Hong Kong Med J 2022 Aug;28(4):334.e1–3
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Abdominal para-aortic ectopic thyroid tissue
mimicking lymphadenopathy on computer tomography
Charmaine HK Wong, MB, ChB, FRCR1; HL Tsui, MB, ChB, FHKAM (Radiology)1; CN Ling, MB, ChB2; Anthony WT Chin, MB, ChB, FHKAM (Radiology)1; PY Chu, MB, ChB, FHKAM (Radiology)1; CS Chan, MB, BS, FHKAM (Radiology)1
1 Department of Radiology and Organ Imaging, United Christian Hospital, Hong Kong
2 Department of Pathology, United Christian Hospital, Hong Kong
Corresponding author: Dr Charmaine HK Wong (charmainehwong@gmail.com)
A 70-year-old woman presented to our hospital for workup for chronic cough. A contrast computed
tomography (CT) of the thorax and abdomen
revealed an incidental finding of multilobulated
soft tissue lesions in the abdomen along the left
para-aortic region. The lesions measured up to
7.4 cm in diameter and demonstrated mild
increased attenuation on pre-contrast images and
vivid heterogenous enhancement on post-contrast
study (Fig 1a and b). Appearance and location
of these lesions raised concern about possible
lymphadenopathy so fluorodeoxyglucose-18
positron emission tomography–CT was performed.
The lesions demonstrated only mild metabolic
activity (maximal standard uptake value=2.6)
[Fig 1c]. They showed no interval change in
appearance, and no other hypermetabolic lesion
could be detected elsewhere. Tumour markers
including alpha-fetoprotein, carcinoembryonic
antigen, and cancer antigen 125 were not elevated.
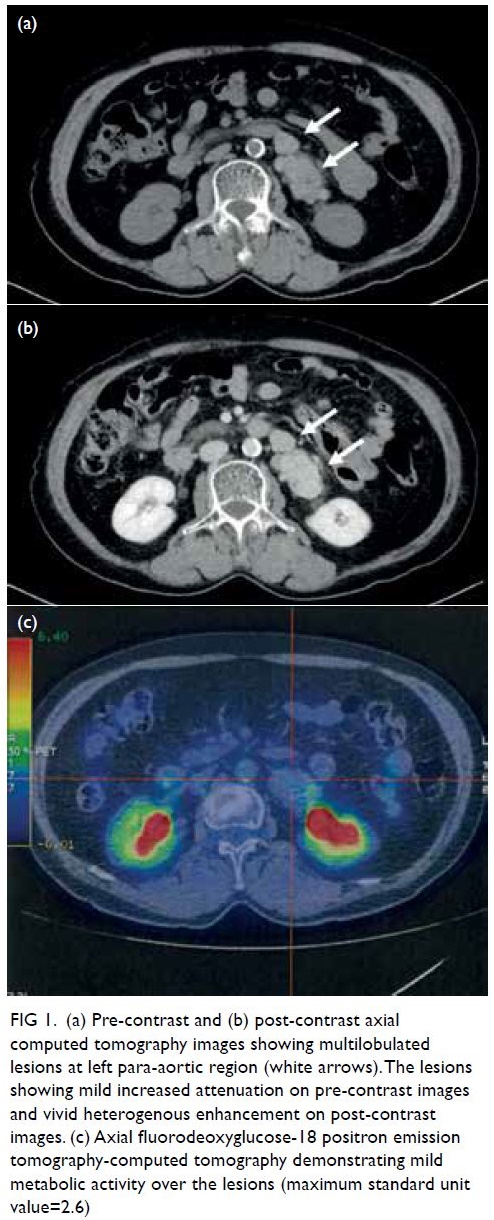
Figure 1. (a) Pre-contrast and (b) post-contrast axial computed tomography images showing multilobulated lesions at left para-aortic region (white arrows). The lesions showing mild increased attenuation on pre-contrast images and vivid heterogenous enhancement on post-contrast images. (c) Axial fluorodeoxyglucose-18 positron emission tomography-computed tomography demonstrating mild metabolic activity over the lesions (maximum standard unit value=2.6)
The CT-guided biopsy of the para-aortic
lesions subsequently showed cuboidal follicular
cells arranged in architecture resembling thyroid
parenchymal tissue (Fig 2). Immunostaining for
thyroglobulin and thyroid transcription factor-1
were positive. There were no nuclear features of
carcinoma.
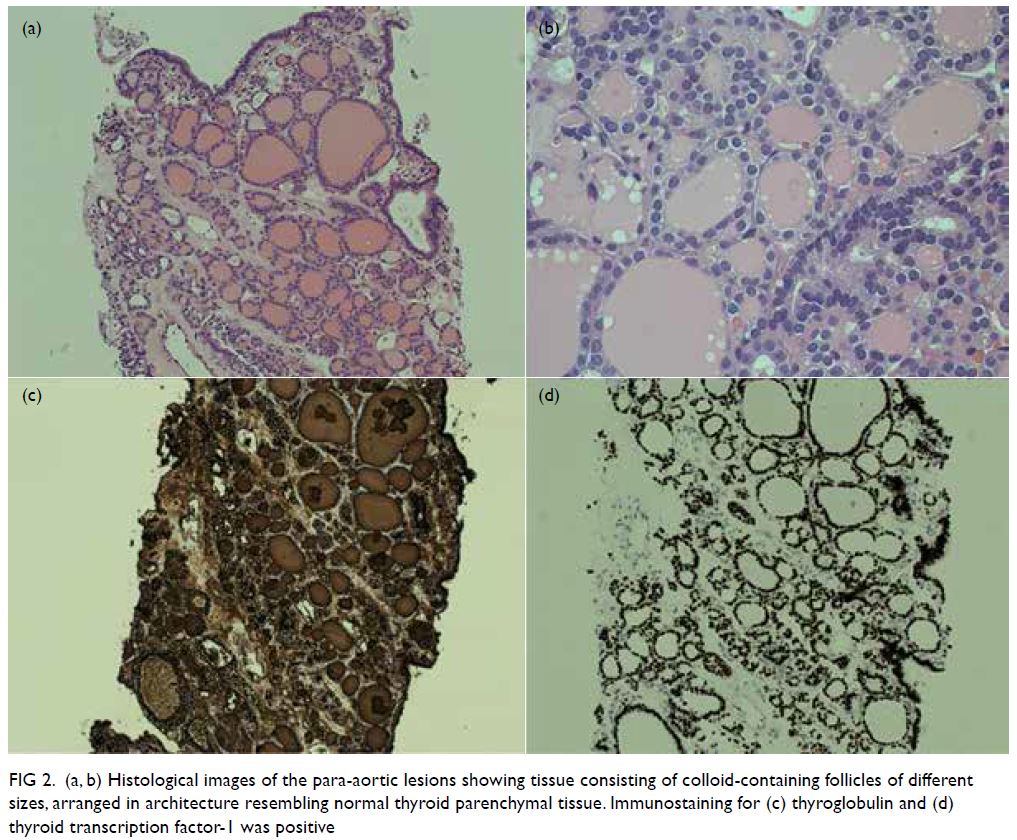
Figure 2. (a, b) Histological images of the para-aortic lesions showing tissue consisting of colloid-containing follicles of different sizes, arranged in architecture resembling normal thyroid parenchymal tissue. Immunostaining for (c) thyroglobulin and (d) thyroid transcription factor-1 was positive
Thyroid scintigraphy using technetium-99m
pertechnetate showed intense radiotracer uptake
over the corresponding para-aortic lesions (Fig 3).
Findings were consistent with ectopic thyroid tissue.
The presence of an orthotopic thyroid at its normal
pretracheal position was demonstrated on CT
and on technetium-99m scan (Fig 4). The patient’s
thyroid function was normal.
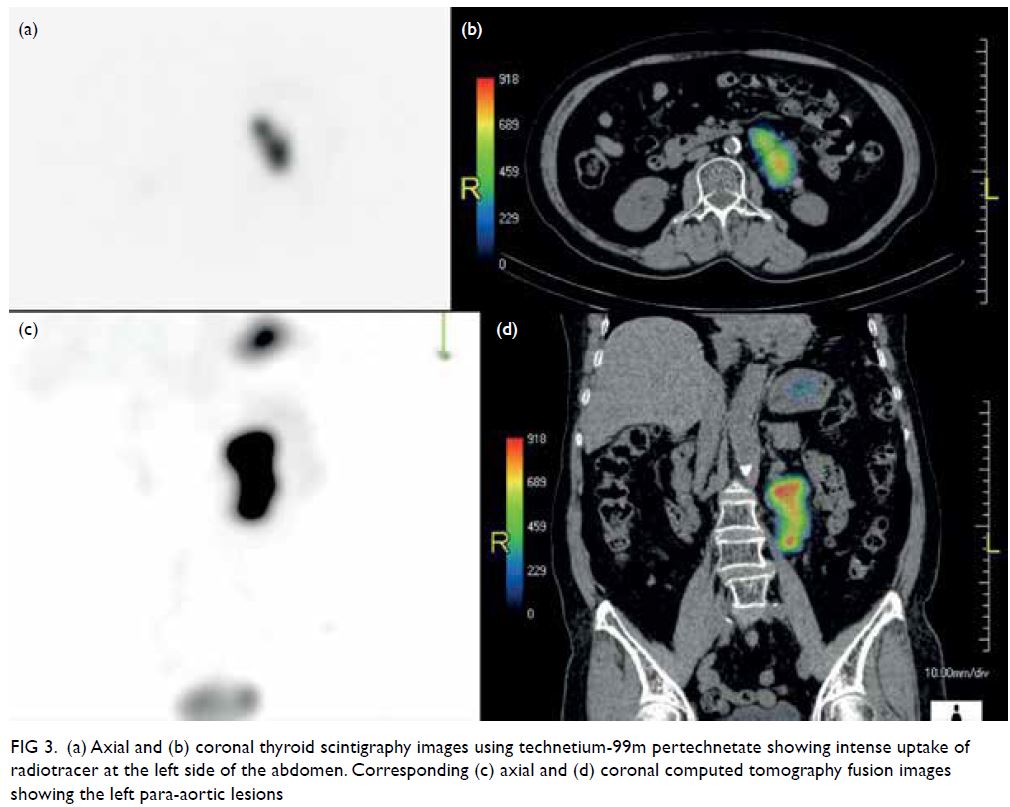
Figure 3. (a) Axial and (b) coronal thyroid scintigraphy images using technetium-99m pertechnetate showing intense uptake of radiotracer at the left side of the abdomen. Corresponding (c) axial and (d) coronal computed tomography fusion images showing the left para-aortic lesions
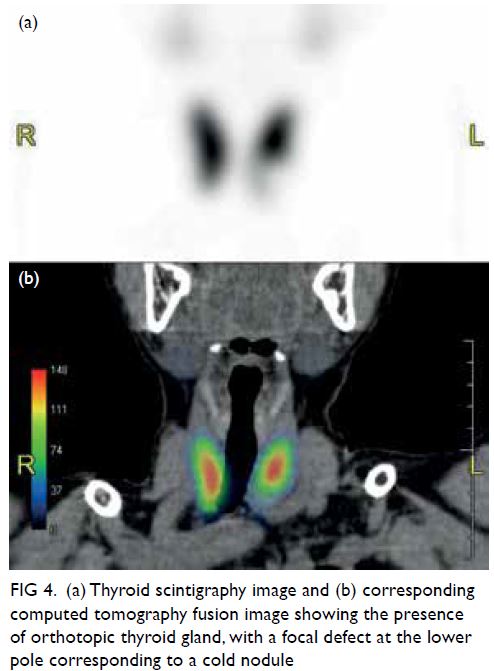
Figure 4. (a) Thyroid scintigraphy image and (b) corresponding computed tomography fusion image showing the presence of orthotopic thyroid gland, with a focal defect at the lower pole corresponding to a cold nodule
Ectopic thyroid gland is a rare developmental
abnormality with a prevalence of approximately 1
per 100 000 to 300 000 population.1 It results from
aberrant embryogenesis of the gland during its
migration from the foramen cecum at the posterior
aspect of the tongue to its final pretracheal position.
Frequent locations include its path of embryological
descent along the midline of the neck, with a
lingual thyroid at the base of the tongue being most
common, accounting for up to 90% of reported
cases.2 Other locations include the lateral neck
and superior mediastinum. More distant locations
such as subdiaphragmatic locations have also been reported but are exceedingly rare. To the best of
the authors’ knowledge, this is the first report of
ectopic thyroid tissue occurring at the para-aortic
region of the abdomen, mimicking the appearance
of lymphadenopathy on CT.
Thyroid scintigraphy is the most important and
sensitive imaging tool to detect ectopic thyroid tissue.
It also has the advantage of being able to demonstrate
the presence or absence of an orthotopic thyroid
gland. In patients with ectopic thyroid tissue, it is
important to evaluate for the presence of orthotopic
thyroid and thyroid function. Hypothyroidism may
be present, particularly in those without a normal
thyroid gland, and more common in patients with
lingual ectopic thyroid.2 Ultrasound is also useful to
locate and evaluate the orthotopic thyroid gland.
Computed tomography and magnetic
resonance imaging are important adjuncts in
evaluation. Ectopic thyroid tissue may show similar
imaging characteristics to normal thyroid gland with
high attenuation on non-contrast CT due to its high
iodine content and vivid post-contrast enhancement.
When ectopic thyroid tissue is found in a location
not consistent with embryologic development, the possibility of malignant metastasis needs to be
considered, occurring in 7% to 23% of patients.3
Biopsy is invaluable and the orthotopic gland
should be evaluated for possible malignant change.
Pathological changes that affect a normal thyroid
including malignant change have been reported in
ectopic tissues,1 and should be considered in the
management and follow-up of ectopic thyroid tissue.
Author contributions
Concept or design: All authors.
Acquisition of data: CHK Wong, HL Tsui, CN Ling.
Analysis or interpretation of data: CHK Wong, HL Tsui, CN Ling.
Drafting of the manuscript: CHK Wong, HL Tsui, CN Ling.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: CHK Wong, HL Tsui, CN Ling.
Analysis or interpretation of data: CHK Wong, HL Tsui, CN Ling.
Drafting of the manuscript: CHK Wong, HL Tsui, CN Ling.
Critical revision of the manuscript for important intellectual content: All authors.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki. The patient provided written informed consent
for all treatments and procedures and consent for publication.
References
1. Noussios G, Anagnostis P, Goulis DG, Lappas D, Natsis K.
Ectopic thyroid tissue: anatomical, clinical, and
surgical implications of a rare entity. Eur J Endocrinol
2011:165:375-82. Crossref
2. Guerra G, Cinelli M, Mesolella M, et al. Morphological,
diagnostic and surgical features of ectopic thyroid gland: a
review of literature. Int J Surg 2014;12 Suppl 1:S3-11. Crossref
3. Ballard D, Patel P, Schild SD, Ferzli G, Gordin E. Ectopic
thyroid presenting as supraclavicular mass: a case report
and literature review. J Clin Transl Endocrinol Case Rep
2018;10:17-20. Crossref

