actively engage in caregiving. However, the
transformation of family structure is much slower
in poor rural areas,13 and husbands in those areas
are not yet prepared for this new role. Because of
constraints regarding their education level and
skills, as well as family finances, husbands in poor
rural areas continue to prioritise financial stability36;
their support does not have a positive impact on
the risk of maternal depression. Thus, women in
poor rural areas must continue to rely on family
members outside of the nuclear family, such as the
baby’s grandmother(s), to assume some caregiving
responsibilities.
Commercialised and specialised mental health
counselling services in urban areas play important
roles in improving maternal mental health.8 Xiao37
found that postnatal care through a menstrual club
provided continuous physical, psychological, and
emotional support that was sufficient to reduce the
incidence of postpartum depression. However, such
clubs are not available in poor rural areas. Therefore,
it is important to promote better caregiving from
family members, including husbands. For example,
husbands could receive training that enables them
to provide practical support, as well as guidance
concerning the early identification of depressive
tendencies and the development of communication
skills for psychological adjustment.
Limitations
This study had some limitations. First, its cross-sectional design prevented the assessment of
maternal depression trends during pregnancy and
after delivery, although such an assessment could
have been conducted in a cohort study. Second, this
study focused on primary family caregiver identity
and did not explore the type or form of caregiving
provided. Third, all participants were residents of
rural northwest China, and thus the results may
not be generalisable to other populations. These
limitations should be addressed in future studies.
Conclusions and policy implications
The prevalence of maternal depression is high in poor rural areas of Shaanxi Province. Identification of the
husband as the family caregiver was not significantly correlated with maternal depression risk, whereas
the involvement of the baby’s grandmother in that
role was significantly negatively correlated with
maternal depression risk. Based on our findings,
we make the following suggestions. In rural areas,
high-quality family support is necessary to ensure
that pregnant women maintain good mental health.
Compared with husbands, grandmothers may be
better primary caregivers because they are more
experienced in terms of parenting and housework.
Husbands in poor rural China should receive training
that enables them to provide effective maternal care.
Author contributions
Concept or design: N Wang, M Mu, J Yang, Y Shi, J Nie.
Acquisition of data: N Wang, M Mu, Z Liu, R Zulihumaer, W Nie.
Analysis or interpretation of data: N Wang, M Mu, J Yang, J Nie.
Drafting of the manuscript: N Wang, M Mu, J Yang, Y Shi, J Nie.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: N Wang, M Mu, Z Liu, R Zulihumaer, W Nie.
Analysis or interpretation of data: N Wang, M Mu, J Yang, J Nie.
Drafting of the manuscript: N Wang, M Mu, J Yang, Y Shi, J Nie.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
As an International Editorial Advisory Board member of the journal, Y Shi was not involved in the peer review process.
Other authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank the study participants and the enumerators who conducted data collection.
Funding/support
The authors are supported by the 111 Project (Grant No. B16031), Soft Science Research Project of Xi’an Science and
Technology Plan (Grant No. 2021-0059), the Fundamental
Research Funds for the Central Universities (Grant No.
2021CSWY024) and the Fundamental Research Funds for the
Central Universities (Grant No. 2021CSWY025) of China.
Ethics approval
The study was approved by the Medical Ethics Committee
of Shaanxi Normal University and Xi’an Jiaotong University
of China (No: 2020-1240). Each eligible participant received
a consent form with information regarding programme
objectives, procedures, potential risks, and benefits, as well
as an explanation of privacy protection. Participants provided
oral consent for inclusion in the study before engaging in a
face-to-face interview with a single enumerator.
References
1. Ceulemans M, Foulon V, Ngo E, et al. Mental health status
of pregnant and breastfeeding women during the COVID-
19 pandemic—a multinational cross-sectional study. Acta
Obstet Gynecol Scand 2021;100:1219-29. Crossref
2. Wan EY, Moyer CA, Harlow SD, Fan Z, Jie Y, Yang H.
Postpartum depression and traditional postpartum care in
China: role of Zuoyuezi. Int J Gynecol Obstet 2009;104:209-13. Crossref
3. Zeng Y, Cui Y, Li J. Prevalence and predictors of antenatal
depressive symptoms among Chinese women in their
third trimester: a cross-sectional survey. BMC Psychiatry
2015;15:66. Crossref
4. Zhang Y, Zou S, Cao Y, Zhang Y. Relationship between
domestic violence and postnatal depression among
pregnant Chinese women. Int J Gynecol Obstet
2012;116:26-30. Crossref
5. Song Y, Li W. The impact of social support and antepartum
emotion on postpartum depression [in Chinese]. China J
Health Psychol 2014;22:909-11.
6. Xu M, Li C, Zhang K, Sun S, Zhang H, Jin J. Comparison of
prenatal depression and social support differences between
Korean and Han pregnant women in Yanbian region [in
Chinese]. Matern Child Health Care China 2015;30:524-7.
7. Zhou X, Liu H, Li X, Zhang S, Li F, Zhao Z. Depression
and risk factors of women in their second-third trimester
of pregnancy in Shaanxi province [in Chinese]. Chin Nurs
Manage 2019;19:1005-11.
8. Liu H, Zhang C. Comparative study on service efficiency of
China’s urban and rural health systems [in Chinese]. China
Soft Sci 2011;10:102-13.
9. Leahy-Warren P, McCarthy G, Corcoran P. First-time
mothers: social support, maternal parental self-efficacy
and postnatal depression. J Clin Nurs 2012;21:388-97. Crossref
10. Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM,
Davis MM. Risk factors for depressive symptoms during
pregnancy: a systematic review. Am J Obstet Gynecol
2010;202:5-14. Crossref
11. Tang C. A review of modernisation theory and its
development on family [in Chinese]. Sociol Stud
2010;25:199-222,246.
12. Högberg U. The World Health Report 2005: “make every
mother and child count”—including Africans. Scand J
Public Health 2005;33:409-11. Crossref
13. Zhao F, Ji Y, Chen F. Conjugal or parent-child relationship?
Factors influencing the main axis of Chinese family
relations in transition period [in Chinese]. J Chin Women
Stud 2021;4:97-112.
14. Li D, Xu X, Liu J, Wu P. The relationship between life event
and pregnancy stress: the mediating effect of mental health
and the moderating effect of husband support [in Chinese].
J Psychol Sci 2013;36:876-83.
15. Dennis CL, Ross L. Women’s perceptions of partner
support and conflict in the development of postpartum
depressive symptoms. J Adv Nurs 2006;56:588-99. Crossref
16. Yang H, Lu Y, Ren L. A study on the impact of bearing
two children on urban youth’s work-family balance: the
empirical analysis based on the third survey of Chinese
women’s social status [in Chinese]. Popul Econ 2016;9:1-9.
17. Hu J, Wang Y. Study on related risk factors of patients with
pre-and postnatal depression [in Chinese]. Chin Nurs Res
2010;24:765-7.
18. Lee DT, Yip AS, Chan SS, Lee FF, Leung TY, Chung TK.
Determinants of postpartum depressive
symptomatology—a prospective multivariate study among
Hong Kong Chinese Women [in Chinese]. Chin Ment
Health J 2005;9:54-9.
19. National Bureau of Statistics of China. Income of villagers in poor rural areas in 2019 [in Chinese]. Available from:
http://www.stats.gov.cn/xxgk/sjfb/zxfb2020/202001/t20200123_1767753.html. Accessed 30 Nov 2022.
20. Sun J, Zhang J, Li C, Lu Y. Strategic judgements and
development suggestions on the development of poverty-stricken
areas in China [in Chinese]. Manage World
2019;35:150-9,185.
21. Peterman A, Schwab B, Roy S, Hidrobo M, Gilligan DO.
Measuring women’s decision making: indicator choice and
survey design experiments from cash and food transfer
evaluations in Ecuador, Uganda, and Yemen. World Dev
2021;141:105387. Crossref
22. Adouard F, Glangeaud-Freudenthal NM, Golse B.
Validation of the Edinburgh postnatal depression scale
(EPDS) in a sample of women with high-risk pregnancies
in France. Arch Womens Ment Health 2005;8:89-95. Crossref
23. Zhang H, Li L. Comparative analysis of 3 postpartum depression scales abroad [in Chinese]. Chin J Nurs
2007;2:186-8.
24. Lee DT, Yip SK, Chiu HF, et al. Detecting postnatal
depression in Chinese women. Validation of the Chinese
version of the Edinburgh Postnatal Depression Scale. Br J
Psychiatry 1998;172:433-7. Crossref
25. Liu Y, Zhang L, Guo N, Li J, Jiang H. Research progress
of Edinburgh Postnatal Depression Scale in screening
of perinatal depression [in Chinese]. Chin J Mod Nurs
2021;27:5026-31.
26. Wang Y, Guo X, Lau Y, Chan KS, Yin L, Chen J.
Psychometric evaluation of the Mainland Chinese version
of the Edinburgh Postnatal Depression Scale. Int J Nurs
Stud 2009;46:813-23. Crossref
27. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The
multidimensional scale of perceived social support. J Pers
Assess 1988;52:30-41. Crossref
28. Yan R, Liu L, Zhang L. Analysis of the relationship between social support self-efficacy and health behaviours
among college students [in Chinese]. Chin J Sch Health
2010;31:362-3.
29. Zhang X, Li X, Li Y, Quan X, Li X. Study on status and
influencing factors of antenatal depression among urban
women in western China [in Chinese]. Matern Child
Health Care China 2019;34:5275-7.
30. Dibaba Y, Fantahun M, Hindin MJ. The association of
unwanted pregnancy and social support with depressive
symptoms in pregnancy: evidence from rural southwestern
Ethiopia. BMC Pregnancy Childbirth 2013;13:135. Crossref
31. Wu H, Rao J. Research review on left-behind women [in Chinese]. J Chin Agric Univ Soc Sci 2009;26:18-23.
32. Hou F, Cerulli C, Wittink MN, Caine ED, Qiu P. Depression, social support and associated factors among women living
in rural China: a cross-sectional study. BMC Womens
Health. 2015;15:28. Crossref
33. Yue A, Gao J, Yang M, Swinnen L, Medina A, Rozelle S.
Caregiver depression and early child development: a
mixed-methods study from rural China. Front Psychol
2018;9:2500. Crossref
34. Xie RH, Yang J, Liao S, Xie H, Walker M, Wen SW. Prenatal
family support, postnatal family support and postpartum
depression. Aust N Z J Obstet Gynaecol 2010;50:340-5. Crossref
35. Wei Q, Zhang C, Hao B, Wang X. Study on parenting
concepts and behaviours of caregivers with children under
3 years old in rural areas of China [in Chinese]. Matern
Child Health Care China 2017;32:1759-61.
36. Hao J, Wang F, Huang J. Male labour migration, women
empowerment and household protein intake: evidence
from less developed rural areas in China [in Chinese].
China Rural Econ 2021;8:125-44.
37. Xiao G. A practical study of puerperal health care in a menstrual centre [in Chinese]. Chin J Mode Drug Appl
2016;10:271-2.