Hong Kong Med J 2022 Oct;28(5):376-82 | Epub 13 Sep 2022
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Vaginal delivery of second twins: factors predictive of failure and adverse perinatal outcomes
SL Mok, MB, BS, FHKAM (Obstetrics and Gynaecology); TK Lo, MB, BS, FHKAM (Obstetrics and Gynaecology)
Department Obstetrics and Gynaecology, Princess Margaret Hospital, Hong Kong
Corresponding author: Dr SL Mok (juliaslmok@yahoo.com.hk)
Abstract
Introduction: This study was performed to explore
factors associated with adverse perinatal outcomes
for second twins and to identify predictive factors
for successful vaginal delivery of the second twin
after vaginal delivery of the first twin.
Methods: This 10-year retrospective study included
231 cases of twin pregnancies in which vaginal
delivery of the second twin was attempted after
vaginal delivery of the first twin. The relationships of
obstetric characteristics with the composite adverse
perinatal outcome of the second twin were analysed.
Predictive factors for successful vaginal delivery of
the second twin were also explored.
Results: Gestational age <32 weeks was the only
independent risk factor for the composite adverse
perinatal outcome and neonatal intensive care
unit admission for the second twin. A longer inter-twin
delivery interval was associated with greater
risk of caesarean delivery of the second twin, but
it did not increase the risk of an adverse perinatal
outcome. Non-vertex presentation of the second twin at delivery was independently associated with
caesarean delivery (9.0% vs 2.0%, P=0.03). For second
twins in breech presentation, caesarean delivery was
associated with the presence of less experienced
birth attendants.
Conclusion: Among second twins born to mothers
who had attempted vaginal delivery, adverse perinatal
outcomes were mainly related to prematurity. The
presence of more experienced birth attendants
may contribute to successful vaginal delivery of the
second twin, particularly for twins in non-vertex
presentation.
New knowledge added by this study
- Among second twins born to mothers who had attempted vaginal delivery, adverse perinatal outcomes were mainly related to prematurity, rather than actual mode of delivery.
- An inter-twin delivery interval of >30 minutes alone did not increase the risk of an adverse perinatal outcome, although it increased the risk of caesarean delivery of the second twin.
- For second twins in breech presentation, caesarean delivery was independently associated with a longer intertwin delivery interval (>30 minutes) and the presence of less experienced birth attendants.
- Our findings support vaginal delivery of the second twin when the first twin is delivered in cephalic presentation.
- If monitoring of the second twin is possible and the findings are reassuring, obstetricians may consider a conservative approach, even 30 minutes after delivery of the first twin; emergency caesarean delivery should be readily available if necessary.
Introduction
Selection of the mode of delivery in a twin pregnancy
is always challenging for obstetricians, although
vaginal delivery is theoretically feasible for diamniotic
twins if the first twin is in cephalic presentation.1
In the past 15 years, two cohort studies2 3 and a
multicentre randomised trial4 concluded that when
the first twin was in cephalic presentation, planned
caesarean delivery did not significantly decrease or
increase the risk of fetal/neonatal death or serious
neonatal morbidity, compared with planned vaginal delivery. These findings suggest that vaginal delivery
of twins is a safe and reasonable mode of delivery.
However, attempts to deliver vaginally are not always
successful, and the intrapartum risks of adverse
outcomes for second twins should be carefully
considered.
In a study of factors that were predictive of
successful vaginal delivery, Easter et al5 found that
the vaginal delivery rates of second twins in non-vertex
presentation were comparable with the vaginal
delivery rates of second twins in vertex presentation. Successful vaginal delivery was associated with
higher parity. In the subgroup of second twins in non-vertex
presentation, successful vaginal delivery was
associated with the presence of more experienced
birth attendants. The rates of neonatal morbidity
and mortality were low in both groups, and they did
not differ between groups. However, that study only
included twins with gestational ages of ≥32 weeks.
In a study that examined caesarean delivery
of the second twin after successful vaginal delivery
of the first twin, Breathnach et al6 found that the
most common indication for caesarean delivery of
the second twin was malpresentation (transverse/shoulder/brow) or compound presentation. Second
twins who were delivered by emergency caesarean
section after vaginal delivery of the first twin had a
perinatal morbidity rate of 29%, but there were only
14 such twins; thus, the sample size was insufficient
for robust statistical analysis.
There is a need for additional information
concerning factors predictive of successful vaginal
delivery of the second twin, which will allow
better case selection and avoid combined vaginal-caesarean
delivery (ie, failed vaginal delivery of the
second twin). To our knowledge, there have been few
studies of these factors in Asian populations. Here,
we examined the medical records of second twins
born to mothers who had attempted vaginal delivery
of twins in Hong Kong; we sought to identify factors
that could affect the perinatal outcomes and predict
failure of vaginal delivery in a predominantly Asian
population. We also included deliveries of preterm
gestations (23-32 weeks), which were not extensively
investigated in previous studies.
Methods
This retrospective study focused on twin pregnancies
that were delivered between 1 January 2006 and 31
December 2015 in Princess Margaret Hospital, a
regional public hospital in Kowloon, Hong Kong.
Inclusion criteria were vaginal delivery of the first
twin at gestational viability or beyond. Exclusion
criteria were miscarriage (delivery before gestational
viability) or delivery of the first twin by elective
or emergency caesarean section. Under Hong
Kong law, 24 full weeks of gestation is generally
regarded as the threshold of gestational viability. In
exceptional cases, the threshold may be reduced to
23 weeks if, after full discussion with the obstetric
and neonatal care teams, the parents demonstrate
a strong preference for earlier initiation of active
neonatal management.
Eligible cases were identified from the Obstetric Clinical Information System (OBSCIS); for each case,
the mother’s demographic and clinical data were
retrieved. The OBSCIS is a territory-wide electronic
database that contains the prenatal, intrapartum, and
postpartum information of all mothers who receive
care in public hospitals in Hong Kong. Clinical
information in the system is updated in a timely
manner by each patient’s midwives and physicians
before the patient is discharged from the hospital.
Data entry integrity is continuously monitored by
a dedicated information technology team within
the Hospital Authority, and each obstetrics unit
is asked to provide missing data promptly. Each
infant’s clinical information was retrieved from the
Electronic Patient Record, a comprehensive system
that contains all health information (except obstetric
records) of patients from birth to death and is shared
by all public hospitals and out-patient clinics under
the Hong Kong Hospital Authority.
The following maternal data were retrieved:
age, parity, gestational age at delivery, chorionicity,
and mode of delivery of the second twin. The
following infant data were retrieved: birth weight,
Apgar score, cord blood pH, delivery time, inter-twin
delivery interval, presentation at delivery, and
neonatal intensive care unit (NICU) admission
status.
The primary outcome of the study was
a composite adverse perinatal outcome that
included any of the following: Apgar score <6 at
5 minutes after birth, cord blood pH <7, NICU
admission, birth trauma, and presence of neonatal
complications. For infants with a hospital stay of
>28 days, complications until hospital discharge
were included. The following complications were
considered: respiratory morbidity, intracranial
haemorrhage, hypoxic ischaemic encephalopathy,
sepsis, metabolic disturbance, birth defects, and
neonatal death. The secondary outcome was mode
of delivery. Gestational age was established by the patient’s last menstrual period and verified by
ultrasound in the first or early second trimester.
Chorionicity was established by prenatal ultrasound
and confirmed by placental histology after delivery.
The likelihood of vaginal delivery may be adversely
impacted by considerably larger second twin size,
compared with the first twin. Breathnach et al6
found that the rate of caesarean section was higher
if the first twin had ≥20% lower weight than the
second twin. Therefore, clinically significant weight
discordance was regarded as ≥20% in the present
study, where weight discordance was defined as the
weight difference between the second and first twin
divided by the weight of first twin.
Vaginal deliveries of twins were managed in
accordance with our labour ward protocol, which
does not regard estimated fetal weight discordance as
a contra-indication to vaginal delivery. All deliveries
were attended by two physicians (as described
below) and assisted by ≥2 midwives. Specialist
supervision was recommended. In this context,
a specialist is an obstetrician who has completed
≥6 years of postgraduate residency training and
received accreditation as a Fellow of the Hong
Kong College of Obstetricians and Gynaecologists
(FHKCOG). Membership in the Royal College of
Obstetricians and Gynaecologists (MRCOG) is a
prerequisite for FHKCOG accreditation. When a
specialist was unavailable (particularly at night),
deliveries were conducted or supervised by an
MRCOG-qualified physician. Paediatricians were
present for all deliveries of second twins. Prenatal
steroids (either betamethasone or dexamethasone
depending on pharmacy availability and initial
treatment at the referral unit) were administered
in cases of delivery before 34 weeks of gestation.
If necessary, oral nifedipine was used as a first-line
tocolytic. Intravenous salbutamol was used as a
second-line tocolytic until 2012; since 2013, atosiban
has been used as a second-line tocolytic.
Statistical analysis was carried out using
SPSS software (Windows version 17.0; SPSS Inc.,
Chicago [IL], United States). Categorical data were
analysed by the Chi squared test or Fisher’s exact
test, as appropriate. Among the factors that showed
statistical significance in univariate analysis, binary
logistic regression was used to identify factors that
were independently predictive of vaginal delivery
and adverse perinatal outcomes. P values <0.05 were
considered statistically significant.
Results
During the 10-year study period, 47 595 deliveries
were performed in Princess Margaret Hospital;
718 twin pairs were delivered. Among these twin
pairs, 182 and 305 were delivered by elective and
emergency caesarean section, respectively; they were excluded from the study. In the remaining
231 cases, the mothers delivered the first twin
vaginally and intended to deliver the second twin
vaginally. The second twins in this group of patients
were included for analysis.
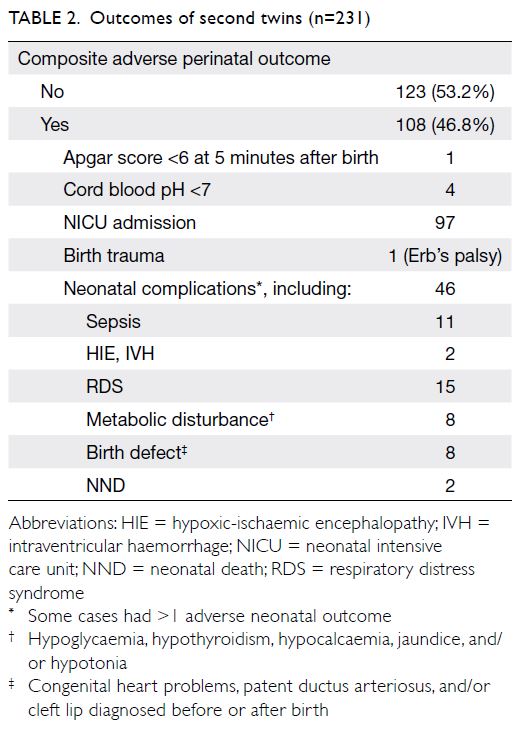
Table 1 shows the demographic and obstetric
characteristics of the 231 cases, stratified according
to the mode of delivery of the second twin.
Emergency caesarean delivery was required in
10 cases (4.3%). Among the three second twins in
vertex presentation, two were delivered by caesarean
section because of second twin retention; the
remaining twin was delivered by caesarean section
because of fetal distress. Among the seven second
twins in non-vertex presentation, the indications for
caesarean delivery were second twin retention (two
cases), fetal distress (four cases), and transverse lie
(one case). Of the factors shown in Table 1, only an
inter-twin delivery interval of >30 minutes and non-vertex
presentation of the second twin at delivery
were associated with the mode of delivery of the
second twin. Logistic regression analysis showed
that an inter-twin delivery interval of >30 minutes
(odds ratio [OR]=26.952, 95% confidence interval
[CI]=5.924-122.619) and non-vertex presentation
of the second twin at delivery (OR=5.003,
95% CI=1.101-22.743) were independently
associated with caesarean delivery of the second
twin.
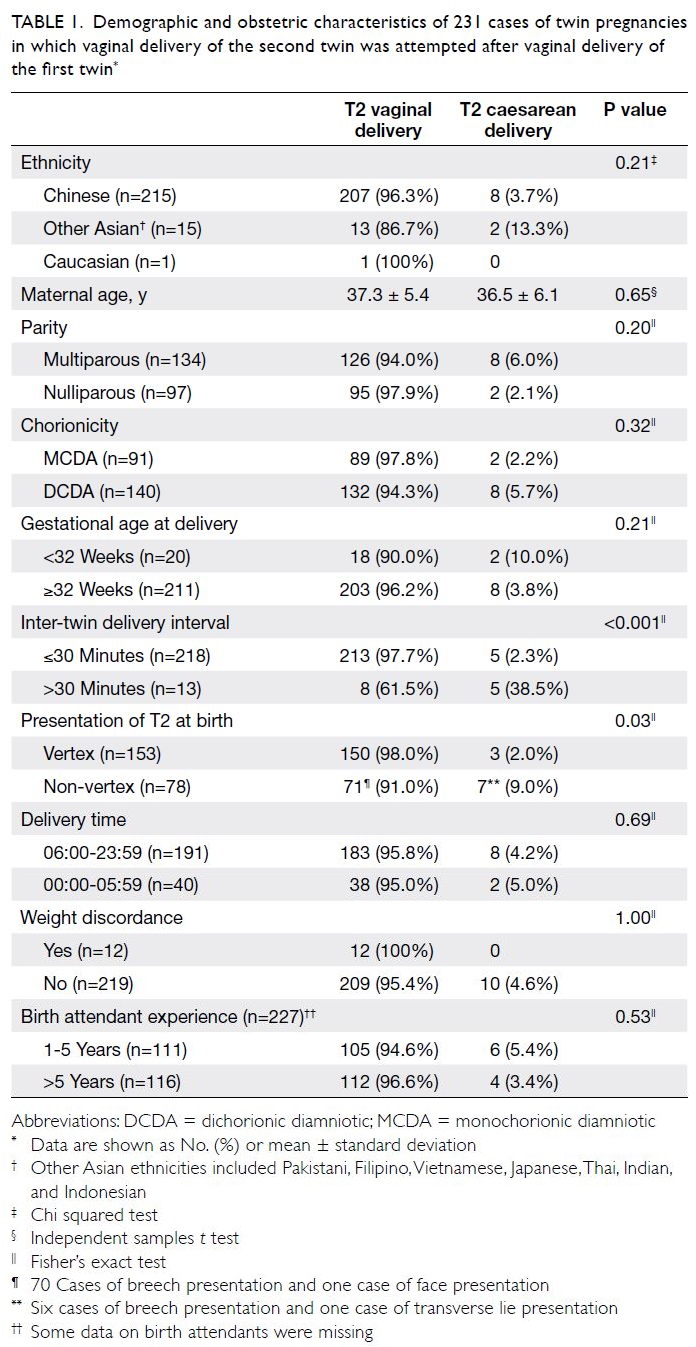
Table 1. Demographic and obstetric characteristics of 231 cases of twin pregnancies in which vaginal delivery of the second twin was attempted after vaginal delivery of the first twin
In subgroup analyses, we examined the
relationships of the demographic and obstetric
factors in Table 1 to determine their relationships
with the mode of delivery for second twins in breech
presentation. Univariate analysis revealed that only
an inter-twin delivery interval >30 minutes and
the presence of less experienced birth attendants
were significantly associated with the mode of
delivery. Logistic regression showed that an inter-twin
delivery interval >30 minutes (OR=36.492,
95% CI=3.035-438.712) and the presence of
less experienced birth attendants (OR=10.252,
95% CI=1.001-104.956) were independently
associated with caesarean delivery of second twins
in breech presentation.
Perinatal outcomes of second twins are
shown in Table 2. Univariate analysis revealed
that the composite adverse perinatal outcome was
only associated with gestational age <32 weeks
(P<0.001; OR=12.1, 95% CI=2.738-53.481) [Table 3].
Similarly, gestational age <32 weeks was the only
factor significantly associated with NICU admission
(P<0.001; OR=6.420, 95% CI=2.073-19.878) [Table 4].
Among the 47 cases with delivery before 34
weeks of gestation, 27 completed steroid treatment
before delivery. In 17 cases, delivery occurred before
the completion of steroid treatment because of rapid
labour that did not respond to tocolytics. Steroid
treatment was not administered in three cases; two of these cases involved delivery before 24 weeks
of gestation, which is the threshold for beginning
steroid treatment in our hospital. In the third
case, the mother was admitted in advanced labour.
Completion or non-completion of steroid treatment
was not associated with the composite adverse
perinatal outcome (25/27 vs 18/20, P=0.753).
Discussion
To our knowledge, this is the first study in Hong Kong concerning the short-term composite adverse
perinatal outcomes of second twins in cases where
vaginal delivery was attempted. Our approach
enabled simultaneous consideration of multiple
outcome parameters. The inclusion of additional
clinical information until hospital discharge for
infants with prolonged hospital stay (>28 days)
allowed a more comprehensive assessment of
outcomes. Notably, cases of gestation <32 weeks
were included; there are minimal published data
for this group of infants because they have been
excluded from many large trials. Additionally, we
examined the effects of birth attendant experience
and birth timing.
Perinatal outcomes
Prior to this study, there were two analyses of twin deliveries in a predominantly Asia population,
both from Hong Kong. The first analysis mainly
focused on patient preference regarding the mode
of delivery; it also included few vaginal deliveries
(35 cases).7 The second analysis, reported by Tang
et al,8 was performed in the same obstetric unit
as the first analysis; it reviewed neonatal and
maternal outcomes after an increase in the rate of
vaginal delivery of twins. The authors did not find any significant differences in neonatal morbidities
between the vaginal delivery group and the elective
caesarean delivery group. However, there were fewer
successful vaginal deliveries of ≥1 twin (72 cases)
and the effect of inter-twin delivery interval was not
evaluated.
In this study, the main factor that affected
the composite adverse perinatal outcome was
gestational age; complications were mainly related
to prematurity. Similarly, NICU admission was
mainly related to complications of prematurity,
rather than complications of vaginal delivery. There
were no statistically significant differences in adverse
perinatal outcomes, even for twins who were not
delivered in cephalic presentation. Thus, non-cephalic
presentation alone should not be considered
sufficient to recommend caesarean delivery for twin
pregnancies.
A study in Hong Kong by Leung et al,9 published
in 2002, showed that all umbilical cord blood gas
parameters in the second twin were significantly
associated with the inter-twin delivery interval. The
risk of severe fetal acidosis was 27% if the second twin
was not delivered ≤30 minutes after delivery of the
first twin, but the outcomes of second twins were not
analysed. In our study, an inter-twin delivery interval
of >30 minutes alone did not increase the risk of
short-term adverse perinatal outcomes, although it
increased the risk of caesarean delivery of the second
twin. Schneuber et al10 also reported similar findings
in their series, which suggested that an increased
inter-twin delivery interval was not associated with
adverse fetal outcomes. If monitoring of the second
twin is possible and the findings are reassuring,
obstetricians may thus consider a conservative
approach, even 30 minutes after delivery of the first
twin; however, emergency caesarean delivery should
be readily available if necessary.
Our study also showed no increase in adverse
perinatal outcomes for infants who were delivered
after midnight. In general, delivery of twins in
daytime or early evening is preferable because
additional staff are present, and those staff are often
more experienced. Therefore, when there are no
indications for urgent delivery, the usual practice
in our unit is to begin labour induction for twin
pregnancies in the early morning. Deliveries after
midnight usually follow spontaneous labour and
are thus unplanned. However, such deliveries are
supervised by the most senior on-call obstetrician
(MRCOG-qualified or FHKCOG-accredited) during
the intrapartum period.
Delivery of non-cephalic second twin
The vaginal delivery of second twins in non-cephalic presentation is challenging. Our findings showed
a higher rate of caesarean delivery for second
twins in non-cephalic presentation (9.0% vs 2.0%, P=0.03). In a large cohort study using the World
Health Organization Global Survey dataset, Vogel
et al11 showed that caesarean rates were 6.2% and
0.9% for second twins in non-cephalic and cephalic
presentation, respectively. Another study by Kong
et al12 revealed the caesarean delivery rates of
second twins were 4.7% in cephalic presentation,
11.1% in breech presentation, and up to 90% in
transverse lie. In both of these studies, analyses were
conducted based on the presentation of the second
twin at the onset of labour; their findings were
consistent with our results. The presence of more
experienced obstetricians who are able to perform
artful manoeuvres (ie, internal podalic version and
external cephalic version) can increase the likelihood of successful vaginal delivery of the second twin.
Regular training and rehearsal of the vaginal delivery
of twins is important for obstetricians to maintain
their skills.
Caesarean section of second twin
In our study, caesarean delivery of the second twin
was necessary in 4.3% of cases, which is similar to
or lower than the proportions in other series.6 8 13 14
Regardless of whether the second twin was delivered
by caesarean section, there were no significant
increases in short-term adverse perinatal outcomes;
however, this mode of delivery is less favourable for
mothers. These results are contrary to the findings by
Breathnach et al,6 in which the perinatal morbidity
rate was 29% among second twins delivered by
emergency caesarean section after vaginal delivery
of the first twin. A systematic review by Rossi et al15
also showed a higher rate of morbidity in second
twins after caesarean delivery (19.8% vs 9.5% after
vaginal delivery). Thus, combined vaginal-caesarean delivery of twins should be avoided whenever possible.
In the present study, the presence of a larger
second twin (≥20% weight discordance) did not
significantly increase the risk of caesarean delivery.
The second twin was larger in only 12 cases (5.2%).
We suspect that many other cases with a larger second
twin were scheduled for caesarean delivery without
a trial of vaginal delivery. Decisions concerning the
mode of delivery are affected by the estimated fetal
weight, fetal presentation, and whether the mother
has a history of successful vaginal delivery. Various
factors must be carefully considered in each case.
Limitations
There were some limitations in this study. First, the retrospective design may have resulted in missing
data or incomplete data collection. This is not a large
problem because clinical information in the OBSCIS
and the Electronic Patient Record is required to be
updated when each patient is discharged from the
hospital; therefore, these systems are reliable sources
of patient data. Nevertheless, some information
was not retrievable, such as the presentation of
the second twin at the time of first twin delivery
and whether birth attendant manoeuvres were
necessary to deliver the second twin. Second, the
non-randomised analysis might have led to selection
bias concerning the mode of delivery, such that
low-risk cases were over-represented in the study.
The number of second twins delivered by caesarean
section was small; a larger trial is needed to more
comprehensively evaluate such cases.
Conclusion
Among second twins born to mothers who
had attempted vaginal delivery, we found that
adverse perinatal outcomes were mainly related to
prematurity, rather than actual mode of delivery. For
all second twins, an inter-twin delivery interval <30
minutes was associated with a higher rate of vaginal
delivery; for second twins in breech presentation, the
presence of more experienced birth attendants was
also associated with a higher rate of vaginal delivery.
Overall, the risk of caesarean delivery of the second
twin was low. Our findings in a predominantly Asian
population in Hong Kong support vaginal delivery
of the second twin when the first twin is delivered in
cephalic presentation.
Author contributions
This study was planned and designed by both authors. Both authors also jointly performed the data analysis. TK Lo
provided leadership and supervision, while SL Mok wrote
and managed the manuscript. Both authors had full access to
the data, contributed to the study, approved the final version
for publication, and take responsibility for its accuracy and
integrity.
Conflicts of interest
Both authors have disclosed no conflicts of interest.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was approved by the Kowloon West Cluster Research Ethics Committee (Ref KW/EX-17-154 (118-02)).
The requirement for patient informed consent was waived
because this was a retrospective review of medical records
that did not involve patient participation.
References
1. Monson M, Silver RM. Multifetal gestation: mode of delivery. Clin Obstet Gynecol 2015;58:690-702. Crossref
2. Peaceman AM, Kuo L, Feinglass J. Infant morbidity and mortality associated with vaginal delivery in twin
gestations. Am J Obstet Gynecol 2009;200:462.e1-6. Crossref
3. Fox NS, Silverstein M, Bender S, Klauser CK, Saltzman DH,
Rebarber A. Active second-stage management in twin
pregnancies undergoing planned vaginal delivery in a U.S.
population. Obstet Gynecol 2010;115:229-33. Crossref
4. Barrett JF, Hannah ME, Hutton EK, et al. A randomized
trial of planned cesarean or vaginal delivery for twin
pregnancy. N Engl J Med 2013;369:1295-305.Crossref
5. Easter SR, Lieberman E, Carusi D. Fetal presentation and successful twin vaginal delivery. Am J Obstet Gynecol 2016;214:116.e1-10.Crossref
6. Breathnach FM, McAuliffe FM, Geary M, et al. Prediction
of safe and successful vaginal twin birth. Am J Obsetet
Gynecol 2011;205:237.e1-7. Crossref
7. Liu AL, Yung WK, Yeung HN, et al. Factors influencing
the mode of delivery and associated pregnancy outcomes
for twins: a retrospective cohort study in a public hospital.
Hong Kong Med J 2012:18:99-107.
8. Tang HT, Liu AL, Chan SY, et al. Twin pregnancy
outcomes after increasing the rate of vagina twin
delivery: retrospective cohort study in a Hong Kong
regional obstetrics unit. J Maternal Fetal Neonatal Med
2016;29:1094-100. Crossref
9. Leung TY, Tam WH, Leung TN, Lok IH, Lau TK. Effect of
twin-to-twin delivery interval on umbilical cord blood gas
in the second twins. BJOG 2002;109:63-7. Crossref
10. Schneuber S, Magnet E, Haas J, et al. Twin-to-twin delivery
time: neonatal outcome of second twin. Twin Res Hum
Genet 2011;14:573-9. Crossref
11. Vogel JP, Holloway E, Cuesta C, Carroli G, Souza JP,
Barrett J. Outcomes of non-vertex second twins, following
vertex vaginal delivery of first twin: a secondary analysis of
the WHO Global Survey on maternal and perinatal health.
BMC Pregnancy Childbirth 2014;14:55. Crossref
12. Kong CW, To WW. The predicting factors and outcomes
of caesarean section of the second twin. J Obstet Gynaecol
2017;37:709-13. Crossref
13. Yang Q, Wen SW, Chen Y, Krewski D, Fung KF, Walker M.
Neonatal death and morbidity in vertex-nonvertex second
twins according to mode of deliverya and birth weight. Am
J Obstet Gynecol 2005;192:840-7. Crossref
14. Persad VL, Baskett TF, O’Connell CM, Scott HM.
Combined vaginal-cesarean delivery of twin pregnancies.
Obstet Gynecol 2001;98:1032-7. Crossref
15. Rossi AC, Mullin PM, Chmait RH. Neonatal outcomes
of twins according to birth order, presentation and mode
of delivery: a systematic review and meta-analysis. BJOG
2011;118:523-32. Crossref