© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
REMINISCENCE: ARTEFACTS FROM THE HONG KONG MUSEUM OF MEDICAL SCIENCES
Centry 2 Haemodialysis Machine
CP Ho, FHKAM (Medicine), FHKCP
Member, Education and Research Committee, Hong Kong Museum of Medical Sciences Society
Haemodialysis was introduced in Hong Kong in the late 1960s. Haemodialysis requires a dialyser, which
replicates the kidney functions of removing excess
waste and water from the blood, and a haemodialysis
machine. The haemodialysis machine has several key
functions. The main function is to prepare dialysate
by diluting one part dialysate concentrate with 34
parts of treated water. Dialysate concentrate is used
because during dialysis, dialysate is used at 500 mL per
minute; a 5-hour dialysis session would consume 150
L. Storage and transportation of such a large volume
of dialysate would be problematic and expensive. The
haemodialysis machine also delivers the dialysate to
the dialyser and drains the waste dialysate. Finally, the
haemodialysis machine monitors dialysate pressure
in the arterial and venous chambers, conductivity of
the dialysate, presence of air in the bloodstream, and
blood leakage. Thus, from an engineering perspective,
a dialysis machine is more appropriately called a
‘dialysate delivery and monitoring system’.
In the early days, there were two types of
haemodialysis machines: a batch tank machine and
a proportioning pump machine. Batch tank systems
are very simple; the batch tank has a capacity of about
120 L, which the user manually fills with one part of
dialysate concentrate and 34 parts of treated water to
make the dialysate. Although simple, because of the
large space requirements, it is unsuitable for dialysis
centres where there are often multiple machines. It is
more commonly used in home haemodialysis, where
simplicity and low cost are important. Proportioning
pump machines have two pumps; one pump draws
one part of dialysate concentrate and another pump
draws 34 parts of water. In this way, the dialysate is
made continuously online. This saves a lot of space
in a dialysis centre, and the preparation time needed
is markedly reduced because there is no need to wait
for filling up the batch tanks.1
Early haemodialysis machines only prepared
the dialysate. In addition to the haemodialysis
machine, separate pumps were needed for blood, to
deliver the blood from the patient to the dialyser, and
heparin, for continuous heparinisation. Moreover,
the operator had to calculate the fluid removal
rate using the ‘transmembrane pressure’ and the
‘ultrafiltration coefficient’ of the dialyser; however,
this could only give an estimate. One example of this
early type of machine was the Centry One (COBE
Laboratories, Inc., Lakewood [CO], United States), which was used in Princess Margaret Hospital, Hong
Kong, when it opened in 1977.
In the 1980s, the early machines were replaced
with newer models like the Centry 2 machines
(COBE Laboratories, Inc.) [Fig a] and the AK10
models (Gambro Company). The Centry 2 machines
were more widely used. These offered several
upgrades over the older models. They were compact
and robust with the blood pump and heparin
pump built in. They also included an indicator to
show the rate of fluid removal from the dialyser
(‘ultrafiltration meter’) in real time, obviating the
need for the operator to calculate this and increasing
the accuracy (Fig b
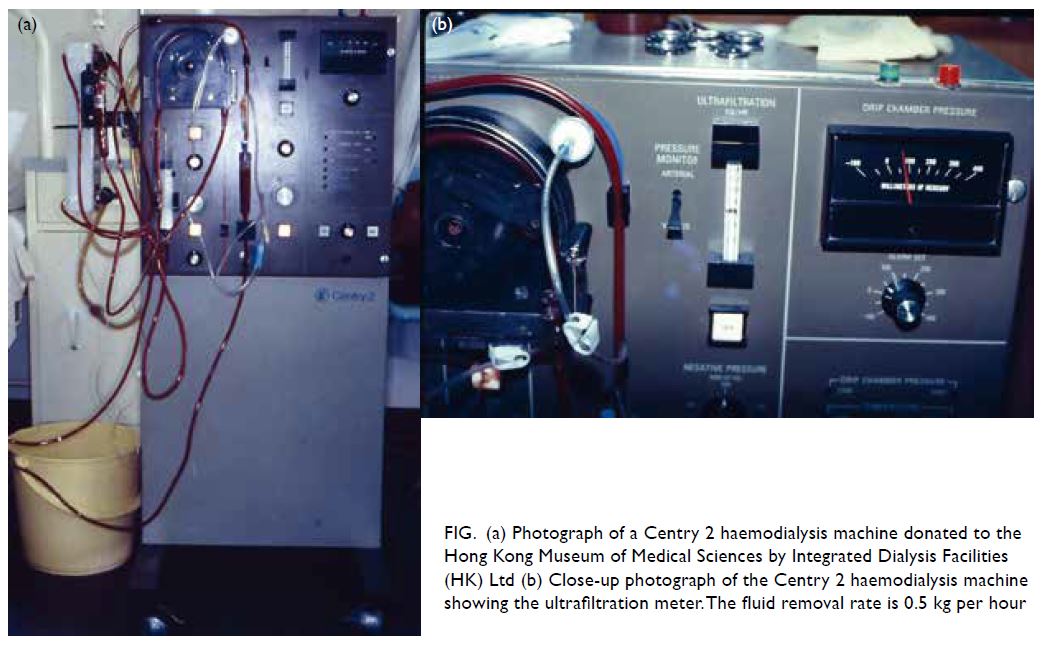
Figure. (a) Photograph of a Centry 2 haemodialysis machine donated to the Hong Kong Museum of Medical Sciences by Integrated Dialysis Facilities (HK) Ltd (b) Close-up photograph of the Centry 2 haemodialysis machine showing the ultrafiltration meter. The fluid removal rate is 0.5 kg per hour
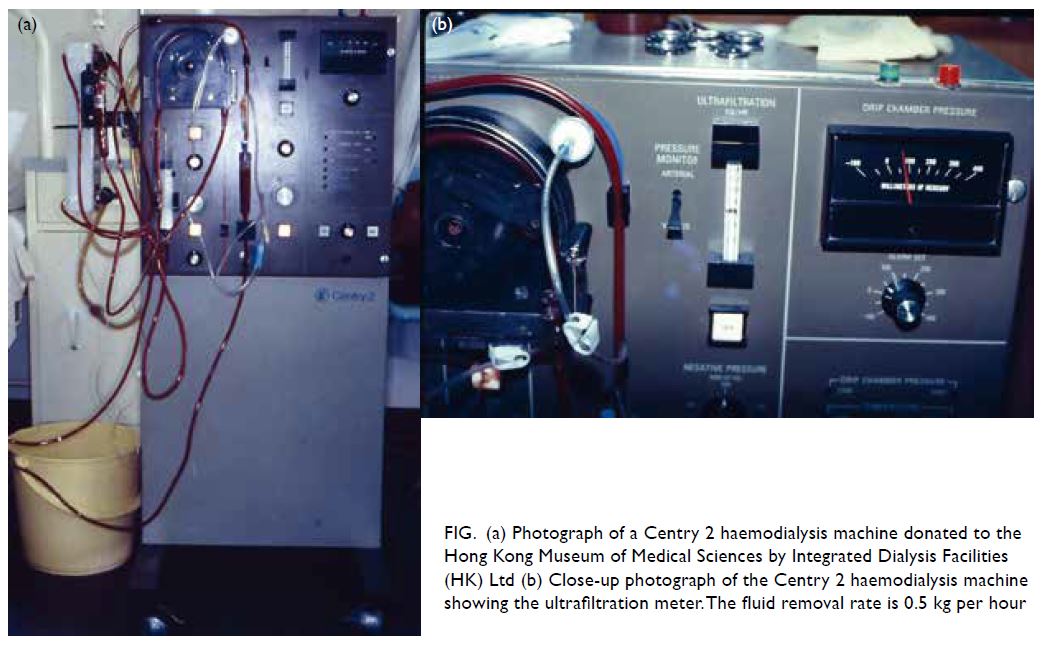
Figure. (a) Photograph of a Centry 2 haemodialysis machine donated to the Hong Kong Museum of Medical Sciences by Integrated Dialysis Facilities (HK) Ltd (b) Close-up photograph of the Centry 2 haemodialysis machine showing the ultrafiltration meter. The fluid removal rate is 0.5 kg per hour
The Centry 2 machine had been widely used in
dialysis centres in Hong Kong as nearly all the public
and private dialysis centres all used it. However, it
was gradually replaced with newer machines in late
1980s. The main drawback of the machine was that the
dialysate contained acetate as the buffer base. During
dialysis, the acetate diffused from the dialysate across
the dialyser membrane into the blood compartment.
The acetate was then converted to bicarbonate in
the liver to replenish the bicarbonate buffer in the
patients’ blood, which was acidic. In elderly patients
or those with multi-system disease, the patient’s liver
might be unable to convert acetate to bicarbonate at a
sufficient rate. As a result, some acetate accumulated
in the blood. Acetate caused vasodilation with
hypotension, headache, and vomiting.
Acetate was used in the dialysate because
of its high solubility. If bicarbonate were used, the
bicarbonate would combine with calcium in the
dialysate and this would cause precipitation and
could blockage of the dialysate path. This problem
was eventually solved by keeping the dialysate (acid)
concentrate solutions and bicarbonate solution
separate. Thus, modern dialysis machines have
three proportioning pumps, one for the bicarbonate
solution, one for the acid concentrate solution, and a
third for the water. The three ingredients are mixed
online and go to the dialyser immediately, avoiding
precipitation.
All new haemodialysis machine models have
bicarbonate dialysis capability. In addition, instead
of only monitoring the ultrafiltration rate, new
machines have the ability to control the rate of
ultrafiltration by directly measuring the volume of
the fluid removed. The operator only has to input the desired ultrafiltration volume, and the machine
automatically monitors the fluid removal and
calculates the negative pressure required, resulting
in accurate fluid removal.
Despite the shortcomings of the Centry 2
machine, it was loved by dialysis staff because it was
compact and reliable. In the early days, relatively
young patients were chosen for haemodialysis who could tolerate the bicarbonate dialysis and
some volume inaccuracies. The Centry 2 because a
workhorse among haemodialysis units. Nevertheless,
with society becoming more affluent and technology
advancing, new machines were introduced for their
‘bicarbonate dialysis’ and ‘ultrafiltration monitor’, older patients could be admitted for haemodialysis
with good clinical results.
1. Ho CP, Au YF, Wong KK. A review of home haemodialysis in Hong Kong. Available from: http://www.dialysis.com.hk/wp-content/uploads/a-review-of-home-haemodialysis-in-HK.pdf. Accessed 20 Jun 2022.

