Hong Kong Med J 2022 Oct;28(5):367-75 | Epub 1 Aug 2022
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Behavioural adaptations and responses to
obstetric care among pregnant women during an early stage of the COVID-19 pandemic in Hong Kong: a cross-sectional survey
PW Hui, MD, FRCOG; Mimi TY Seto, MB, BS, MRCOG; KW Cheung, MB, BS, MRCOG
Department of Obstetrics and Gynaecology, Queen Mary Hospital, Hong Kong
Corresponding author: Dr PW Hui (apwhui@hku.hk)
Abstract
Introduction: This study evaluated behavioural
adaptations and responses to obstetric care among
pregnant women during an early stage of the
coronavirus disease 2019 (COVID-19) pandemic.
Methods: This cross-sectional survey included
pregnant women who received obstetric care from
27 May 2020 to 16 June 2020 in a university-affiliated
hospital in Hong Kong. Responses were collected
with respect to obstetric appointment scheduling,
workplace changes, mask-wearing practices, travel
and quarantine experiences, obstetric service
adjustments, and visiting arrangements. Regression
analysis was used to compare the effects of patient
characteristics on their responses.
Results: In total, 1000 surveys were distributed;
733 pregnant women provided complete survey
responses. Among obstetric-related appointments in
public hospitals, 16% were postponed or cancelled by
pregnant women; such changes were most frequent
among women beyond 24 weeks of gestation,
women who had previous deliveries, and women
who had a history of mental illness. The practice of
working from home imposed psychological stress
and negatively impacted the pregnancy experience in 4.5% of women. Childbirth companionship was
regarded as an important service by 88.1% of women;
only 4.2% agreed with its suspension. Obstetric
service adjustments had the greatest impact on
Chinese women and nulliparous women.
Conclusions: The findings provide an overview
of how pregnant women adapted during an early
stage of the COVID-19 pandemic. Women adjusted
obstetric service attendance, began working from
home, and wore masks. Women’s expectations did
not match changes in childbirth companionship and
peripartum services. Hospital administrators should
consider psychological impacts on pregnant women
when implementing service adjustments.
New knowledge added by this study
- Pregnant women, especially women who had previous deliveries and a history of mental illness, were more likely to postpone or cancel obstetric appointments during an early stage of the coronavirus disease 2019 (COVID-19) pandemic.
- While working from home improved the overall pregnancy experience for most women, it caused psychological stress and had a negative influence in 4.5% of respondents.
- Childbirth companionship was considered important by 88.1% of the respondents; only 4.2% of respondents fully accepted its suspension.
- Obstetricians and policy makers should be aware of mismatches in the expectations of pregnant women concerning childbirth companionship and peripartum services; infection control should be balanced with peripartum needs.
- Obstetric service adjustments had the greatest impact on Chinese women and nulliparous women.
Introduction
Coronavirus disease 2019 (COVID-19) has had
substantial psychosocial impacts worldwide
and caused major behavioural changes. In 2020,
increased stress and anxiety levels were reported in
countries with major disease spread.1 2 3 4 5 6 Pregnancy is considered a risk factor for COVID-19 because
of relative maternal immunosuppression; there is
also a risk of vertical transmission.7 8 9 10 11 Importantly, behavioural changes have been recognised among
pregnant women.4 The pandemic situation could potentially disrupt obstetric care for pregnant women.8 Thus, it is important to study how the pandemic has affected obstetric care and pregnancy experiences.
Considering the severe adult respiratory
syndrome (SARS) outbreaks in 2002 to 2003 in
Hong Kong, a serious alert level was announced
on 4 January 2020 in response to the emergence of
novel coronavirus pneumonia in Wuhan, China.12 13
This was escalated to an emergency alert level on
25 January 2020. Corresponding policies were
imposed in public hospitals with each alert
announcement. In obstetric units, husbands and
partners were no longer allowed to accompany
pregnant women for labour and delivery. No visiting
was allowed for mothers or babies staying with their
mothers in postnatal wards. All antenatal exercise
classes, antenatal seminars, hospital tours, and
postnatal classes were suspended. Many workplaces
for women and their partners shifted to working from
home. These changes were coupled with suspensions
of schools and non-urgent community services.
The infection continued to spread worldwide;
the COVID-19 pandemic was recognised by the
World Health Organization on 11 March 2020.
On 20 March 2020, the first case of COVID-19 in
a pregnant woman was confirmed in Hong Kong.
The local government subsequently restricted travel
with additional quarantine measures and mandated
social distancing in late March 2020.12 This study
was conducted in the middle of 2020 to examine how
pregnant women responded to changes in obstetric
care and alterations in the workplace during an early
stage of the COVID-19 pandemic; it also investigated their adaptations to the practices of mask wearing
and social distancing.
Methods
This prospective questionnaire survey was conducted in the obstetric unit of a university-affiliated tertiary
public hospital in Hong Kong from 27 May 2020
to 16 June 2020 in English (online supplementary Table 1) and Traditional Chinese (online supplementary Table 2). Pregnant women were
invited to participate in an online questionnaire
upon admission to obstetric wards or attendance
to obstetric clinics; each invitation was provided
by a midwife (in an obstetric ward) or a designated
research assistant (in an obstetric clinic). Clinic
sessions included an antenatal check-up, ultrasound
scan, and screenings for gestational diabetes and
Group B streptococcus. The survey was administered
to all women who could read either Chinese or
English. Each woman received an information
leaflet containing an introduction of the project, a
description of key events related to COVID-19 from
January 2020 to March 2020, and a QR code linked
to an online survey. The participants could begin
the survey by scanning the QR code, selecting the
language, and providing their consent.
The survey was developed by the authors and
tailored to address issues related to the impacts
of COVID-19 on obstetric services. Prior to this
study, the survey content was validated by local
consultant obstetricians and midwives; it consisted
of demographic data collection and questions that
involved five domains. These domains were related
to obstetric appointment scheduling, workplace
changes, mask-wearing practices, travel and
quarantine experiences, and adjustments to birth
companionship and visiting hours since the first
novel coronavirus alerts were announced in January
2020. Concerning obstetric appointment scheduling,
participants were asked whether their appointments
had been postponed or rescheduled from a public
hospital to a private hospital. Concerning workplace
changes, participants were asked whether they
and/or their partners had begun to work from home;
they were then asked to describe the impact of the
change on their pregnancy experience. Concerning
mask-wearing practices, participants were asked
about their pattern and type of mask use. With
respect to travel and quarantine, participants
were asked whether they had travelled because of
COVID-19 risk; they were also asked about their
experiences with COVID-19 testing and quarantine.
Regarding the importance of birth companionship
and visiting hours, as well as the acceptance of service
adjustments and relief measures, participants were
asked to rate their opinions of these factors using a
visual analogue scale of 0 to 100, with 100 as very
important or strongly accepted.
Women with gestational age ≤24 weeks
were regarded as the early gestational group,
while women with gestational age >24 weeks and
women in the postnatal period were regarded as
the late gestational group. The COVID-19 alert
was announced by the Hong Kong government on
4 January 2020, slightly more than 20 weeks prior
to the commencement of this study. Women in the
early gestational group conceived after the date of
COVID-19 alert announcement, while women in
the late gestational group were already pregnant
on the announcement date. Statistical analysis was
performed using SPSS software (Windows version
26.0; IBM Corp, Armonk [NY], United States).
The distributions of continuous variables were
checked for normality. Analysis of variance and t
test assessments were used for normally distributed
variables, while the Mann-Whitney U test was used
for non-normally distributed variables. Categorical
variables were evaluated by the Chi squared test
or Fisher’s exact test. Regression analysis was
performed to examine the effects of marital status,
ethnic background, parity, and mental illness on the
behaviours of pregnant women regarding antenatal
appointment rescheduling and their opinions of
obstetric service adjustments. A value of P<0.05 was
considered significant.
Results
In total, 1000 information leaflets were distributed to 200 women in obstetric wards and 800 women
in out-patient clinics. In all, 890 responses were
registered online, including 878 women who
consented to participate and 12 women who did not
consent. Among women who agreed to participate,
145 did not finish the survey; thus, 733 completed
responses were available for analysis.
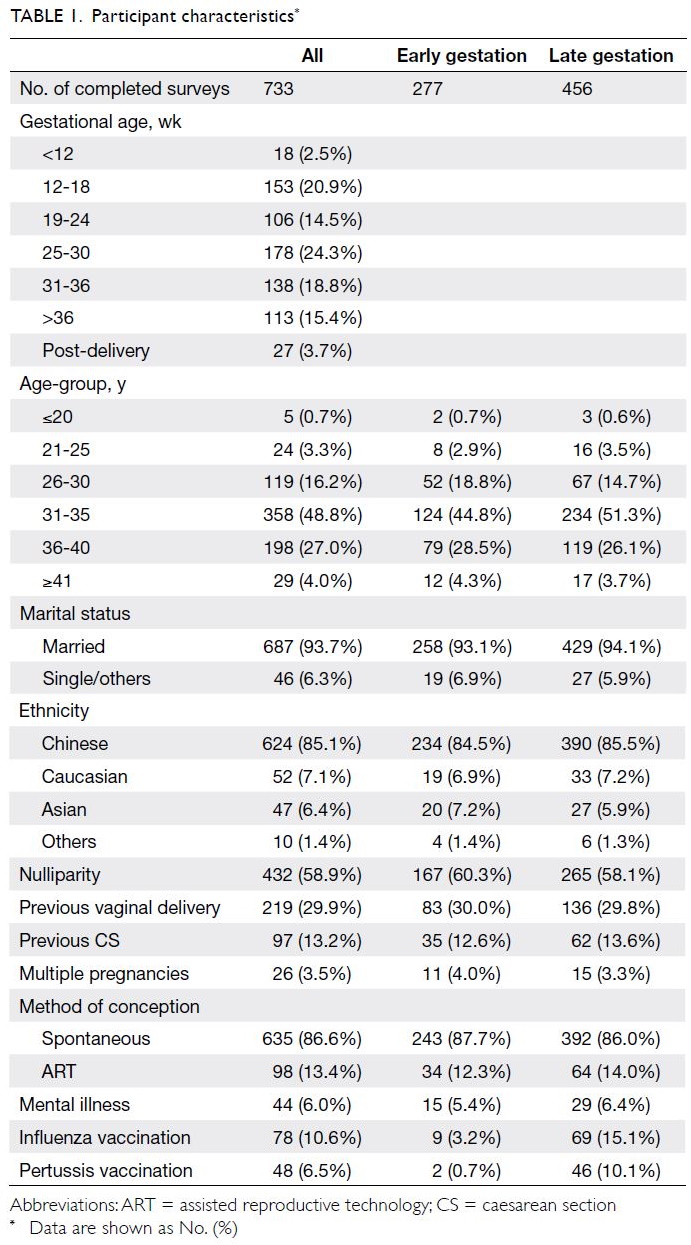
Table 1 shows the basic demographic
characteristics of the participants. Women aged
31 to 35 years constituted nearly half (48.8%) of
the respondents. The largest gestational age-group
was 25 to 30 weeks (24.3%). With the exception
of influenza and pertussis vaccination histories,
other background characteristics were comparable
between early and late gestational groups.
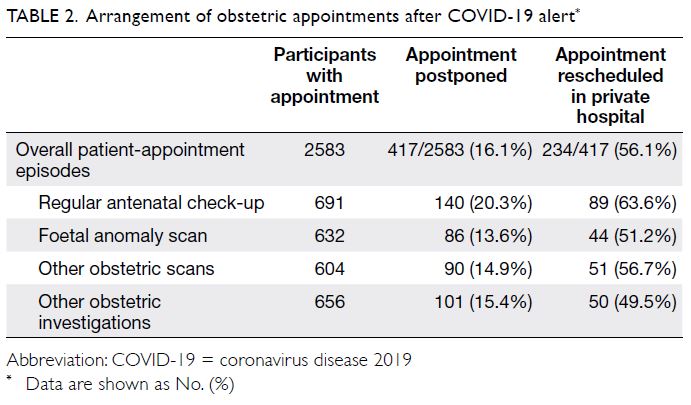
Obstetric appointment scheduling
Among 2583 patient appointments, 417 (16.1%)
were postponed or cancelled by pregnant women.
Over half (56.1%) of these were rescheduled to
a private hospital. The rate of postponement or
cancellation was higher for regular antenatal
visits (20.3%) and lower for foetal anomaly scans
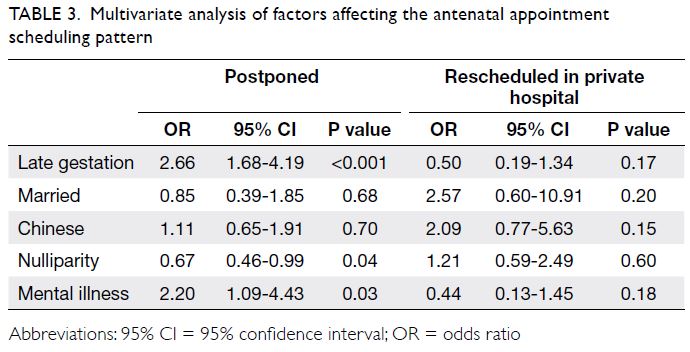
(13.6%) [Table 2]. Multivariate analysis showed that
women in the late gestational group (odds ratio
[OR]=2.66; 95% confidence interval [CI]=1.68-4.19;
P<0.001) and women with mental illness (OR=2.20; 95% CI=1.09-4.43; P=0.03) were more likely to
postpone or cancel regular antenatal appointments,
while nulliparous women (OR=0.67; 95% CI=0.46-0.99; P=0.04) were less likely to make such changes
(Table 3). No significant associations of demographic
characteristics with ultrasound and investigation
appointments (blood test, screening of Down’s
syndrome, or Group B streptococcus colonisation)
were identified.
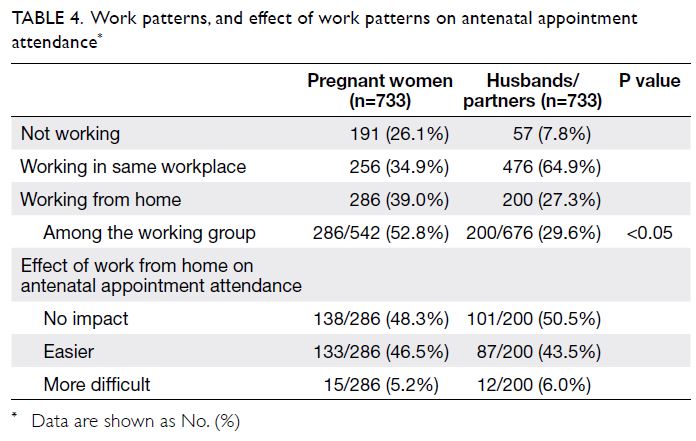
Working from home
As shown in Table 4, there were 542 (73.9%) working
women in this study; more than half of them began
working from home after the COVID-19 alert
announcement. Compared with their husbands/partners, significantly more women were working
from home (29.6% vs 52.8%; P<0.05). Among
women working from home, this work pattern facilitated obstetric appointment attendance for
46.5% (133/286) of the women and 43.5% (87/200)
of their husbands/partners. There was a tendency
for decreased omission of antenatal appointments
among women working at home, compared with
women working in usual workplaces, although the
differences were not statistically significant for any
type of appointment (antenatal check-up 6.6% vs
6.7%, P=0.10; anomaly scan 3.7% vs 8.0%, P=0.09;
obstetric scan 3.5% vs 6.6%, P=0.22; obstetric
investigations 5.1% vs 8.3%, P=0.30).
Overall pregnancy experience
Among the 131 women who reported that both they
and their husbands/partners worked from home,
107 (81.7%) reported a better overall pregnancy
experience. Among the 224 women who reported
that they or their husbands/partners worked from
home, 139 (62.1%) felt this work arrangement had
made their overall pregnancy experience better while
13 (5.8%) felt this had made their experience worse.
A significantly greater proportion of respondents
reported a much better overall pregnancy experience
when both they and their husbands/partners were
working from home than when either they or their
husbands/partners were working from home (50.4%
vs 31.7%; P=0.001). In contrast, suspension of school
and community services had more negative impacts
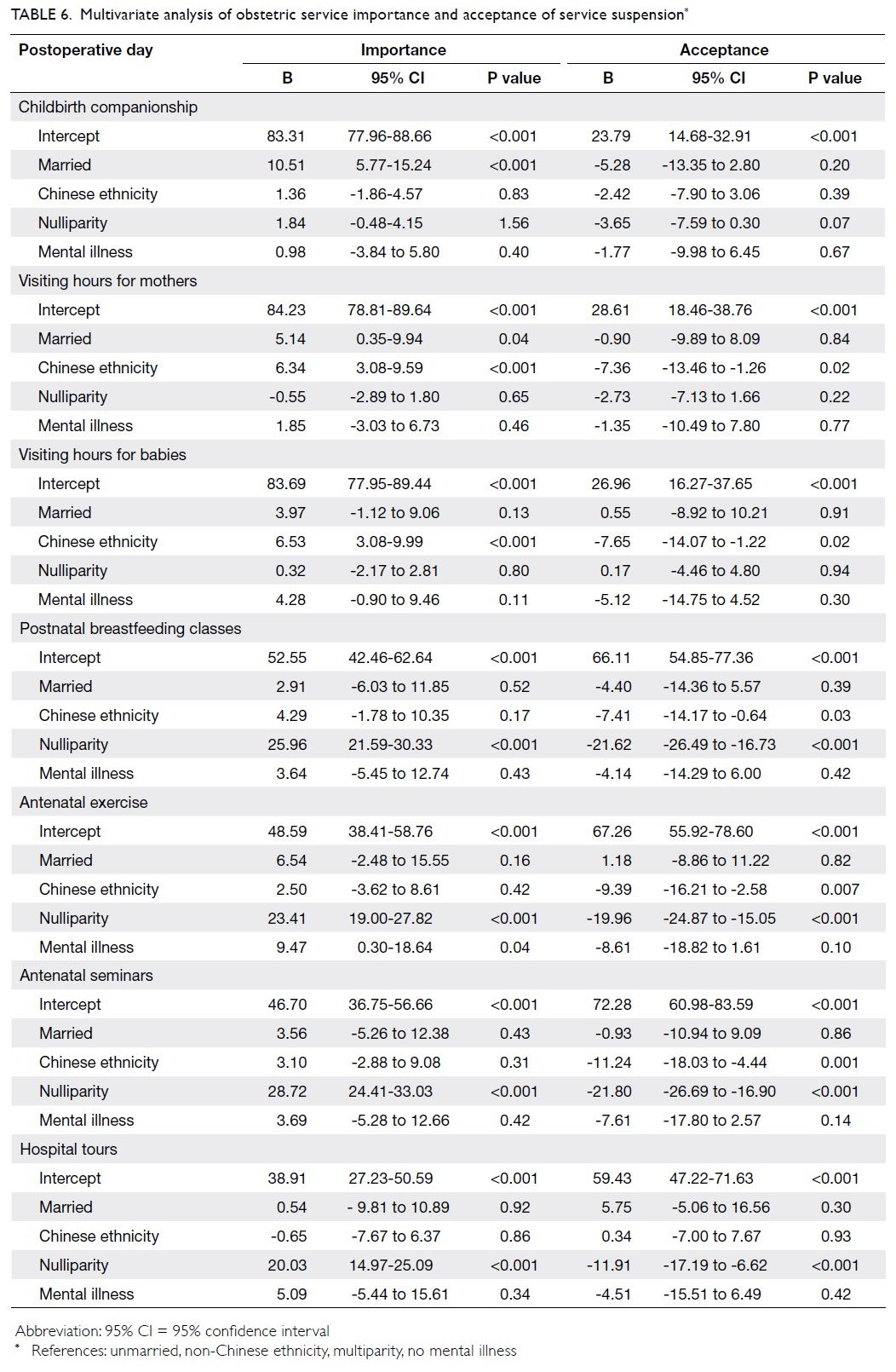
on pregnancy experience (Table 5).
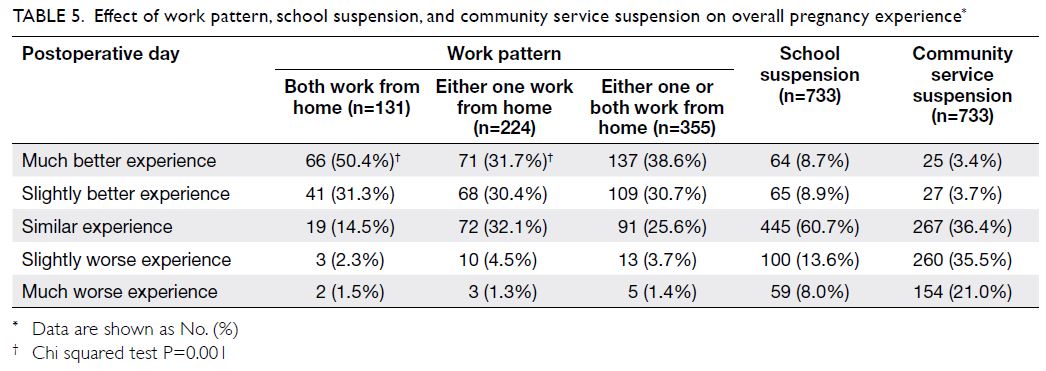
Table 5. Effect of work pattern, school suspension, and community service suspension on overall pregnancy experience
More time to spend at home was selected by
80.1% (197/246) of the respondents as a beneficial
effect of working from home on their pregnancy
experience (online supplementary Table 3). Among
18 women who had a worse pregnancy experience
because of working from home, more psychological
stress was chosen by 13 (72.2%) women as one of the
underlying reasons. Five (27.8%) women reported
greater conflict with their husbands/partners because
of working from home (online supplementary Table 4).
Mask-wearing practices
The mean proportion of mask-wearing time was
significantly greater in clinical areas (97.2% for
hospitals and 97.0% for clinics) than in outdoor
areas (89.3%) and at home (4.1%, P<0.05). Over
90% of respondents always wore masks in clinical
areas; 63.8% always wore masks outdoors, and 0.8%
always wore masks at home. Among all women in
the study, surgical masks were most commonly
used; N95 masks were used by 55 (7.5%) women
in hospitals and 32 (4.4%) women in clinics (online supplementary Table 5).
Travel and quarantine experiences
Since the announcement of the COVID-19 alert,
6.8% (50/733) of respondents had travelled abroad because of COVID-19 risk in Hong Kong; 13.4%
(98/733) of respondents had returned to Hong Kong
because of COVID-19 risk abroad. Additionally, 31
(4.2%) women had been quarantined and 26 (3.5%)
women had lived with household members during
home quarantine. Coronavirus disease 2019 testing
had been performed in 3.7% of all respondents.
Moderate to marked emotional disturbance related
to personal quarantine experience was reported by
64.5% (20/31) of the women (online supplementary Table 6).
Adjustments of birth companionship and
visiting hours
Husband/partner companionship during childbirth
was regarded as the most important obstetric service,
followed by visiting hours for pregnant women and
neonates. Childbirth companionship was considered
important by 88.1% of the respondents; only 4.2%
of the respondents fully accepted its suspension.
In contrast, suspension of hospital tours was fully
accepted by 27.0% of the respondents (online supplementary Fig). Univariate analysis showed
that marital status, ethnicity, parity, and history of
mental illness were factors that influenced opinions
of obstetric service importance and acceptance of
service suspension. Regression analysis showed that
being married was strongly associated with greater
perceived importance of childbirth companionship
(B=10.51; 95% CI=5.77-15.24) and visiting hours
for mothers (B=5.14; 95% CI=0.35-9.94). Chinese
women had the greatest perceived importance of
visiting arrangements for both mothers and babies;
they had the least acceptance of suspension of those
services. Nulliparity was only factor significantly
associated with the perceived importance of
antenatal exercise (B=23.41; 95% CI=19.00-27.82),
antenatal seminars (B=28.72; 95% CI=24.41-33.03),
hospital tours (B=20.03; 95% CI=14.97-25.09),
and postnatal breastfeeding classes (B=25.96;
95% CI=21.59-30.33) [Table 6].
Discussion
Summary
To our knowledge, this is the first study of the behavioural adaptations and responses to obstetric
care among pregnant women during an early stage
of the COVID-19 pandemic in Hong Kong, a city
which previously experienced SARS outbreaks in
2002-2003. Approximately 16% of obstetric-related
appointments in public hospitals were postponed or
cancelled by pregnant women because of COVID-19,
but only 56% of these appointments were
rescheduled in private hospitals. Women who had
previous deliveries and a history of mental illness
were more likely adjust their appointments. Working
from home during the COVID-19 pandemic
improved the overall pregnancy experience in most
respondents. However, approximately 5% of women
reported negative impacts on their pregnancy
experiences, primarily because of psychological
stress. Concerning obstetric services, nearly 90% of
the women considered childbirth companionship
to be important; <5% of the women fully accepted
its suspension. More than 80% of the respondents
regarded visiting for mothers and newborns as
very important aspect of the overall pregnancy
experience. Obstetric service adjustments had the
greatest impact on Chinese women and nulliparous
women.
Antenatal care
Delays in seeking medical attention for acute medical
conditions such as cardiac and cerebrovascular
events were reported in 2020.14 15 16 Importantly,
failure to attend scheduled antenatal care can lead to
adverse outcomes.17 18 Women in the late gestational
group were already pregnant on the date of the
COVID-19 alert announcement; they might
have reported more adjustments to obstetric
appointments. Additionally, their shifts in obstetric
care and avoidance of in-hospital stays in public hospitals might be reflected by the reduced
delivery rate.19 Because of their previous pregnancy
experience, multiparous women might have been
more likely to modify antenatal appointments.
In contrast, women with mental illness require
greater antenatal care and psychosocial support.20
The establishment of virtual clinics for online
assessment without exposing pregnant women to
COVID-19 risk in clinical areas offers an important
alternative.21 To establish such clinics, antenatal
protocols must be revised to incorporate virtual
visits when ultrasounds, physical examinations, and
obstetric investigations are unnecessary. Pregnant
women would also require stable internet access, as
well as foetal doppler and blood pressure monitoring
equipment.
Working from home
Prior to and during the survey period, no complete
lockdowns were instituted in Hong Kong, although
working from home was encouraged. In this study,
slightly more than half of working women were
working from home after the COVID-19 alert.
There is a need to consider safety for women who
reported greater conflict with their husband/partner
while working from home. Increased domestic
violence was observed during the early stages of the
COVID-19 pandemic; greater relationship friction
and household conflict could be contributing
factors.22 Public policy should be revised to facilitate
the identification of women in need of conflict
assistance when physical and psychosocial support
may be limited because of physical isolation and the
suspension of community services.9 23
Behavioural adaptations
In this study, >90% of pregnant women reported
wearing a mask in clinical areas, although <10%
reported wearing an N95 mask in hospitals. Our
finding of 90% mask usage in clinical areas was much
greater than the 31.8% observed among the general
public in Taiwan in 2020.3 While the high rate of mask
use could represent compliance with hospital policies
regarding mandatory mask use and heightened
awareness of self-protection in pregnant women,
the use of N95 masks might also indicate a fear of
contacting COVID-19 in public hospitals where
confirmed cases were managed. Additionally, >20%
of the women either travelled abroad or returned to
Hong Kong because of COVID-19 risk. The history
of SARS outbreaks in Hong Kong might have led to
increased caution from the initial announcement of
the COVID-19 alert. Travel during pregnancy and
changes in delivery plans are important decisions.
In 2020, a study in China showed that women were
generally more anxious than men with respect to
COVID-19; greater perceived susceptibility and severity of COVID-19 were also associated with
greater anxiety.5 Obstetric decision-making and the
implementation of preventive measures have been
associated with antenatal anxiety secondary to the
COVID-19 pandemic.3 8 Quarantine can lead to
widespread and long-lasting adverse psychological
sequelae.24 In 2020, anxiety levels were significantly
higher among people who personally knew at least
one person with COVID-19.1 In our cohort, moderate
to marked emotional disturbance was reported by
two-thirds of women who had undergone quarantine
and one-third of women who had been living with
household members during home quarantine. There
is a need for supportive counselling to be provided to
this susceptible group of women.
Expectations of childbirth companionship
and peripartum services
Women’s expectations did not match changes in peripartum services and childbirth companionship;
these mismatches were greatest in married women.
Childbirth companionship provides multiple types
of physical and psychological support.25 Women of
Chinese ethnicity exhibited the greatest disagreement
with suspension of visiting hours. The principle
of “doing the month” in Chinese culture promotes
maternal rest with nutritious supplements; thus,
visits during the postpartum period are regarded
as essential convalescence for mothers and babies.26
In Hong Kong, a greater proportion of women had
a higher Edinburg Postpartum Depression Scale
score upon suspension of childbirth companionship
and visiting hours after announcement of the
COVID-19 alert.19 In 2020, a similar effect on the
Edinburg Postpartum Depression Scale score was
observed in a Turkish population.27 Importantly,
the Comprehensive Child Development Service in
public obstetric units provides a programme for the
identification, follow-up, and counselling of women
at risk of postpartum depression; this programme
constitutes critical support during stressful periods,
such as the COVID-19 pandemic.
Strengths and limitations
Likely because many women of reproductive age
living in Hong Kong remember the SARS outbreaks
in 2002-2003, a notable strength was that the present
study provided a useful assessment of adaptations
and responses to a similar disease (COVID-19). Such
valuable information can improve the understanding
of behaviour among pregnant women in places that
encounter further waves of COVID-19 transmission.
The merit of this survey was that the online
questionnaire format allowed respondents to
complete the questionnaire remotely and at their
preferred speed. The responses were automatically
captured in a database, which minimised entry errors and potential transmission of COVID-19.
However, this questionnaire format is limited to
patients with electronic access and does not permit
the involvement of an interviewer to explain the
questions. The use of convenience sampling in a
single centre might also have introduced bias and
limited the generalisability of the findings to the
general population.
An additional limitation was that only women
who continued antenatal follow-up or delivered in
our public hospital were included in the present
study. The delivery rate for January to April
decreased by 13% in 2020, compared with the same
period in 2019, despite a similar number of delivery
bookings.17 This phenomenon was observed across
all public hospitals in Hong Kong, indicating that
pregnant women might have chosen to deliver in
private hospitals instead. There is no standalone
maternity hospital in Hong Kong; all maternity
units are housed within general hospitals that admit
patients with COVID-19. We suspect that this
situation might have led some pregnant women to
deliver in private hospitals where they perceived the
risk of COVID-19 to be lower.
The final limitation was that the survey was
conducted during a non-peak period of COVID-19
transmission in 2020. Childbirth companionship
was resumed 2 days prior to the survey period;
companions were required to complete an
assessment of fever, travel, occupational exposure,
contact history, and clustering phenomenon. Thus,
the practices might have differed and the overall fear
of disease might have been less intense, compared
with a peak period of COVID-19 transmission.
Furthermore, the retrospective nature of this
study might have introduced recall bias, which
we attempted to minimise by providing a timeline
of key events concerning COVID-19 in the
information leaflet. However, the initial response of
the general public to COVID-19 might have been
exaggerated because accurate disease information
was limited during the early stages of the pandemic;
the performance of a questionnaire study during
a non-peak period might have helped to gather
less exaggerated data concerning the behaviour of
pregnant women. Further prospective longitudinal
studies can address how women respond in different
phases of the COVID-19 pandemic.
Conclusion
This study demonstrated the adaptations and
responses of pregnant women to the COVID-19
pandemic in Hong Kong. The women in this study
adjusted their obstetric appointments, began to
work from home, and practised protective measures
to reduce their risk of disease. While the overall
pregnancy experience was mostly improved by
working from home, women reported emotional disturbance because of the pandemic. Expectations
of obstetric services remained high, particularly
for Chinese women and nulliparous women.
Obstetricians and policymakers should attempt to
balance infection control and the peripartum needs
of pregnant women when modifying childbirth
companionship policies. Particular attention
to nulliparous women is needed because they
demonstrated higher levels of disagreement with the
suspension of antenatal and postnatal educational
programmes.
Author contributions
Concept or design: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: PW Hui.
Drafting of the manuscript: PW Hui.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: PW Hui.
Drafting of the manuscript: PW Hui.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank Ms WK Choi for her assistance with creation of the online survey and Mr G Chu for his assistance
with participant recruitment.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The research has been approved by Institutional Review Board of The University of Hong Kong/Hospital Authority
West Cluster (Ref UW 20-387).
References
1. Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J Psychiatr 2020;51:102076. Crossref
2. Wang C, Pan R, Wan X, et al. Immediate psychological
responses and associated factors during the initial stage
of the 2019 coronavirus disease (COVID-19) epidemic
among the general population in China. Int J Environ Res
Public Health 2020;17:1729. Crossref
3. Wong LP, Hung CC, Alias H, Lee TS. Anxiety symptoms
and preventive measures during the COVID-19 outbreak
in Taiwan. BMC Psychiatry 2020;20:376. Crossref
4. Corbett GA, Milne SJ, Hehir MP, Lindow SW,
O’Connell MP. Health anxiety and behavioural changes of
pregnant women during the COVID-19 pandemic. Eur J
Obstet Gynecol Reprod Biol 2020;249:96-7. Crossref
5. Lin Y, Hu Z, Alias H, Wong LP. Knowledge, attitudes,
impact, and anxiety regarding COVID-19 infection among
the public in China. Front Public Health 2020;8:236. Crossref
6. Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19
outbreak in a population sample in the northern Spain [in
Spanish]. Cad Saude Publica 2020;36:e00054020.
7. Kotlyar AM, Grechukhina O, Chen A, et al. Vertical
transmission of COVID-19: a systematic review and meta-analysis.
Am J Obstet Gynecol 2020;224:35-53.e3.
8. Liu X, Chen M, Wang Y, et al. Prenatal anxiety and
obstetric decisions among pregnant women in Wuhan
and Chongqing during the COVID-19 outbreak: a cross-sectional
study. BJOG 2020;127:1229-40. Crossref
9. Thapa SB, Mainali A, Schwank SE, Acharya G. Maternal
mental health in the time of the COVID-19 pandemic.
Acta Obstet Gynecol Scand 2020;99:817-8. Crossref
10. Wu Y, Zhang C, Liu H, et al. Perinatal depressive and
anxiety symptoms of pregnant women along with COVID-19 outbreak in China. Am J Obstet Gynecol 2020;223:240.e1-9.
11. Westgren M, Pettersson K, Hagberg H, Acharya G.
Severe maternal morbidity and mortality associated with
COVID-19: the risk should not be downplayed. Acta
Obstet Gynecol Scand 2020;99:815-6. Crossref
12. Leung GM, Cowling BJ, Wu JT. From a sprint to a marathon
in Hong Kong. N Engl J Med 2020;382:e45.
13. To KK, Yuen KY. Responding to COVID-19 in Hong Kong.
Hong Kong Med J 2020;26:164-6.
14. Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ.
Decline of acute coronary syndrome admissions in Austria
since the outbreak of COVID-19: the pandemic response
causes cardiac collateral damage. Eur Heart J 2020;41:1852-3. Crossref
15. Teo KC, Leung WC, Wong YK, et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke
2020;51:2228-31. Crossref
16. Marijon E, Karam N, Jost D, et al. Out-of-hospital cardiac
arrest during the COVID-19 pandemic in Paris, France:
a population-based, observational study. Lancet Public
Health 2020;5:e437-43.
17. Vogel JP, Habib NA, Souza JP, et al. Antenatal care packages with reduced visits and perinatal mortality: a secondary analysis of the WHO Antenatal Care Trial. Reprod Health
2013;10:19. Crossref
18. Mohamed Shaker El-Sayed Azzaz A, Martínez-Maestre MA,
Torrejón-Cardoso R. Antenatal care visits during
pregnancy and their effect on maternal and fetal outcomes
in pre-eclamptic patients. J Obstet Gynaecol Res
2016;42:1102-10. Crossref
19. Hui PW, Ma G, Seto MT, Cheung KW. Effect of COVID-19
on delivery plan and postnatal depression score of pregnant
women. Hong Kong Med J 2021;27:113-7.
20. Berthelot N, Lemieux R, Garon-Bissonnette J, Drouin-Maziade C, Martel É, Maziade M. Uptrend in distress and psychiatric symptomatology in pregnant women during
the coronavirus disease 2019 pandemic. Acta Obstet
Gynecol Scand 2020;99:848-55. Crossref
21. Aziz A, Zork N, Aubey JJ, et al. Telehealth for high-risk
pregnancies in the setting of the COVID-19 pandemic. Am
J Perinatol 2020;37:800-8. Crossref
22. Roesch E, Amin A, Gupta J, García-Moreno C. Violence against women during COVID-19 pandemic restrictions.
BMJ 2020;369:m1712.
23. Usher K, Bhullar N, Durkin J, Gyamfi N, Jackson D.
Family violence and COVID-19: increased vulnerability
and reduced options for support. Int J Ment Health Nurs
2020;29:549-52. Crossref
24. Brooks SK, Webster RK, Smith LE, et al. The psychological
impact of quarantine and how to reduce it: rapid review of
the evidence. Lancet 2020;395:912-20. Crossref
25. Bohren MA, Berger BO, Munthe-Kaas H, Tunçalp Ö.
Perceptions and experiences of labour companionship:
a qualitative evidence synthesis. Cochrane Database Syst
Rev 2019;(3):CD012449.
26. Liu YQ, Maloni JA, Petrini MA. Effect of postpartum
practices of doing the month on Chinese women’s physical
and psychological health. Biol Res Nurs 2014;16:55-63. Crossref
27. Durankuş F, Aksu E. Effects of the COVID-19 pandemic
on anxiety and depressive symptoms in pregnant women:
a preliminary study. J Matern Fetal Neonatal Med
2020;35:205-11. Crossref