© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
COMMENTARY
ICU Liberation for critically ill children in
Hong Kong
A Dudi, MB, BS, FAAP1; KL Hon, MB, BS, MD1; Henry CH Pak, MSc, BSc PT2 Stephen WW Chan, DHSc, MSc2; Cecilia YS Leung, MSc, BSc OT2; Sabina CS Chan, MSc, MA2 CC Au, MB, BS, MRCPCH1
1 Paediatrics and Adolescent Medicine, Hong Kong Children’s Hospital, Hong Kong
2 Department of Allied Health, Hong Kong Children’s Hospital, Hong Kong
Corresponding author: Dr CC Au (aucc@ymail.com)
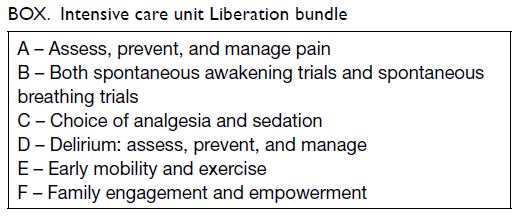
Intensive care unit (ICU) Liberation (https://www.sccm.org/iculiberation) is a campaign to promote
patient recovery by being mindful of reducing
iatrogenic harms during ICU stay, proposed by the
United States Society of Critical Care Medicine.1 2
The ICU Liberation bundle includes the ABCDEF
elements (Box). The ICU Liberation elements have
been broadly adopted in adult intensive care units
and improved outcomes significantly.3 Moreover,
ICU Liberation could be adapted to the needs of
children and their family.4 5 Herein we present our
own experience of adopting and implementing ICU
Liberation practices at a paediatric ICU (PICU) in
Hong Kong.
In the past decade, more patients have survived paediatric intensive care compared with previous
decades.6 This has brought long-term morbidities
among patients discharged from the PICU,
collectively known as post–intensive care syndrome
(PICS) in children.7 8 These long-term morbidities
include functional deficits of physical, cognitive,
emotional, and social health that affect the daily
life, school performance, and social performance
of these patients and their family.9 10 11 The PICS
affects one-third of patients discharged from PICU
and can persist for years.12 The well-intended and
often aggressive treatment in the PICU is, in part,
the origin of PICS in children. The PICU stay is a
physically traumatic and emotionally stressful
experience for children and their family, and these
individuals may develop PICS, such as post-traumatic
stress disorder13 or critical illness myopathy.14 Acute
PICU care prioritise disease control with aggressive
treatment over considerations for sleep, recovery,
and rehabilitation; however, the patient may develop ventilator dependence,15 physical impairment,16 or delirium.17 18
The PICU at Hong Kong Children’s Hospital
commenced service on 27 March 2019. In the first
2 years, the capacity of the PICU grew rapidly from
four beds to 16 beds, with a total of 650 patients
treated. The PICU provides a full range of intensive
care support, including mechanical ventilation,
continuous renal replacement therapy, and
extracorporeal life support. As clinical leaders with
a vision to transform PICU culture in our hospital,
we advocate ICU Liberation in our daily practice.
We have established close collaboration between
medical, nursing, and allied health teams. The PICU
practice has evolved according to consensus and
teamwork.
Our practice is founded on a humanistic
approach. Learning, caring, and smiling are the
core values of the Hong Kong Children’s Hospital.
Education is emphasised to consolidate knowledge
and changes. Individual patient care goals are
regularly discussed by staff during team rounds.
Staff also receive formal on-the-job training as well
as informal feedback, including on pain assessment,
non-pharmacological treatment, and analgesics;
spontaneous awakening and breathing trial in
children; sedation titration to target adequate effect;
environmental modification to promote sleep and
reduce delirium; early mobilisation; and family
empowerment. A clinical information system is
used to document and review individual patient
progress in the ABCDEF elements. Patient outcomes
are audited and long-term follow-up is arranged
for patients with complicated PICU course. For
patients with acute medical conditions, after their
condition is stabilised, they are considered for each
of the ABCDEF elements. We carefully consider
how to proceed, taking necessary precautions and
correcting deviations, to ensure patient safety at
all times. Patient-related factors, such as functional
status, development, and nutrition, are considered
individually. As a result, interventions in our PICU
have progressed towards improving physical,
psychological, and social sequelae.
Through implementing ICU Liberation practices, we have realised several key improvements.
We have been able to actively mobilise patients who
are still receiving mechanical ventilation, continuous
renal replacement therapy, or intracranial pressure
monitoring. We have actively engaged families, even
during the coronavirus disease 2019 pandemic,
by using communication tools such as digital
photographs and videoconferencing software. We
have facilitated family care even in complex medical
conditions by training caregivers. And we have also
extended family support to palliative care in the
PICU, including home visits. In each case, the ICU
Liberation bundle was carefully considered and
tailored to according to individual assessment.
Barriers to ICU Liberation have been
overcome by leadership and teamwork. Challenges
present were owing to system factors and staff
factors. In our future development we would address
these challenges by developing clinical practice
protocols, coordinating the roles of team members,
and supporting staff knowledge and procedural
competence. We propose focusing in future on
further improvements to treating pain, facilitating
spontaneous breathing, minimising sedation,
preventing delirium, mobilising early, and engaging
family members, in order to better support patient
recovery. Further studies are warranted to evaluate
implementation strategies for ICU Liberation and
perceptions of ICU Liberation in our PICU.
Author contributions
All authors contributed to the concept or design of the study,
acquisition, analysis, and interpretation of the data, drafting
of the manuscript, and critical revision of the manuscript for
important intellectual content. All authors had full access to
the data, contributed to the study, approved the final version
for publication, and take responsibility for its accuracy and
integrity.
Conflicts of interest
As an editor of the journal, KL Hon was not involved in the peer review process. Other authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. Ely EW. The ABCDEF Bundle: science and philosophy of how ICU liberation serves patients and families. Crit Care Med 2017;45:321-30. Crossref
2. Marra A, Ely EW, Pandharipande PP, Patel MB. The ABCDEF bundle in critical care. Crit Care Clin
2017;33:225-43. Crossref
3. Pun BT, Balas MC, Barnes-Daly MA, et al. Caring for critically ill patients with the ABCDEF bundle. Crit Care Med 2019;47:3-14. Crossref
4. Walz A, Canter MO, Betters K. The ICU liberation bundle and strategies for implementation in pediatrics. Curr Pediatr Rep 2020;8:69-78. Crossref
5. Smith HA, Besunder JB, Betters KA, et al. 2022 Society
of critical care medicine clinical practice guidelines
on prevention and management of pain, agitation,
neuromuscular blockade, and delirium in critically
ill pediatric patients with consideration of the ICU
environment and early mobility. Pediatr Crit Care Med
2022;23:e74-110. Crossref
6. Namachivayam P, Shann F, Shekerdemian L, et al. Three
decades of pediatric intensive care: who was admitted,
what happened in intensive care, and what happened
afterward. Pediatr Crit Care Med 2010;11:549-55. Crossref
7. Manning JC, Pinto NP, Rennick JE, Colville G, Curley MA.
Conceptualizing post intensive care syndrome in
children—The PICS-p Framework. Pediatr Crit Care Med
2018;19:298-300. Crossref
8. Herrup EA, Wieczorek B, Kudchadkar SR. Characteristics of postintensive care syndrome in survivors of pediatric critical illness: a systematic review. World J Crit Care Med
2017;6:124-34. Crossref
9. Ebrahim S, Singh S, Hutchison JS, et al. Adaptive behavior, functional outcomes, and quality of life outcomes of children requiring urgent ICU admission. Pediatr Crit
Care Med 2013;14:10-8. Crossref
10. Bronner MB, Knoester H, Sol JJ, Bos AP, Heymans HS, Grootenhuis MA. An explorative study on quality of life and psychological and cognitive function in pediatric survivors
of septic shock. Pediatr Crit Care Med 2009;10:636-42. Crossref
11. Jones S, Rantell K, Stevens K, et al. Outcome at 6 months after admission for pediatric intensive care: a report of a national study of pediatric intensive care units in the United Kingdom. Pediatrics 2006;118:2101-8. Crossref
12. Ong C, Lee JH, Leow MK, Puthucheary ZA. Functional outcomes and physical impairments in pediatric critical care survivors: a scoping review. Pediatr Crit Care Med 2016;17:e247-59. Crossref
13. Nelson LP, Gold JI. Posttraumatic stress disorder in
children and their parents following admission to the
pediatric intensive care unit: a review. Pediatr Crit Care
Med 2012;13:338-47. Crossref
14. Kukreti V, Shamim M, Khilnani P. Intensive care unit acquired weakness in children: critical illness
polyneuropathy and myopathy. Indian J Crit Care Med
2014;18:95-101. Crossref
15. Shehabi Y, Bellomo R, Reade MC, et al. Early intensive care sedation predicts long-term mortality in ventilated critically ill patients. Am J Respir Crit Care Med
2012;186:724-31. Crossref
16. Bone MF, Feinglass JM, Goodman DM. Risk factors for acquiring functional and cognitive disabilities during admission to a PICU. Pediatr Crit Care Med 2014;15:640-8. Crossref
17. Smith HA, Gangopadhyay M, Goben CM, et al. Delirium
and benzodiazepines associated with prolonged ICU stay
in critically ill infants and young children. Crit Care Med
2017;45:1427-35. Crossref
18. Smith HA, Fuchs DC, Pandharipande PP, Barr FE, Ely EW.
Delirium: an emerging frontier in the management of
critically ill children. Crit Care Clin 2009;25:593-614. Crossref