Hong Kong Med J 2022 Oct;28(5):410.e1–2
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Haemodynamic compensation in a patient with
bilateral vertebral artery
BD Ku, MD1; SS Yoon, MD, PhD2; SH Heo, MD, PhD2
1 Department of Neurology, International St Mary’s Hospital, Catholic
Kwandong University College of Medicine, Incheon, South Korea
2 Department of Neurology, Kyung Hee University School of Medicine, Seoul, South Korea
Corresponding author: Prof BD Ku (bondku34@cku.ac.kr)
Bilateral vertebral artery dissection (VAD) is often
related to sudden mechanical injury of the arteries
such as that following direct trauma or rotational
forces. The natural course of bilateral VAD is
variable, from recanalisation to fatal subarachnoid
haemorrhage.1 We report a patient with bilateral
VAD and favourable clinical course due to adequate
carotid haemodynamic compensation despite
progressive vertebrobasilar insufficiency.
In February 2007, a 42-year-old man
presented with acute, stabbing neck pain, radiating
to his occipital area and persisting for 5 days after
performing yoga exercises while standing on his
head. He showed no neurological deficit except for
limited neck motion due to pain. Serial magnetic
resonance angiography (MRA) 5, 12, and 19 days later
revealed progressive bilateral VAD with consequent
vertebrobasilar flow insufficiency (Fig 1). Cerebral
angiography 25 days after this dissection revealed
compensated retrograde filling of the basilar artery
(Fig 2). The MRA taken 50 days after dissection
showed much more aggravated steno-occlusive
changes in the entire vertebrobasilar circulation
(Fig 3). Unlike the progressive deterioration of
vertebrobasilar circulation, the patient’s neck pain
gradually resolved without neurological deficit.
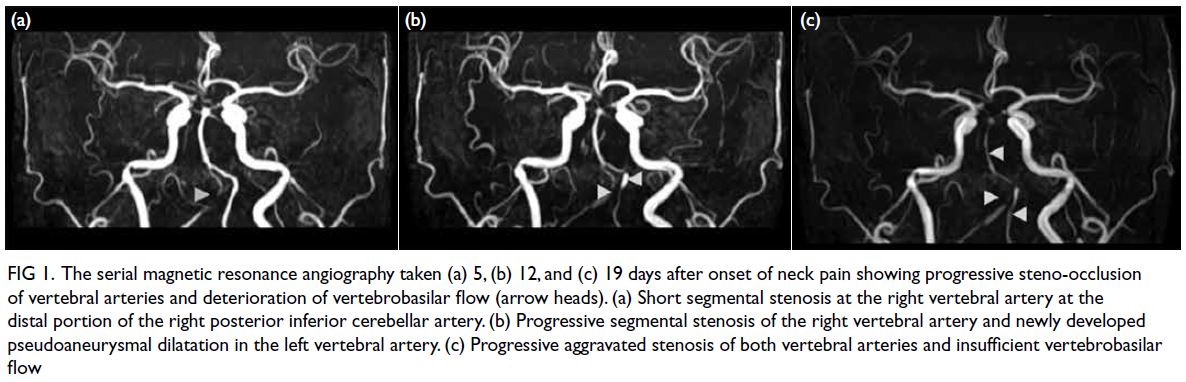
Figure 1. The serial magnetic resonance angiography taken (a) 5, (b) 12, and (c) 19 days after onset of neck pain showing progressive steno-occlusion of vertebral arteries and deterioration of vertebrobasilar flow (arrow heads). (a) Short segmental stenosis at the right vertebral artery at the distal portion of the right posterior inferior cerebellar artery. (b) Progressive segmental stenosis of the right vertebral artery and newly developed pseudoaneurysmal dilatation in the left vertebral artery. (c) Progressive aggravated stenosis of both vertebral arteries and insufficient vertebrobasilar flow
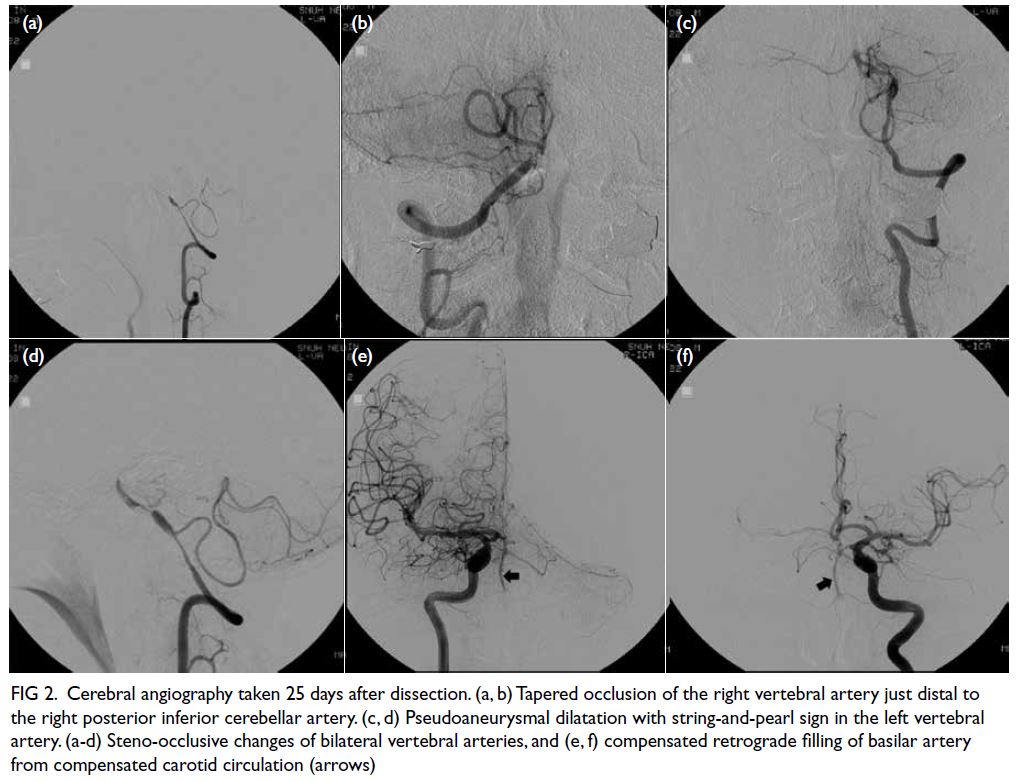
Figure 2. Cerebral angiography taken 25 days after dissection. (a, b) Tapered occlusion of the right vertebral artery just distal to the right posterior inferior cerebellar artery. (c, d) Pseudoaneurysmal dilatation with string-and-pearl sign in the left vertebral artery. (a-d) Steno-occlusive changes of bilateral vertebral arteries, and (e, f) compensated retrograde filling of basilar artery from compensated carotid circulation (arrows)
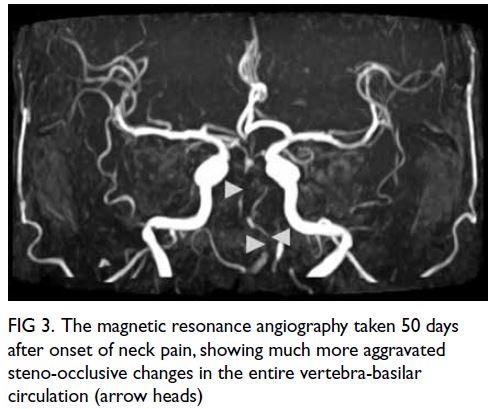
Figure 3. The magnetic resonance angiography taken 50 days after onset of neck pain, showing much more aggravated steno-occlusive changes in the entire vertebra-basilar circulation (arrow heads)
Cerebral angiography performed after the
first three MRA studies showed nearly complete
occlusion of the vertebral arteries just distal to the
bilateral posterior inferior cerebellar artery. This
protected the patient against neurological deficit. It is
unclear why the fourth MRA at 1 month later showed
further deterioration of vertebra-basilar circulation. The potential explanation for this finding may be
related to the increased compensatory carotid artery
flow through the collateral circulation. The presence
of adequate haemodynamic compensation from the
carotid artery territory constitutes an important
positive prognostic factor of the low-flow ischaemia
in a patient with bilateral VAD.1 2
Funaki et al3 reported that serial MRA could
be of great use to monitor restorative bilateral
VAD haemodynamics. In contrast, our patient
showed progressive deterioration of vertebrobasilar
circulation. This suggests that the haemodynamic
status of bilateral VAD can variably alter, so serial
MRA can help monitor the progression of dissection
in some patients.2
The present case suggests that the
haemodynamics of bilateral VAD are variable
and adequate haemodynamic compensation may
constitute a positive prognostic factor.
Author contributions
Concept or design: BD Ku.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: BD Ku.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: BD Ku.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
The authors have disclosed no conflicts of interest.
Acknowledgement
The authors would like to thank Harrisco (www.harrisco.com) for the English language review.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was conducted in accordance with the principles outlined in the Declaration of Helsinki.
References
1. de Bray JM, Penisson-Besnier I, Dubas F, Emile J.
Extracranial and intracranial vertebrobasilar dissections:
diagnosis and prognosis. J Neurol Neurosurg Psychiatry
1997;63:46-51. Crossref
2. Bacci D, Valecchi D, Sgambati E, et al. Compensatory
collateral circles in vertebral and carotid artery occlusion.
Ital J Anat Embryol 2008;113:265-71.
3. Funaki T, Oshimoto T, Wataya T, et al. Bilateral vertebral
artery dissection and its chronological changes detected
by MR angiography: a case report [in Japanese]. No To
Shinkei 2004;56:247-50.

