Hong Kong Med J 2022 Jun;28(3):270.e1–3
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Unusual gallbladder disease: spontaneous
gallbladder haematoma
Se-kook Kee, MD1; Dongwook Je, MD2; Woo-young Nho, MD1,2
1 Department of Surgery, CHA University, Republic of Korea
2 Department of Emergency Medicine, CHA University, Republic of Korea
Corresponding author: Prof WY Nho (wooyoung.nho@gmail.com)
In September 2020, a 29-year-old woman presented
to the emergency department with a 2-day history
of upper abdominal pain. The patient had no history
of recent trauma around the abdominal area. The
patient’s vital signs were stable upon arrival but
physical examination revealed tenderness over the
right upper quadrant area. The patient reported
moderate to heavy alcohol consumption (10-15
standard drinks per week). Laboratory findings
revealed a white blood cell count of 3030/mm3,
haemoglobin level 12.8 g/dL, and low platelet count of 34 000/mm3. The prothrombin time was mildly
prolonged to 14.2 s. Elevated levels of liver enzymes,
aspartate transaminase (113 U/L), direct bilirubin
(6.18 mg/dL), and gamma-glutamyltransferase
(350 U/L), were reported. Computed tomography
(CT) scans showed a distended gallbladder with
several gallstones and bile duct stones. Moreover,
the intraluminal space of the gallbladder was filled
with heterogeneous material, and extravasation of
the contrast agent was suspected in the arterial phase
(Fig 1). Emergency laparoscopic exploration was planned with a preoperative diagnosis of gallbladder
haematoma. At the first laparoscope view, cirrhotic
change to the liver with ascites and an oedematous
gallbladder were evident (Fig 2a). The surgeon tried
gallbladder decompression by needle aspiration and
made a small opening to remove the blood but it was
unsuccessful (Fig 2b). Laparoscopic cholecystectomy
was successful without complications such as
perforation (Fig 2c and d). Endoscopic retrograde
cholangiopancreatography with endoscopic
sphincterotomy was performed 5 days after the
initial surgery and remnant common bile duct stones
were removed. Pathological evaluation revealed
a gallbladder haematoma with 30 to 40 gallstones
(Fig 3). Moreover, venous vessels were remarkably
dilated in the vicinity of the haemorrhagic site on
CD31 immunostaining. The patient was discharged
on postoperative day 10 with no complications.
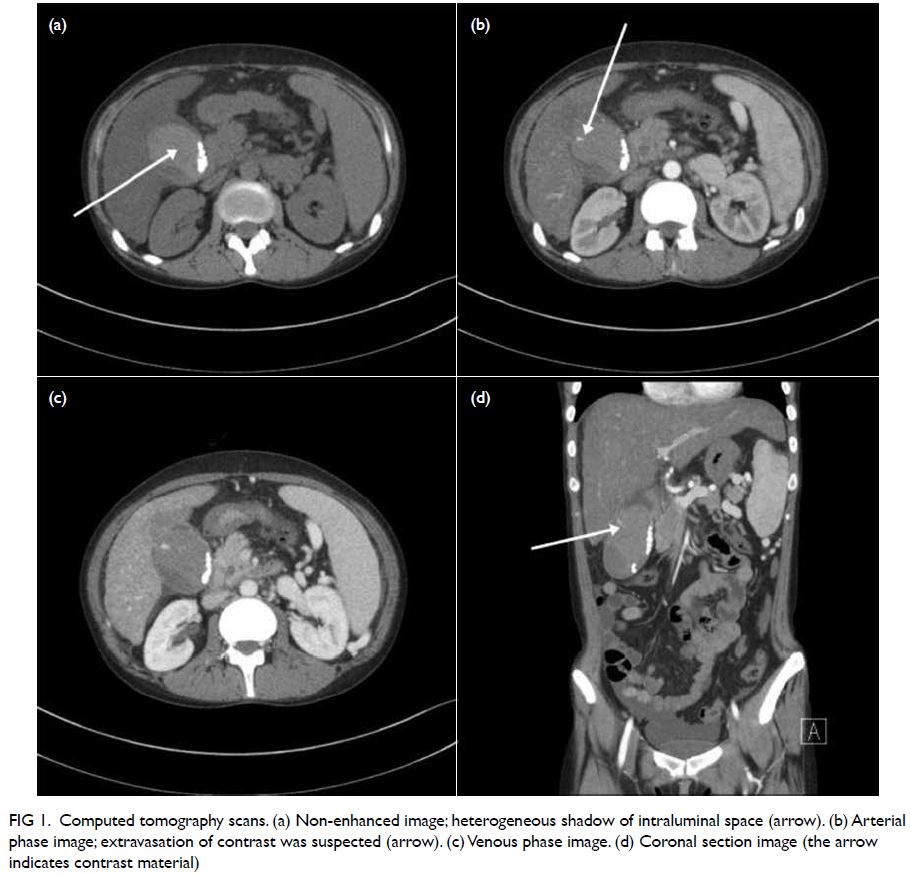
Figure 1. Computed tomography scans. (a) Non-enhanced image; heterogeneous shadow of intraluminal space (arrow). (b) Arterial phase image; extravasation of contrast was suspected (arrow). (c) Venous phase image. (d) Coronal section image (the arrow indicates contrast material)
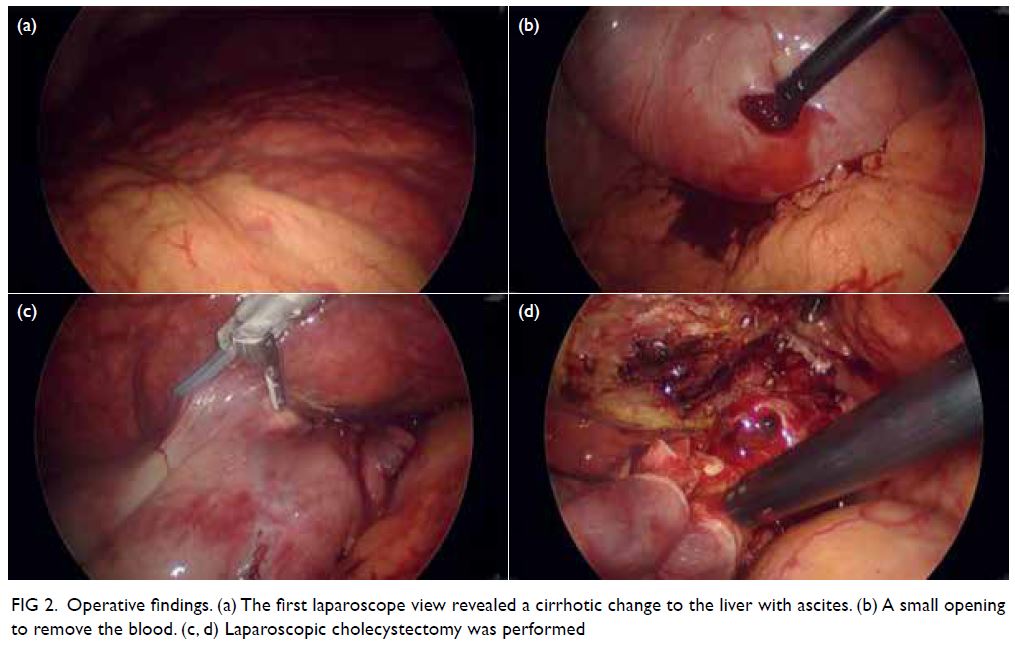
Figure 2. Operative findings. (a) The first laparoscope view revealed a cirrhotic change to the liver with ascites. (b) A small opening to remove the blood. (c, d) Laparoscopic cholecystectomy was performed
The gallbladder is normally physiologically
empty or filled with bile juice. Gallbladder haematoma
is defined as filling of the gallbladder with blood. The
definition can vary from gallbladder bleeding that
comprises active bleeding inside the gallbladder to
gallbladder haematoma when already-formed blood
clots are evident. Haemorrhagic cholecystitis may be
an appropriate term in cases of a gallbladder showing
inflammation with blood. Reported risk factors for
spontaneous bleeding include atherosclerosis or
aneurysm, biliary malignancy, renal failure, cirrhosis,
and coagulopathy, or anticoagulant medication.1 2 3
Moreover, abdominal blunt trauma can lead to gallbladder injury and cause gallbladder bleeding.3
Clinical manifestations of gallbladder haematoma
similarly represent acute gallbladder disease.2 Upper
abdominal pain is frequent due to distension of the
gallbladder, and melena or haematemesis may also be
present. In cases of cholecystitis, fever may develop,
and laboratory study will demonstrate inflammation.
The conventional radiological methods to evaluate
gallbladder disease like ultrasonography or CT scan
have diagnostic value.3 Ultrasonography may reveal
a blood clot in the lumen with wall thickening and
fluid accumulation around the gallbladder.2 In the
CT scan, hyperdense blood and bile shadow with or without fluid level may be suspicious of gallbladder
haematoma. Extravasation of contrast material into
the lumen of the gallbladder during the arterial
phase of contrast-enhanced CT is related to active
bleeding.3,4 Surgical treatment produces superior
results and the minimally invasive method of a
laparoscopic approach has been widely adopted.1 3
Other endoscopic or percutaneous approaches for
decompression may be considered before surgery.1
Gallbladder haematoma is associated with high
morbidity and mortality. Delayed management
potentially increases the risk of perforation and
concomitant unfavourable outcomes.4 5
Author contributions
Concept or design: WY Nho.
Acquisition of data: D Je.
Analysis or interpretation of data: SK Kee.
Drafting of the manuscript: SK Kee.
Critical revision of the manuscript for important intellectual content: WY Nho.
Acquisition of data: D Je.
Analysis or interpretation of data: SK Kee.
Drafting of the manuscript: SK Kee.
Critical revision of the manuscript for important intellectual content: WY Nho.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The study was reviewed and approved by the Institutional Review Board (IRB) of CHA Gumi Medical Center (GM20-11).
1. Leaning M. Surgical case report—acalculous hemorrhagic cholecystitis. J Surg Case Rep 2021;2021:rjab075. Crossref
2. Itagaki H, Katuhiko S. Gallbladder hemorrhage during orally administered edoxaban therapy: a case report. J Med Case Rep 2019;13:383. Crossref
3. Parekh J, Corvera CU. Hemorrhagic cholecystitis. Arch Surg 2010;145:202-4. Crossref
4. Kwon JN. Hemorrhagic cholecystitis: report of a case. Korean J Hepatobiliary Pancreat Surg 2012;16:120-2. Crossref
5. López V, Alconchel F. Hemorrhagic cholecystitis. Radiology 2018;289:316. Crossref


