Hong Kong Med J 2022 Aug;28(4):285–93 | Epub 21 Jan 2022
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Stillbirth rate in singleton pregnancies: a 20-year
retrospective study from a public obstetric unit in Hong Kong
Sani TK Wong, MB, ChB; WT Tse, MB, ChB, MRCOG; SL Lau, MB, ChB, MRCOG; Daljit S Sahota, PhD; TY Leung, MD, FRCOG
Department of Obstetrics and Gynaecology, The Chinese University of Hong Kong, Hong Kong
Corresponding author: Prof TY Leung (tyleung@cuhk.edu.hk)
Abstract
Introduction: Although the stillbirth rate is
low in Hong Kong, up to 50% of stillbirths have
unclassifiable causes and up to one third of stillbirths
have unexplained causes. This retrospective study
investigated the underlying causes of singleton
stillbirths in Hong Kong.
Methods: This study examined the prevalences and
causes of stillbirths in a university tertiary obstetric
unit between 2000 and 2019. Medical records were
reviewed for all singleton pregnancies complicated
by stillbirths. Causes of stillbirth were determined
via clinical assessments and laboratory findings,
then compared between 2000-09 and 2010-19.
Results: Overall perinatal mortality significantly
decreased by 16.7%, from 5.50/1000 in 2000-09 to
4.59/1000 in 2010-19; the singleton stillbirth rate
slightly decreased (from 3.27/1000 to 2.91/1000).
These changes were related to early prenatal
diagnostic improvements concerning congenital
malformations and genetic disorders. Pre-eclampsia
prevalence among singleton pregnancies increased
from 1.5% to 1.7% because of increasing maternal
age; the stillbirth rate among patients with pre-eclampsia
decreased from 2.5% to 1.4%. Foetal
growth restriction of unknown cause contributed to 16% of all stillbirths; this prevalence did not change
over time. Moreover, foetal growth restriction was
not diagnosed during routine antenatal care in 43.5%
of patients. Thirty-six percent of all stillbirths were
unexplained. The prevalences of stillbirth associated
with chorioamnionitis and placental abruption did
not change over time.
Conclusions: Causes of stillbirth in Hong Kong have changed in the past 20 years because of altered
demographic characteristics and improved prenatal
testing. Further improvements should focus on
early foetal growth restriction detection and preeclampsia
prevention.
New knowledge added by this study
- The stillbirth rate among singleton pregnancies in Hong Kong is declining (from 3.27/1000 in 2000-09 to 2.91/1000 in 2010-19), mainly because of reductions in congenital malformations and genetic diseases.
- Pre-eclampsia is becoming more prevalent (from 1.5% in 2000-09 to 1.7% in 2010-19), although the pre-eclampsia–related stillbirth rate has decreased (from 2.5% to 1.4%).
- Foetal growth restriction (FGR) remains a common cause of stillbirths (16% of all stillbirths), and 43.5% of FGR-related stillbirths were undiagnosed during routine antenatal care.
- Primary prevention of pre-eclampsia through first trimester screening and aspirin prophylaxis is essential for improving maternal and foetal health.
- Antenatal detection of FGR should be improved using more accurate sonographic and biochemical tests.
- Territory-wide perinatal mortality monitoring is important for maintaining the standard of perinatal care in Hong Kong.
Introduction
Compared with many other regions worldwide,
Hong Kong has one of the lowest perinatal mortality
rates, defined as the total number of stillbirths and
early neonatal deaths per 1000 births.1 Worldwide,
there are consistent definitions of early and late neonatal deaths (ie, the death of a livebirth in the first
7 days and 28 days after birth, respectively); however,
the definition of stillbirth varies among regions.
Hong Kong has been using the United Kingdom’s
definition of stillbirth, which is ‘a baby delivered with
no signs of life at or after 24 weeks of gestation’.1 In contrast, some countries use 20 weeks, 22 weeks, or
500 g as a threshold for stillbirth.2 To facilitate global
comparisons, the World Health Organization has
stratified stillbirth into early (death at a birthweight
>500 g or at a gestational age ≥22 weeks) and late
foetal death (death at a birthweight ≥1000 g or at a
gestational age ≥28 weeks).3
The estimated global stillbirth rate was
18.4/1000 births in 2015.4 Estimated stillbirth
rates are significantly lower in developed countries
(approximately 3.4/1000 births); the highest stillbirth
rate has been reported in sub-Saharan Africa regions
(28.7/1000 births).4 Intrapartum stillbirths comprise
up to 57% of all reported stillbirths in South Asia;
most are related to obstetric emergencies.5 Thus, the
stillbirth rate is a potential indicator of a country’s
healthcare system quality; variations in intrapartum
stillbirth rates among countries may reflect the
readiness of health facilities to provide adequate
intrapartum care and ensure that trained birth
attendants are available for delivery.5 Therefore, the
United Nations has included stillbirth prevention as
a major Sustainable Development Goal.6
The stillbirth rate is consistently low in
Hong Kong (2/1000 births during the period from
2004 to 2014).1 However, up to 50% of stillbirths
have unclassifiable causes and up to one third of
stillbirths have unexplained causes, which may
reflect inconsistencies and limitations regarding the different coding systems that are used by obstetric
units in Hong Kong.
This study was performed to review the
overall perinatal mortality in a tertiary centre in
Hong Kong, and specifically explored the causes,
the associated risk factors and trends of stillbirth in
singleton pregnancies. Neonatal deaths and perinatal
mortalities in multiple pregnancies will be reported
separately.
Methods
Study setting
This study retrospectively reviewed data collected
from 1 January 2000 to 31 December 2019, in the
Prince of Wales Hospital in Hong Kong. The hospital
serves a population of approximately 1.7 million
in the New Territories East region of Hong Kong,
with an annual delivery rate of approximately 6000
to 7000 births. The obstetric unit is also a tertiary
centre that receives complicated maternal and foetal
cases referred from other hospitals as well as a
maternal foetal medicine training centre accredited
by both The Royal College of Obstetricians and
Gynaecologists (https://www.rcog.org.uk) and
The Hong Kong College of Obstetricians and
Gynaecologists (www.hkcog.org.hk). The standard
antenatal and obstetric care, as well as the
investigation of stillbirth and neonatal death are
described in the Supplementary Appendix.
Data collection and analysis
Data of all deliveries including maternal demographic data (eg, ethnicity, maternal age, height, body weight,
body mass index [BMI], underlying medical diseases,
and obstetric history), obstetric and perinatal
outcomes were retrieved from a hospital-specific
Obstetric Specialty Clinical Information System that
is used to record maternal and perinatal outcomes
after birth.7 Stillbirths (defined as foetal death that
occurred at or after 24 weeks; late stillbirth occurred
at or after 28 weeks)3 were identified from the
database and their details were further retrieved
from hospital electronic records. All stillbirths
were included regardless of their booking status
or whether their deaths were occurred before
admission to our unit; however, the booking status
was incorporated into the analysis.
The stillbirth rate was calculated as the number
of stillbirths divided by the total number of births
(after 24 weeks). The stillbirth rates of singleton
pregnancies were compared between 2000-09 and
2010-19.
Statistical analysis
Continuous variables were compared by the
independent samples t test or Mann-Whitney
U test for parametric and non-parametric data, respectively. Categorical variables were compared
by the Chi squared test or Fisher’s exact test, as
appropriate. The level of significance was set at
a two-sided P value of <0.05. Data analysis was
performed using SPSS (Windows version 22.0; IBM
Corp, Armonk [NY], United States).
Results
Mortality during the study period
During the 20-year study period, there were 128 967
babies delivered. Among them were 429 stillbirths,
159 early neonatal deaths, and 59 late neonatal
deaths. The total mortality rate was 5.02 per 1000
births and the perinatal mortality rate was 4.56 per
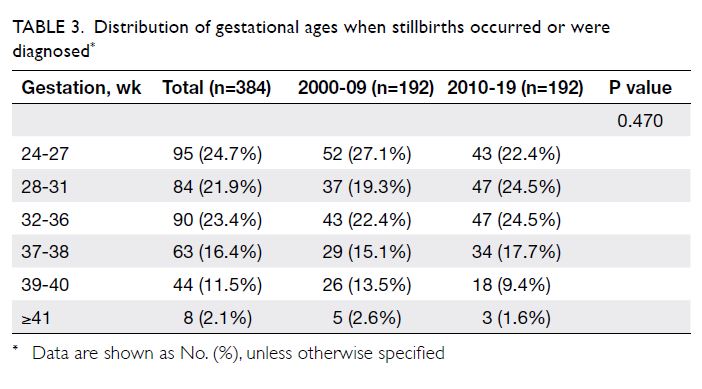
1000 births. The total mortality rate was significantly
lower during 2010-19 than during 2000-09 (4.59
per 1000 births vs 5.50 per 1000 births; P=0.023).
The perinatal mortality rate was also significantly
lower in 2010-19 (4.18 per 1000 births vs 5.00 per
1000 births; P=0.035), although the rates of stillbirths
and late stillbirths were not significantly different
between 2000-09 and 2010-19 (Table 1).
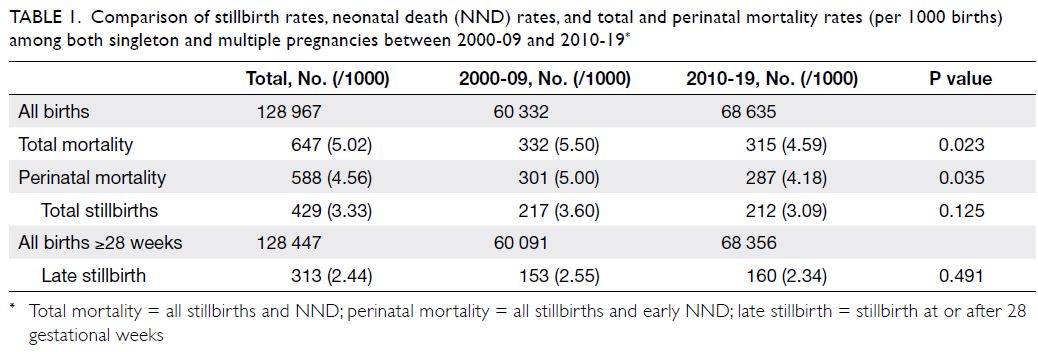
Table 1. Comparison of stillbirth rates, neonatal death (NND) rates, and total and perinatal mortality rates (per 1000 births) among both singleton and multiple pregnancies between 2000-09 and 2010-19
Table 2 shows all mortality data for singleton
pregnancies. Among 124 665 singleton babies,
the respective total mortality, perinatal mortality
and stillbirth rates were 4.56/1000, 4.17/1000 and
3.08/1000. Among the 384 singleton stillbirths, 95 (24.7%) occurred between 24 and 27 weeks,
while 289 (75.3%) occurred thereafter; thus, the
late stillbirth rate was 2.33/1000. The detailed
distribution of gestational ages among stillbirths
is shown in Table 3. There were 23 (6%) cases of
intrapartum death (0.18/1000 births); these were
caused by placental abruption (n=11), known lethal
foetal anomalies (n=7), chorioamnionitis (n=2),
uterine rupture (n=1), maternal diabetic ketoacidosis
(n=1), and umbilical cord accident—cord ulceration
related to duodenal atresia (n=1).8
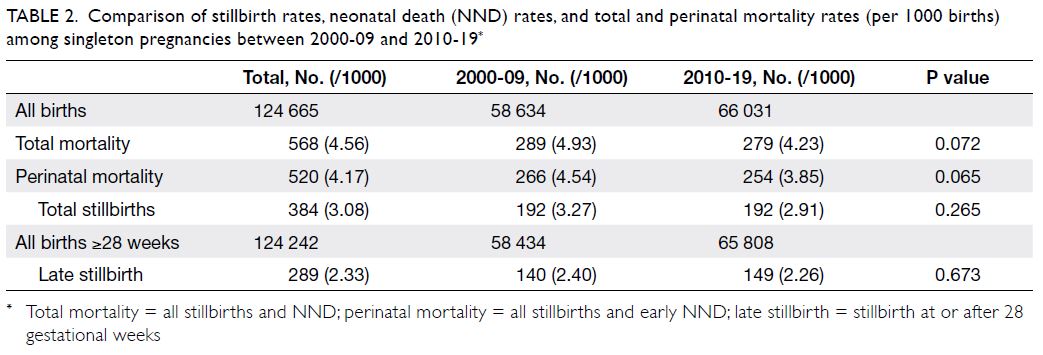
Table 2. Comparison of stillbirth rates, neonatal death (NND) rates, and total and perinatal mortality rates (per 1000 births) among singleton pregnancies between 2000-09 and 2010-19
Singleton stillbirths: causes and potential risk
factors
Table 4 shows the direct causes of the 384 singleton stillbirths that occurred during the study period.
The most common leading cause was foetal
growth restriction (FGR) [n=61, 15.9% of singleton
stillbirths]; 41 of these 61 cases (67.2%) were not
diagnosed before birth. The next most common
leading causes were chorioamnionitis (n=43, 11.2%
of singleton stillbirths), congenital malformations
and genetic abnormalities (n=35, 9.1% of singleton
stillbirths), placental abruption (n=31, 8.1% of
singleton stillbirths), and pre-eclampsia (n=24, 6.3%
of singleton stillbirths). Pre-eclampsia also occurred
in 11 cases of placental abruption, one case of genetic abnormality (Haemoglobin Barts), and one case of
chorioamnionitis; importantly, pre-eclampsia was
not regarded as the leading cause in these 13 cases.
There were 139 unexplained stillbirths and
comprised about one third of all singleton stillbirths.
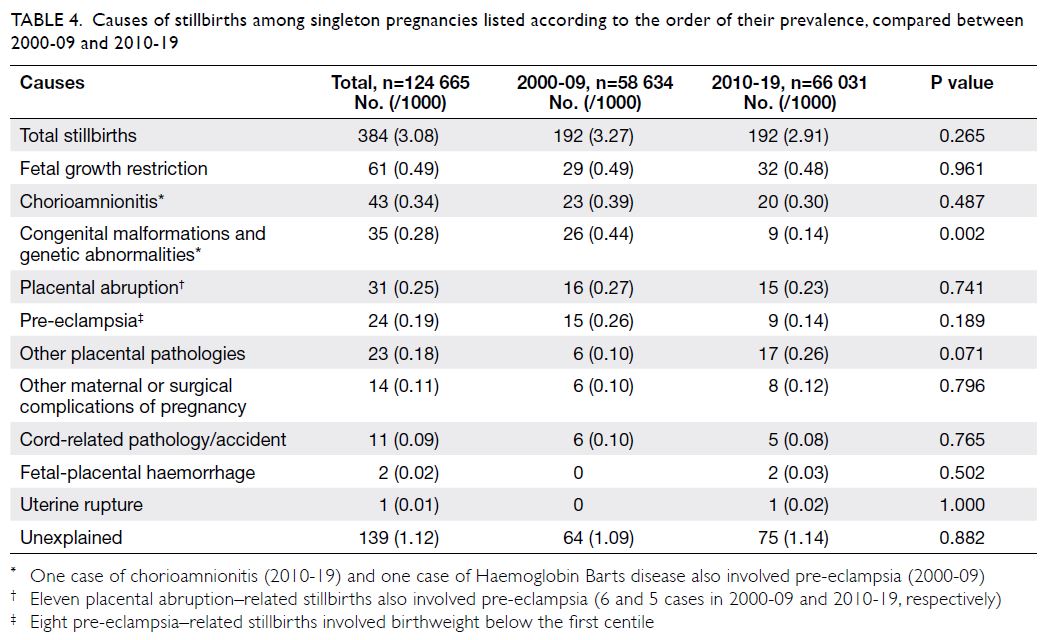
Table 4. Causes of stillbirths among singleton pregnancies listed according to the order of their prevalence, compared between 2000-09 and 2010-19
Table 5 shows the maternal characteristics for
all stillbirths and for the subgroups of unexplained
stillbirths and FGR-related stillbirths in singleton
pregnancies. Compared with mothers in the
livebirth group (excluding neonatal death), mothers
in the stillbirth group were significantly older
(30.7 ± 5.5 years vs 31.8 ± 5.8 years; P<0.001); greater
proportions of mothers in the stillbirth group had
advanced maternal age ≥35 years (24.1% vs 33.3%;
P<0.001) and ≥40 years (3.9% vs 6.8%; P=0.004).
Mothers in the stillbirth group also had higher BMI at booking (22.8 ± 3.6 kg/m2 vs 23.4 ± 3.9 kg/m2;
P=0.003); greater proportions of mothers in the
stillbirth group had BMI ≥30 kg/m2 (3.7% vs 6.3%;
P=0.012). The prevalences of nulliparity (52.2% vs
57.7%; P=0.027), non-booked status (8.0% vs 22.9%,
P<0.001), and non-Chinese Asian ethnicity (2.6%
vs 5%; P=0.018) were also significantly higher in
the stillbirth group. In the unexplained stillbirth
subgroup, only nulliparity and non-booked status
remained significant risk factors. In the FGR-related
stillbirth subgroup, the mothers were more likely
to be non-Chinese, non-booked cases, nulliparous,
older, and obese (BMI ≥30 kg/m2).
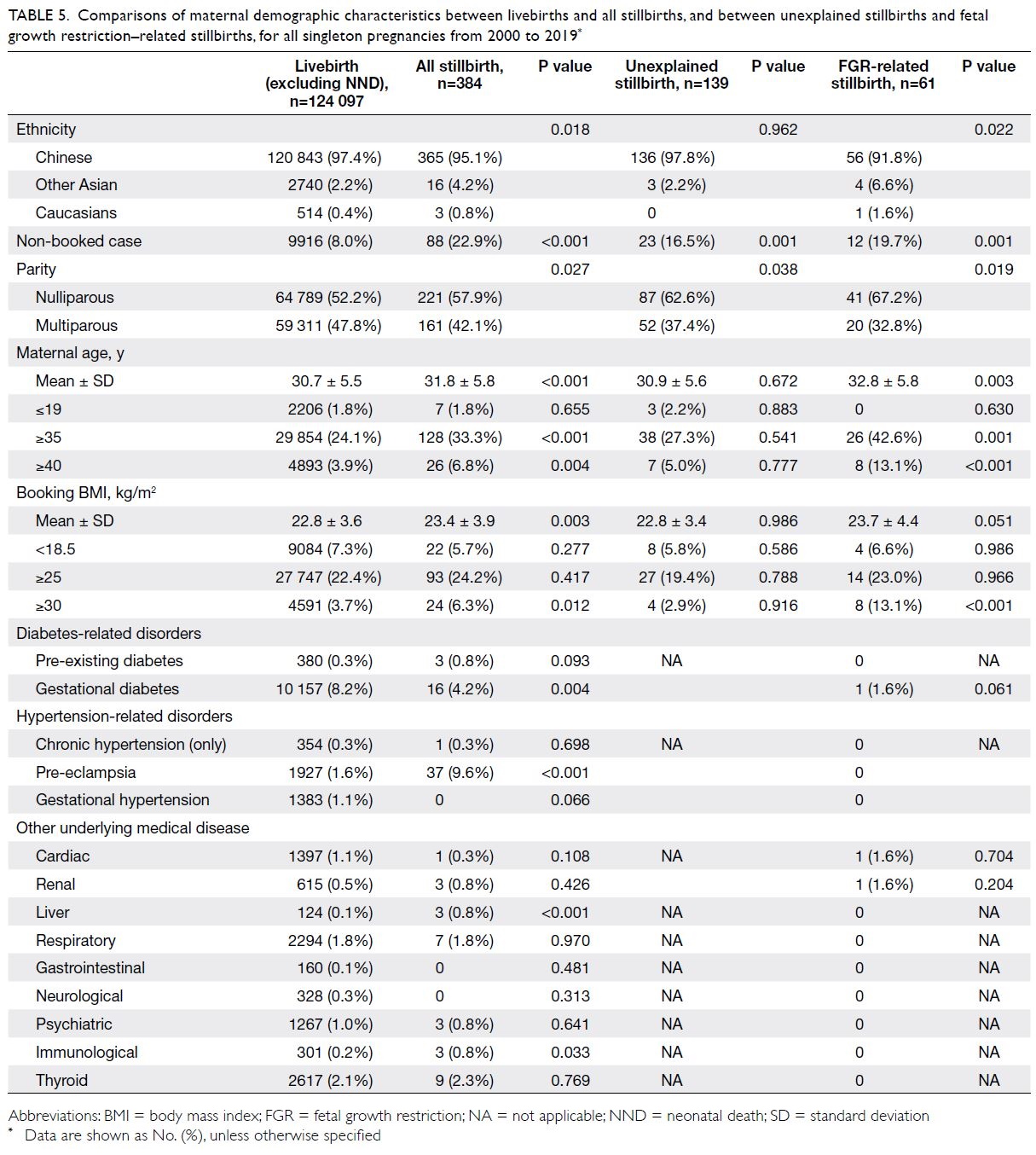
Table 5. Comparisons of maternal demographic characteristics between livebirths and all stillbirths, and between unexplained stillbirths and foetal growth restriction–related stillbirths, for all singleton pregnancies from 2000 to 2019
Compared with the livebirth group, the
prevalences of several medical diseases were also
higher in the stillbirth group, including pre-eclampsia
(1.6% vs 9.6%; P<0.001), liver diseases (0.1% vs 0.8%;
P<0.001), and immunological diseases (0.2% vs 0.8%;
P=0.033). However, histories of other pre-existing
medical condition such as diabetes and chronic
hypertension were not associated with stillbirth.
There was a lower prevalence of gestational diabetes
(8.2% vs 4.2%; P=0.004) in the stillbirth group.
Changes in stillbirth causes and risk factors
over time
Comparing 2000-09 and 2010-19, there was a trend
towards reduction in stillbirth rate (3.27/1000 vs
2.91/1000; P=0.265), although this difference was
not statistically significant. Among the direct causes
of stillbirths, there was a significant reduction in
the prevalence of congenital malformations and genetic abnormalities (0.44/1000 vs 0.14/1000;
P=0.002). There was a trend towards reduction
in pre-eclampsia–related stillbirths (0.26/1000 vs
0.14/1000; P=0.189), although this difference was
not statistically significant. There was an increasing
trend of singleton stillbirths related to other placental
pathologies although it did not reach statistical significance (0.10/1000 vs 0.26/1000; P=0.071). The
prevalences of FGR, chorioamnionitis, placental
abruption, other maternal or surgical complications
of pregnancy, cord-related pathology/accident,
foetal-placental haemorrhage, uterine rupture, and
unexplained stillbirth did not change over time
(Table 4).
Between 2000-09 and 2010-19, there were
several significant changes in maternal demographics
(Table 6), including a higher maternal age over time
(29.9 ± 5.3 years vs 31.4 ± 5.6 years; P<0.001); in
2010-19, a greater proportion of mothers had
advanced maternal age ≥35 years (20.2% vs 27.6%;
P<0.001) and ≥40 years (3.2% vs 4.7%; P<0.001).
The mean booking BMI was significantly reduced
in 2010-19 (22.9 ± 3.6 kg/m2 vs 22.6 ± 3.6 kg/m2;
P<0.001), with greater prevalence of underweight
(BMI at booking <18.5 kg/m2; 6.7% vs 7.9%; P<0.001),
although a greater prevalence of obesity was also
observed (BMI at booking >30 kg/m2; 3.6% vs 3.8%,
P=0.01) [Table 6]. The prevalence of non-booked
cases was also significantly reduced (13.6% vs 3.1%;
P<0.001). Chinese ethnicity remained dominant
(97.2% vs 97.5%; P<0.001) and the proportions of
nulliparous mothers were similar (52.5% vs 52.0%;
P=0.065). In 2010-19, there were higher prevalence
of pre-existing diabetes (0.3% vs 0.4%; P=0.001),
gestational diabetes (6.7% vs 9.4%; P<0.001),
chronic hypertension (0.1% vs 0.4%; P<0.001) and
gestational hypertension (0.4% vs 1.8%; P<0.001);
the caesarean delivery rate also increased (21.2% vs
23.2%; P<0.001). Other changes in the prevalences of
medical diseases are summarised in Table 6.
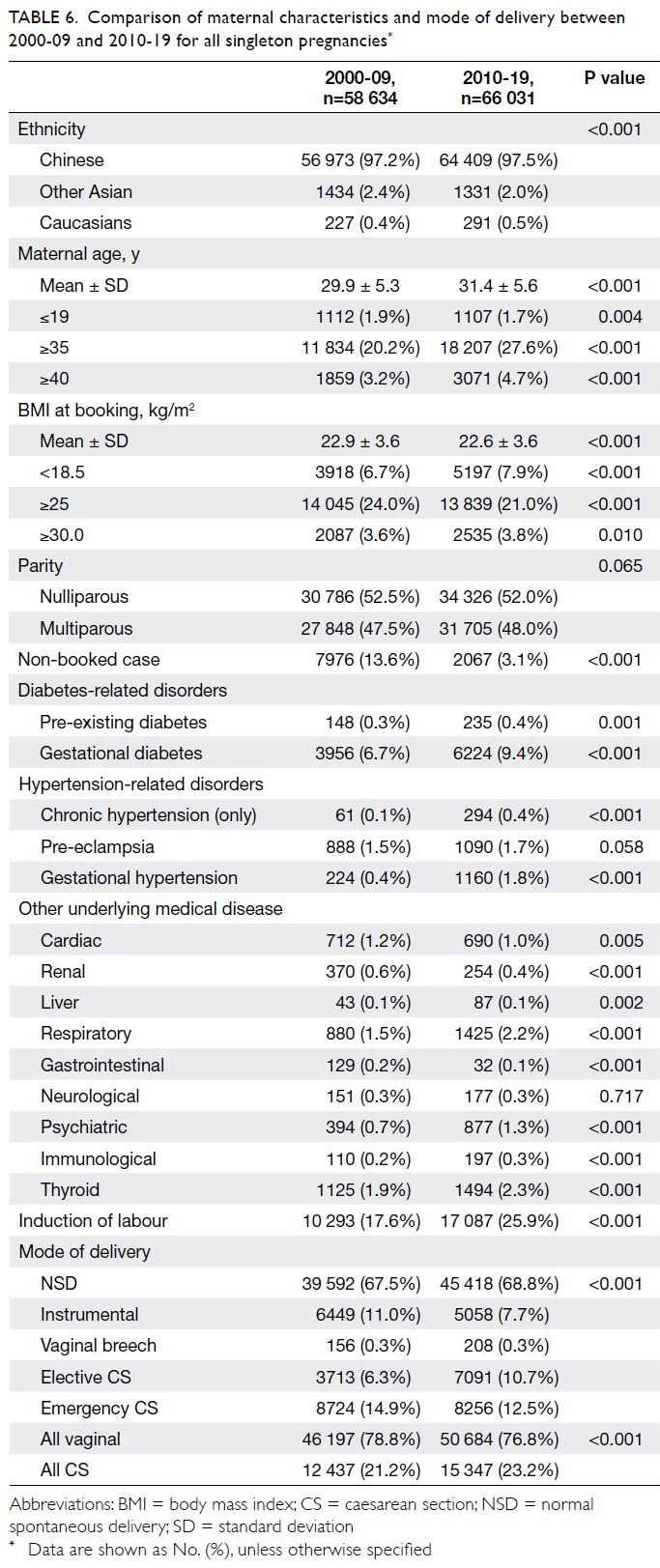
Table 6. Comparison of maternal characteristics and mode of delivery between 2000-09 and 2010-19 for all singleton pregnancies
Discussion
Changes in perinatal mortality
This investigation of perinatal mortality in Hong
Kong showed that the overall perinatal mortality
rate was significantly reduced by 16.7% from
5.50/1000 in 2000-09 to 4.59/1000 in 2010-19. This
is a combined effect of reductions in stillbirths and
neonatal deaths, although these individual trends
(ie, rates of stillbirth and neonatal death) were not
significantly different over time. Compared with the
stillbirth rate of 4.44/1000 reported by our unit in
1994,9 we observed gradual declines to 3.60/1000
in 2000-09 and 3.09/1000 in 2010-19. Because our
hospital is a tertiary referral centre, it is reasonable
that our stillbirth rate is slightly higher than the rate
determined in a territory-wide audit performed
by the Hong Kong College of Obstetricians and
Gynaecologists (2/1000 births).1
The intrapartum death rate in Hong Kong was
considerably reduced from 0.96/1000 (22% of all
stillbirths) in the 1990s9 to 0.2/1000 in the present
study; intrapartum deaths only comprised 6% of
all stillbirths in our cohort. Our findings compare
favourably with the reported mean intrapartum
rates of 0.9/1000 and 7/1000 in developed and
developing countries, respectively, during the mid-2000s.10 Furthermore, approximately one third of
our intrapartum stillbirths involved congenital lethal
malformations; the patients had not undergone
intrapartum foetal monitoring and no active resuscitation had been performed after birth. Our
low intrapartum stillbirth rate was related to the
use of continuous foetal heart rate monitoring, as
well as short decision-to-delivery interval (median
10 minutes) and bradycardia-to-delivery interval
(median 11 minutes); these approaches have been
described in our previous reports.11 12 13
Changes in stillbirth causes and risk factors
In this study, we observed a significant decline
in stillbirths caused by congenital malformations
and chromosomal abnormalities since 2010. This
coincided with implementation of the universal first
trimester Down syndrome screening by the Hospital
Authority in 2010,14 15 16 as well as the provision of
non-invasive cell-free foetal DNA testing in private
sectors beginning in 2011.17 18 These two new
services might have various implications beyond
improvements in detection of foetuses with trisomy
21. The early detection of lethal malformations
and genetic disorders (eg, trisomy 18, trisomy 13,
and alpha-thalassemia major) was also improved.19
Because mothers were encouraged to undergo
earlier antenatal assessments, foetuses with those
lethal diseases were converted to legal abortions
earlier during pregnancy; instead of progressing
until stillbirth or neonatal death.
Pre-eclampsia is a known important causative
factor of foetal death.20 In this study, pre-eclampsia
was regarded as the leading cause of 24 stillbirths;
eight of these cases (33.3%) also had FGR that
contributed to birthweight below the first centile.
In addition, pre-eclampsia caused placental
abruption in another 11 stillbirths; co-existing pre-eclampsia
was present in one case of congenital
abnormality (Haemoglobin Barts) and one case of
chorioamnionitis. Therefore, the risk of stillbirth
in the presence of pre-eclampsia was increased by
six-fold, from 1.6% to 9.6% (Table 5). Although the
prevalence of pre-eclampsia increased from 1.5%
(888/58 634) in 2000-09 to 1.7% (1090/66 031)
in 2010-19 (Table 6), the pre-eclampsia–related
stillbirth rate decreased from 2.5% (22/888) to 1.4%
(15/1090). This reduction is probably related to
improvements in antenatal care, early detection,
and intervention (eg, iatrogenic preterm delivery).
Because increased pre-eclampsia prevalence is
related to advanced maternal age and obesity,7 21
primary prevention via first trimester screening
and aspirin prophylaxis is essential for preventing
adverse foetal outcomes in the future.22 23 24 25
We have noticed increasing rates of stillbirths
related to placental pathologies, such as villitis or
villous vasculopathy. Stillbirths were also associated
with FGR; approximately 30% of cases involved
birthweight below the third centile. Because
placentas of livebirths were not subjected to routine
histological examination, the prevalences of such pathologies remain unknown. Furthermore, these
cases were categorised only according to post-delivery
histology; the determinations were made
after exclusion of obvious clinical abnormalities
(eg, pre-eclampsia, medical diseases, congenital
disorders, and genetic disorders). Therefore, such
pathologies are challenging to diagnose prenatally
with the goal of preventing foetal death, unless
FGR is detected. Similarly, the 61 cases in the FGR
group involved stillbirths without obvious causes
of FGR. Their birthweight centiles were below first
centile, first to below third centile, and third to less
than fifth centile in 44 (72.1%), 16 (26.2%), and one
(1.6%) cases, respectively. However, a substantial
proportion of these cases (43.5%) were diagnosed
based on post-delivery birthweight alone, rather
than through prenatal assessments. Conventionally,
foetal growth is routinely monitored at intervals
of a few weeks by fundal height measurement in
public sector hospitals. Only high-risk patients
or suspected cases of FGR are monitored via
sonographic foetal biometric measurement. Further
service improvements should focus on increasing the
rate of FGR detection, while minimising the false-positive
rate using a combination of first trimester
biochemical markers.26 27 28 29 30 31
Unexplained stillbirths constituted 36.2% of
our stillbirth cohort, which is consistent with the
prevalences in other developed countries32; the
prevalence in our study did not substantially decrease
during the study period. With the exceptions of
nulliparity and non-admitted status, we were unable
to identify any maternal demographic factors that
contributed to this type of stillbirth. Unexplained
stillbirths were unrelated to extreme maternal
age or extreme maternal BMI (ie, underweight or
overweight). In 17.4% of these cases, the birthweight
centile was between the third and less than tenth
centile, which was much higher than expected.
These might have constituted more subtle cases of
FGR or late-onset FGR. Further studies are needed
to determine whether late-onset FGR or elective
induction of labour at 39 weeks can reduce the
stillbirth rate in Hong Kong. Chorioamnionitis,
placental abruption, and cord accidents are
unpredictable events; their prevalences among
stillbirths remained similar throughout the study
period.
Strengths and limitations
To our knowledge, this is the largest study
concerning the prevalence and causes of stillbirth
in Hong Kong with a 20-year study period. The
computerised database of the Hospital Authority
provided comprehensive information concerning
major risk factors, although it did not contain data
concerning maternal social factors (eg, smoking,
family income, and marital status). Clinical practice might have changed during the 20-year
study period; this might have led to modifications
regarding the classification of stillbirth causes. For
example, the shift from karyotyping to chromosomal
microarrays may facilitate more diagnoses of genetic
diseases.33 Foetal growth restriction was classified
based on birthweight centile; it might have been
underestimated because foetal death might have
occurred several days before birth. Thus, we used
foetal weight below the third centile as a threshold to
identify high-risk cases. Lastly, although our cohort
provides extensive data regarding stillbirths in Hong
Kong, the number of cases may have been insufficient
to identify statistically significant results concerning
less common events. Nonetheless, our findings
provide a basis for future territory-wide reviews
of perinatal outcomes. We will also investigate the
neonatal mortality of singleton pregnancies and
perinatal mortality of multiple pregnancies in our
subsequent studies.
Conclusion
The overall perinatal mortality rate was significantly
reduced from 2000-09 to 2010-19. We observed a
declining trend in stillbirth rate among singleton
pregnancies, mainly because of improvements in
early prenatal diagnosis of congenital malformations
and genetic disorders; this led to increasing
termination of affected pregnancies before 24 weeks.
The prevalence of pre-eclampsia has been rising
because of the increasing maternal age, but the
stillbirth rate among patients with pre-eclampsia
has decreased. Foetal growth restriction of
unknown cause contributes to 16% of all stillbirths;
its prevalence has not changed over time. The
majority of FGR cases were not diagnosed before
birth. Overall, 36% of stillbirths were unexplained,
and they might have involved components of FGR.
Therefore, prenatal FGR detection remains a priority
for our obstetric service.
Author contributions
Concept or design: STK Wong, WT Tse, TY Leung.
Acquisition of data: STK Wong, WT Tse, TY Leung.
Analysis or interpretation of data: STK Wong, WT Tse, DS Sahota.
Drafting of the manuscript: STK Wong, SL Lau, TY Leung.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: STK Wong, WT Tse, TY Leung.
Analysis or interpretation of data: STK Wong, WT Tse, DS Sahota.
Drafting of the manuscript: STK Wong, SL Lau, TY Leung.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Ethical approval was obtained from The Joint Chinese University of Hong Kong–New Territories East Cluster
Clinical Research Ethics Committee (Ref CRE 2017.442).
References
1. Hong Kong College of Obstetricians & Gynaecologists.
Territory-wide Audit Report 2014. Available from: https://www.hkcog.org.hk/hkcog/Download/Territory-wide_Audit_in_Obstetrics_Gynaecology_2014.pdf. Accessed 11 Feb 2021.
2. Cousens S, Blencowe H, Stanton C, et al. National, regional, and worldwide estimates of stillbirth rates in
2009 with trends since 1995: a systematic analysis. Lancet
2011;377:1319-30. Crossref
3. World Health Organization. Maternal, newborn, child
and adolescent health. Definition of stillbirths. Available
from: https://www.who.int/maternal_child_adolescent/epidemiology/stillbirth/en/ Accessed 11 Feb 2021.
4. Blencowe H, Cousens S, Jassir FB, et al. National, regional,
and worldwide estimates of stillbirth rates in 2015, with
trends from 2000: a systematic analysis. Lancet Glob
Health 2016;4:e98-108.Crossref
5. Lawn JE, Blencowe H, Pattinson R, et al. Stillbirths: Where? When? Why? How to make the data count? Lancet
2011;377:1448-63. Crossref
6. de Bernis L, Kinney MV, Stones W, et al. Stillbirths: ending preventable deaths by 2030. Lancet 2016;387:703-16. Crossref
7. Leung TY, Leung TN, Sahota DS, et al. Trends in maternal obesity and associated risks of adverse pregnancy outcomes in a population of Chinese women. BJOG 2008;115:1529-
37. Crossref
8. Chan SS, Lau AP, To KF, Leung TY, Lau TK, Leung TN. Umbilical cord ulceration as a cause of fetal haemorrhage
and stillbirth. Hong Kong Med J 2008;14:148-51.
9. Lau TK, Li CY. A perinatal audit of stillbirths in a teaching
hospital in Hong Kong. Aust N Z J Obstet Gynaecol
1994;34:416-21. Crossref
10. Goldenberg RL, McClure EM, Bann CM. The relationship
of intrapartum and antepartum stillbirth rates to measures
of obstetric care in developed and developing countries.
Acta Obstet Gynecol Scand 2007;86:1303-9. Crossref
11. Leung TY, Chung PW, Rogers MS, Sahota DS, Lao TT,
Chung TK. Urgent Cesarean delivery for fetal bradycardia.
Obstet Gynecol 2009;114:1023-8. Crossref
12. Leung TY, Lao TT. Timing of Caesarean section according to urgency. Best Pract Res Clin Obstet Gynaecol
2013;27:251-67. Crossref
13. Wong L, Tse WT, Lai CY, et al. Bradycardia-to-delivery
interval and fetal outcomes in umbilical cord prolapse.
Acta Obstet Gynecol Scand 2021;100:170-7. Crossref
14. Sahota DS, Leung WC, Chan WP, To WW, Lau ET,
Leung TY. Prospective assessment of the Hong Kong
Hospital Authority universal Down syndrome screening
programme. Hong Kong Med J 2013;19:101-8.
15. Sahota DS, Leung TY, Fung TY, Chan LW, Law LW, Lau TK.
Medians and correction of biochemical and ultrasound
markers in Chinese undergoing first trimester screening
for Trisomy 21. Ultrasound Obstet Gynecol 2009;33:387-93. Crossref
16. Leung TY, Chan LW, Leung TN, et al. First-trimester combined screening for trisomy 21 in a predominantly
Chinese population. Ultrasound Obstet Gynecol
2007;29:14-7. Crossref
17. Cheng Y, Leung WC, Leung TY, et al. Women’s preference
for non-invasive prenatal DNA testing versus chromosomal
microarray after screening for Down syndrome: a
prospective study. BJOG 2018;125:451-9. Crossref
18. Chan YM, Leung WC, Chan WP, Leung TY, Cheng YK, Sahota DS. Women’s uptake of non-invasive DNA testing
following a high-risk screening test for trisomy 21 within
a publicly funded healthcare system: findings from a
retrospective review. Prenat Diagn 2015;35:342-7. Crossref
19. Leung TY, Vogel I, Lau TK, et al. Identification of
submicroscopic chromosomal aberrations in fetuses with
increased nuchal translucency and an apparently normal
karyotype. Ultrasound Obstet Gynecol 2011;38:314-9. Crossref
20. Harmon QE, Huang L, Umbach DM, et al. Risk of fetal death with preeclampsia. Obstet Gynecol 2015;125:628-35. Crossref
21. Chaemsaithong P, Leung TY, Sahota D, et al. Body
mass index at 11-13 weeks’ gestation and pregnancy
complications in a Southern Chinese population: a
retrospective cohort study. J Matern Fetal Neonatal Med
2019;32:2056-68. Crossref
22. Chaemsaithong P, Sahota D, Pooh RK, et al. First-trimester
pre-eclampsia biomarker profiles in Asian population:
a multicenter cohort study. Ultrasound Obstet Gynecol
2020;56:206-14. Crossref
23. Chaemsaithong P, Pooh RK, Zheng M, et al. Prospective
evaluation of screening performance of first-trimester
prediction models for preterm preeclampsia in Asian
population. Am J Obstet Gynecol 2019;221:650.e1-16. Crossref
24. Cheng YK, Poon LC, Shennan A, Leung TY, Sahota DS.
Inter-manufacturer comparison of automated
immunoassays for the measurement of soluble FMS-like
tyrosine kinase-1 and placental growth factor. Pregnancy
Hypertens 2019;17:165-71. Crossref
25. Cheng Y, Leung TY, Law LW, Ting YH, Law KM, Sahota DS.
First trimester screening for pre-eclampsia in Chinese
pregnancies: case-control study. BJOG 2018;125:442-9. Crossref
26. Li W, Chung CY, Wang CC, et al. Monochorionic twins
with selective fetal growth restriction: insight from
placental whole transcriptome analysis. Am J Obstet
Gynecol 2020;223:749.e1-16. Crossref
27. Meng M, Cheng YK, Wu L, et al. Whole genome miRNA
profiling revealed miR-199a as potential placental
pathogenesis of selective fetal growth restriction in
monochorionic twin pregnancies. Placenta 2020;92:44-53. Crossref
28. Cheng YK, Lu J, Leung TY, Chan YM, Sahota DS.
Prospective assessment of the INTERGROWTH-21
and World Health Organization estimated fetal weight
reference curve. Ultrasound Obstet Gynecol 2018;51:792-8. Crossref
29. Cheng Y, Leung TY, Lao T, Chan YM, Sahota DS. Impact
of replacing Chinese ethnicity-specific fetal biometry
charts with the INTERGROWTH-21(st) standard. BJOG
2016;123 Suppl 3:48-55. Crossref
30. Leung TY, Chan LW, Leung TN, Fung TY, Sahota DS,
Lau TK. First trimester maternal serum levels of placental
hormones are independent predictors of second trimester
fetal growth parameters. Ultrasound Obstet Gynecol
2006;27:156-61. Crossref
31. Leung TY, Sahota DS, Chan LW, et al. Prediction of birth
weight by crown-rump length and maternal serum levels
of pregnancy-associated plasma protein-A in the first
trimester. Ultrasound Obstet Gynecol 2008;31:10-4. Crossref
32. Reinebrant HE, Leisher SH, Coory M, et al. Making
stillbirths visible: a systematic review of globally reported
causes of stillbirth. BJOG 2018;125:212-24. Crossref
33. Hui AS, Chau MH, Chan YM, et al. The role of chromosomal
microarray analysis among fetuses with normal karyotype
and single system anomaly or nonspecific sonographic
findings. Acta Obstet Gynecol Scand 2021;100:235-43. Crossref