Hong Kong Med J 2022 Jun;28(3):239–48 | Epub 20 Jun 2022
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE (HEALTHCARE IN MAINLAND CHINA)
Unnecessary caesarean section delivery in rural China: exploration of relationships with full-term
gestational age and early childhood development
A Yue, PhD1; W Zheng, MD1; S Li, PhD1,2; Q Jiang, MD1; Y Li, PhD1; Y Shi, PhD1
1 Center for Experimental Economics in Education, Shaanxi Normal University, PR China
2 National School of Development, Beijing University, Beijing, PR China
Corresponding author: Dr S Li (lishanceee@163.com)
Abstract
Introduction: Gestational age at delivery is
reportedly associated with cognitive and non-cognitive
development in early childhood. Delivery
at an earlier full-term gestational age has been
associated with an increased rate of caesarean section
(C-section) delivery; the high rate of C-section
delivery in China implies that the rate of medically
unnecessary C-section delivery is also high. This
study investigated the relationships of medically
unnecessary C-section delivery with full-term
gestational age and early childhood development in
rural China.
Methods: We conducted a survey of 2765 children
(aged 5-24 months) who resided in 22 national
designated poverty counties. Primary caregivers
were interviewed to collect information regarding
child and household characteristics (including the
child’s gestational age), each child’s delivery method,
and reasons for C-section delivery (if applicable).
The children were assessed using the Bayley Scales
of Infant Development. Developmental outcomes
were compared among gestational age-groups;
regression analyses were used to assess relationships
among medically unnecessary C-section delivery,
gestational age, and developmental outcomes.
Results: Overall, 56.2% of children were born at
≤39 weeks of gestation. Among C-section deliveries,
13.1% were medically necessary and >40% could
clearly be classified as medically unnecessary. Repeat C-section was the most common reason
given for medically unnecessary C-section delivery.
For each 1-week increase in full-term gestational
age, cognition scale scores increased by 0.62 points
(P<0.01), language scale scores increased by 0.84
points (P<0.01), and motor scale scores increased
by 0.55 points (P<0.05). Medically unnecessary C-section
delivery was significantly associated with
lower full-term gestational age.
Conclusion: Higher full-term gestational age was
significantly associated with better childhood
developmental outcomes, indicating that medically
unnecessary C-section delivery may negatively
influence early childhood development.
New knowledge added by this study
- Among children born at full term, levels of cognitive, language, and motor development increased with increasing gestational age.
- Caesarean section delivery was negatively associated with gestational age, and a considerable proportion of deliveries in rural China involved medically unnecessary caesarean section.
- There is a need to reduce the rate of medically unnecessary caesarean section delivery, especially when this delivery method is chosen based on a desire for repeat caesarean section.
- Physicians should carefully consider the potential consequences when they recommend or agree to perform caesarean section delivery; they should also provide detailed information that helps pregnant women to gain greater knowledge about childbirth.
Introduction
Premature birth can influence cognitive development
and academic achievement in childhood.1 2 The final 4 to 5 weeks of gestation, from 37 to 41 weeks, is
an important period; children born earlier than this
might have risks of worse outcomes later in life.3 4 Substantial brain development occurs during the
37th and 38th weeks of gestation5 6; consistent with
this developmental timing, higher gestational age has
been positively associated with cognitive and motor
development in early childhood.7 8 9 Additionally,
higher full-term gestational age has been positively
associated with reading and math achievement in
third grade.10 There is evidence to support the use
of 39 weeks of gestation as a threshold for full-term
delivery.11 12 Moreover, the American College of
Obstetricians and Gynecologists (ACOG) and the
Society for Maternal-Fetal Medicine discourage
medically unnecessary delivery before 39 weeks of
gestation.13
Caesarean section (C-section) is the most
common medical intervention associated with
delivery at a lower gestational ages.14 Furthermore,
an increased rate of delivery at lower gestational age
has been linked to an increased rate of C-section
delivery.15 16 One study found that the rate of elective
C-section delivery gradually increased with a change
in distribution from 39 weeks to 38 weeks.17 To our
knowledge, no studies have explored the relationship
between unnecessary C-section delivery and full-term
gestational age. Caesarean section delivery
is overused in many countries, often without a
clear medical need, because of its convenience
and perceived ease.18 A women’s preference can be
affected by the belief that C-section delivery is safer
for the baby19; it can also be affected by an intense fear of childbirth (eg, with nightmares, physical
complaints, and anxiety).20 Some women might
deliver by C-section for a specific (or auspicious)
birth date or the convenience of returning to full-time
employment.21 22
Although the ACOG encourages measures to
avoid medically unnecessary C-section delivery,13
the global rate of unnecessary C-section delivery
remains high.18 In China, the rate of C-section
delivery is among the highest worldwide (42%-46%)23 24; this high rate persists even in rural areas
with few resources.25 In the early 2000s, the World
Health Organization (WHO) recommended a
rate of C-section delivery below 15% in most
populations26; a more recent study suggested that
a rate of 19% is appropriate.27 For either threshold,
the rate of C-section delivery in China greatly
exceeds international recommendations. According
to a 2010 WHO report, the high rate of C-section
delivery in China implied that the rate of medically
unnecessary C-section delivery was also high.18
While some studies have measured the rate of
C-section delivery in China,28 29 30 there is no published
literature regarding the rate of medically unnecessary
C-section delivery in China or other countries.
Considering the potentially high rate of
medically unnecessary C-section delivery in China,
there is a need to consider its potential associations
with full-term gestational age and early childhood
development. Thus, this study investigated the
relationships of medically unnecessary C-section
delivery with full-term gestational age and early
childhood development in rural China.
Methods
Sample selection
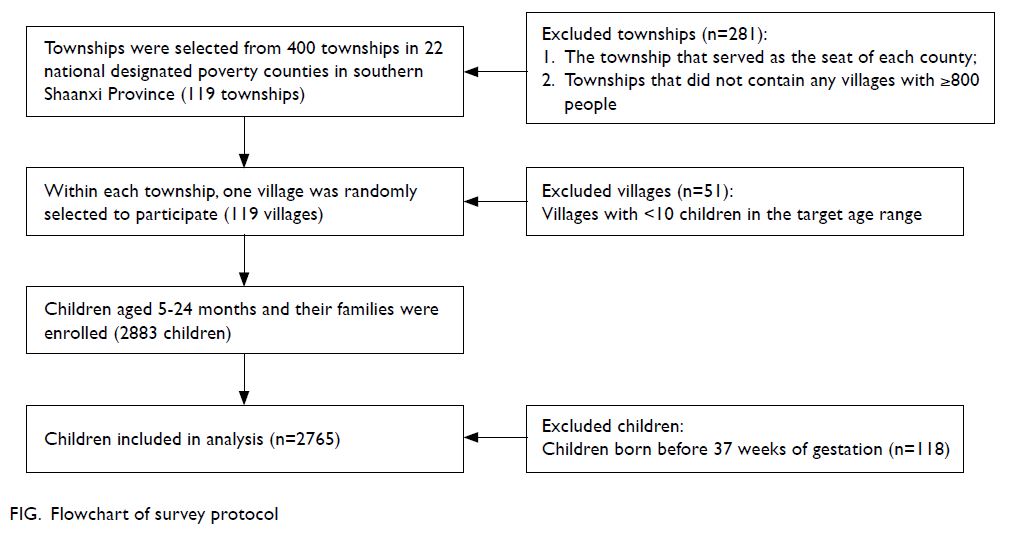
This study used data that were collected from November 2015 to May 2017 in 22 nationally
designated poverty counties located in southern
Shaanxi Province, China. In each county, all
townships (the administrative level between county
and village) were included in the study (Fig), with
the following exceptions: the township that served
as the seat of each county and townships that did not
contain any villages with ≥800 people.
Subsequently, the sample villages and families
were selected as follows. To meet the power
requirements of a larger, interventional study,31
a minimum of 10 children was required in each
village. Therefore, one village (with ≥10 children in
our target age range) was randomly selected from
each township. A list of all registered births in the
previous 24 months was obtained from the local
family planning official in each village. All children
in our target age range (5-24 months) were enrolled.
Because the present study focused on children born
at full term (37-41 weeks of gestation), all children born before 37 weeks of gestation were removed from
the final sample. Regarding variables that did not
change with time, data collected in the second part
of the survey (described below) were used to impute
missing values where possible. Missing values that
could not be imputed were excluded from analysis,
as were missing values that changed over time. We
calculated the mean values of some variables based
on the records of missing data. Multiple imputation
was conducted to determine whether missing values
would influence the results of analysis.
Data collection
In the first part of the survey, teams of trained
enumerators collected socio-economic information
from all participating households. Each child’s
primary caregiver (typically the mother or
grandmother) was administered a detailed survey
regarding child and household characteristics,
including each child’s sex and birth order, the
mother’s age and level of education, the father’s level
of education, and whether the family was receiving
government welfare payments (ie, financial support
for the lowest-income families nationwide). The
family asset index of each household was calculated
using principal component analysis32 based on
whether the household owned or had access to the
following assets: tap water, flushing toilet, water
heater, refrigerator, washing machine, computer,
internet, and transportation (motorcycle, car, or
truck); the approximate value of the home was also
used in the calculation. Each child’s age, gestational
age (determined by the hospital), and birth weight
were obtained from their birth certificate.
In the second part of the survey, each child was administered the third edition of the Bayley
Scales of Infant Development (BSID-III). The BSID-III
is an internationally recognised assessment for
developmental outcomes during early childhood.33
The BSID-III has high inter- and intra-rater
reliability agreement, internal consistency, and test-retest
stability, even when tested in other cultural
contexts.33 34 The BSID-III results are categorised
into five standardised scales, three of which were
used in this study: cognitive (information processing,
counting, and number skills), language (receptive and
expressive communication skills), and motor (fine
and gross motor skills). Each of these scales evaluates
a child’s performance on a series of interactive
tasks, with consideration of the child’s gestational
and chronological ages. Raw scores for each scale
were converted to composite scores in accordance
with BSID-III guidelines.35 These composite scores
allowed comparison of developmental levels among
children who were born at different gestational ages.
The third and final part of the survey collected
information regarding the method of childbirth and
the reasons for C-section delivery (if applicable).
In accordance with the methodology of previous
childbirth surveys,25 36 we asked whether the delivery
had been normal vaginal birth, C-section, or other. For
children delivered by C-section, we asked caregivers
the open-ended question: “Why did the mother have
a C-section?” and recorded all responses. We then
collaborated with a paediatrician who was not a co-author
of the present study to categorise the reasons
as “medically necessary” or “medically unnecessary.” Based on a review of international medical and public health literature, we classified a C-section
delivery as “medically unnecessary” if less risky
alternatives were available (online supplementary Table 1). The final classifications were carefully
reviewed by the paediatrician and adjustments were
made as necessary.
Statistical analyses
All statistical analyses were conducted using Stata
Statistical Software (Version 14.2; StataCorp, College
Station [TX], United States). P values of <0.05 were
considered significant. Student’s t test was used to
compare childhood developmental outcomes across
gestational age-groups. The relationships between
gestational age and childhood developmental
outcomes were assessed using ordinary least squares
regression, with adjustment for the following
potential confounders: child characteristics (sex, age,
and whether the child had siblings) and household
characteristics (whether the mother was the primary
caregiver, maternal age, maternal education, paternal
education, family asset index, and whether the
household received government welfare payments).
Additionally, ordinary least squares regression was used to assess the relationship between
unnecessary C-section delivery and gestational age,
with adjustment for the potential confounders (child
and household characteristics) described above. We
also controlled for BSID-III tester (enumerator) fixed
effects. In all analyses, we account for clustering
within villages using Huber–White cluster-adjusted
standard errors.
Results
Participant socio-economic and demographic
characteristics
The survey protocol is shown in the Figure. In
total, 119 townships were included in the study. We
initially enrolled 2883 children aged 5 to 24 months;
after exclusion of children born before 37 weeks of
gestation, we analysed 2765 children.
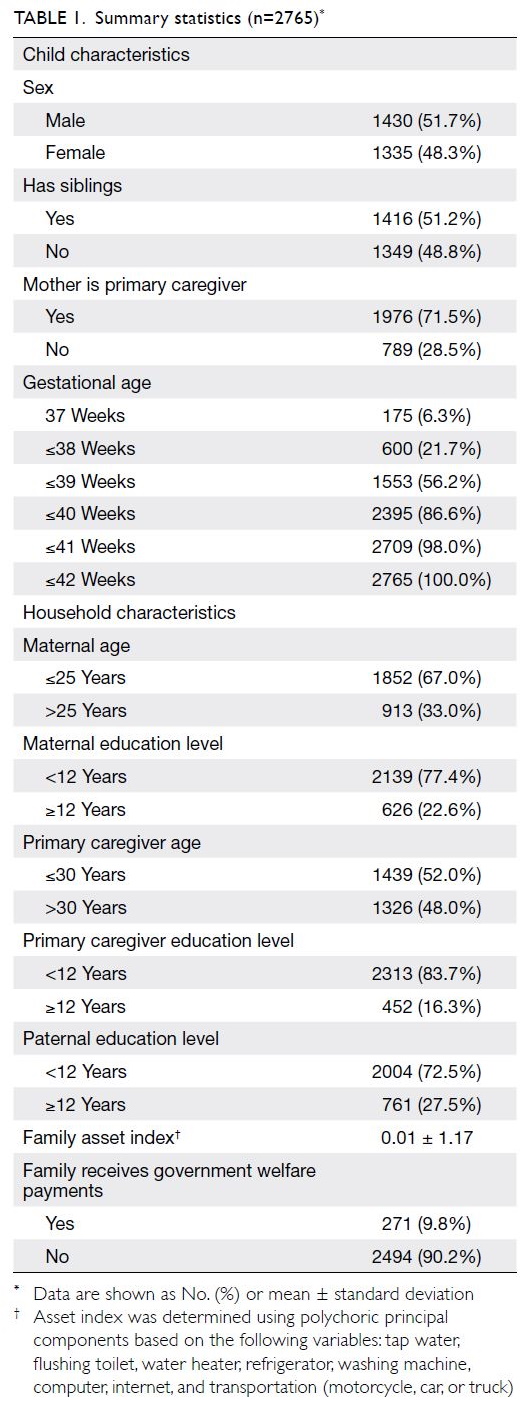
The participants’ socio-economic and
demographic characteristics are shown in Table 1.
More than of the children (51.2%) had siblings at
the time of the survey. The mother was the primary
caregiver for 71.5% of the children. Most mothers
(77.4%) had <12 years of education, and one-third of
mothers (33.0%) were aged >25 years. Less than one-tenth
(9.8%) of sampled families reported receiving
government welfare payments.
Table 1 also shows the gestational ages of the surveyed children. Overall, 6.3% of the children
were delivered at 37 weeks of gestation, 49.8% were
delivered between 38 and 39 weeks, and 41.8% were
delivered between 40 and 41 weeks. Only 2% of the
children were delivered after 41 weeks of gestation.
Links between gestational age and childhood
developmental outcomes
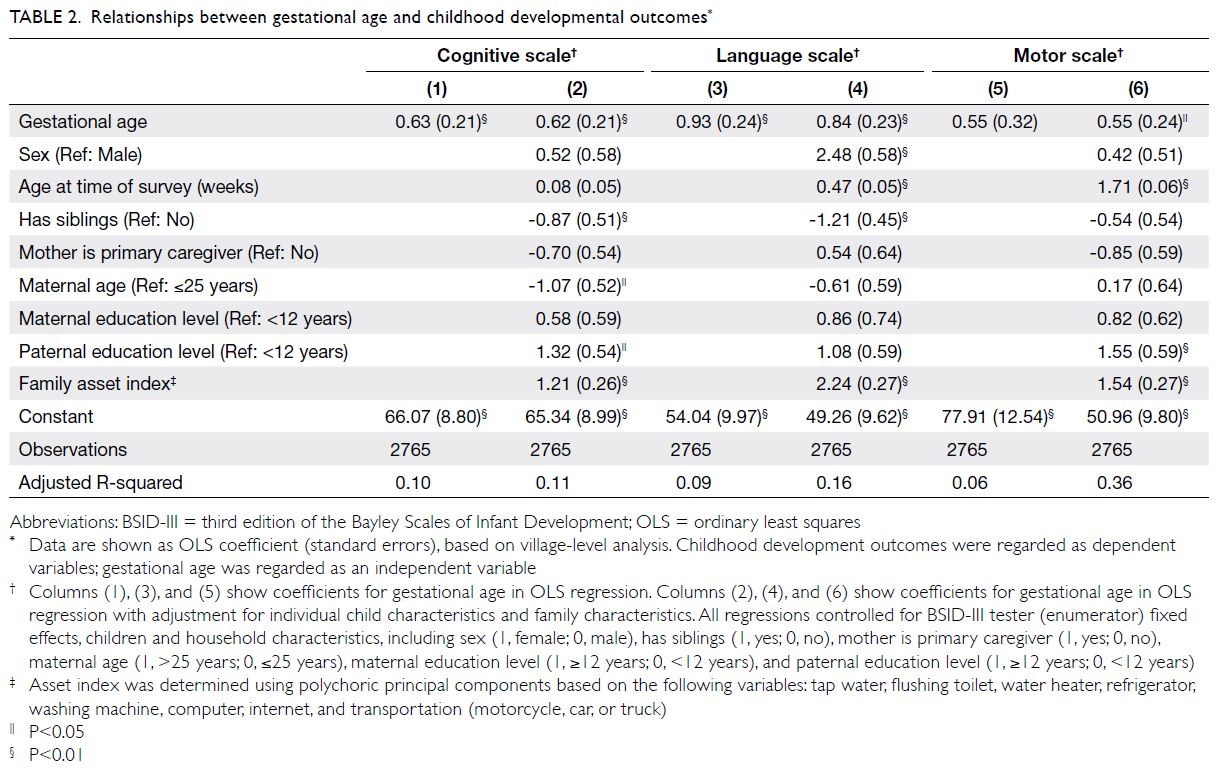
We investigated the relationships between
gestational age and childhood developmental
outcomes (Table 2). Children with higher gestational
ages had higher scores on the cognition, language, and motor scales of the BSID-III. For each 1-week
increase in gestational age, cognition scale scores
increased by 0.62 points (P<0.01), language scale
scores increased by 0.84 points (P<0.01), and motor
scale scores increased by 0.55 points (P<0.05). The
detailed mean cognition, language, and motor scale
scores according to gestational age are shown in the
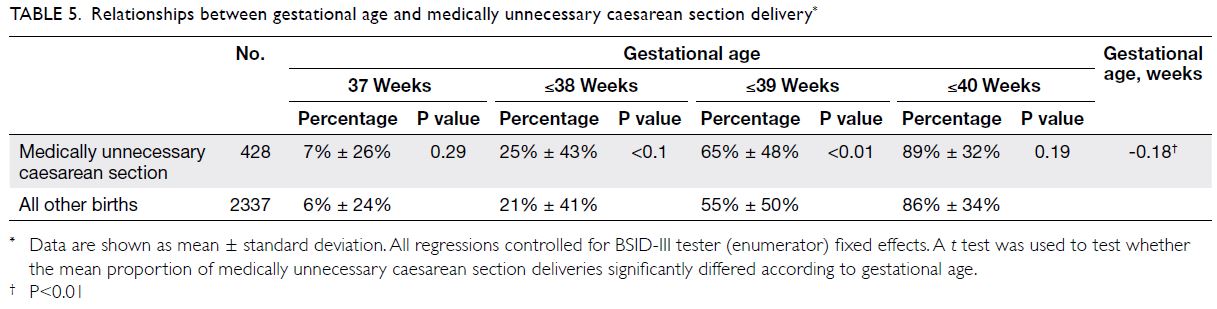
online supplementary Table 2. We also investigated
potential non-linear relationships between
gestational age and developmental scores by adding
a squared term of gestational age to the regression
(Table 3). However, the squared term coefficient
was not statistically significant for cognitive
development. This suggested that gestational age
had non-linear relationships with language and
development, while it had a linear relationship with
cognitive development.
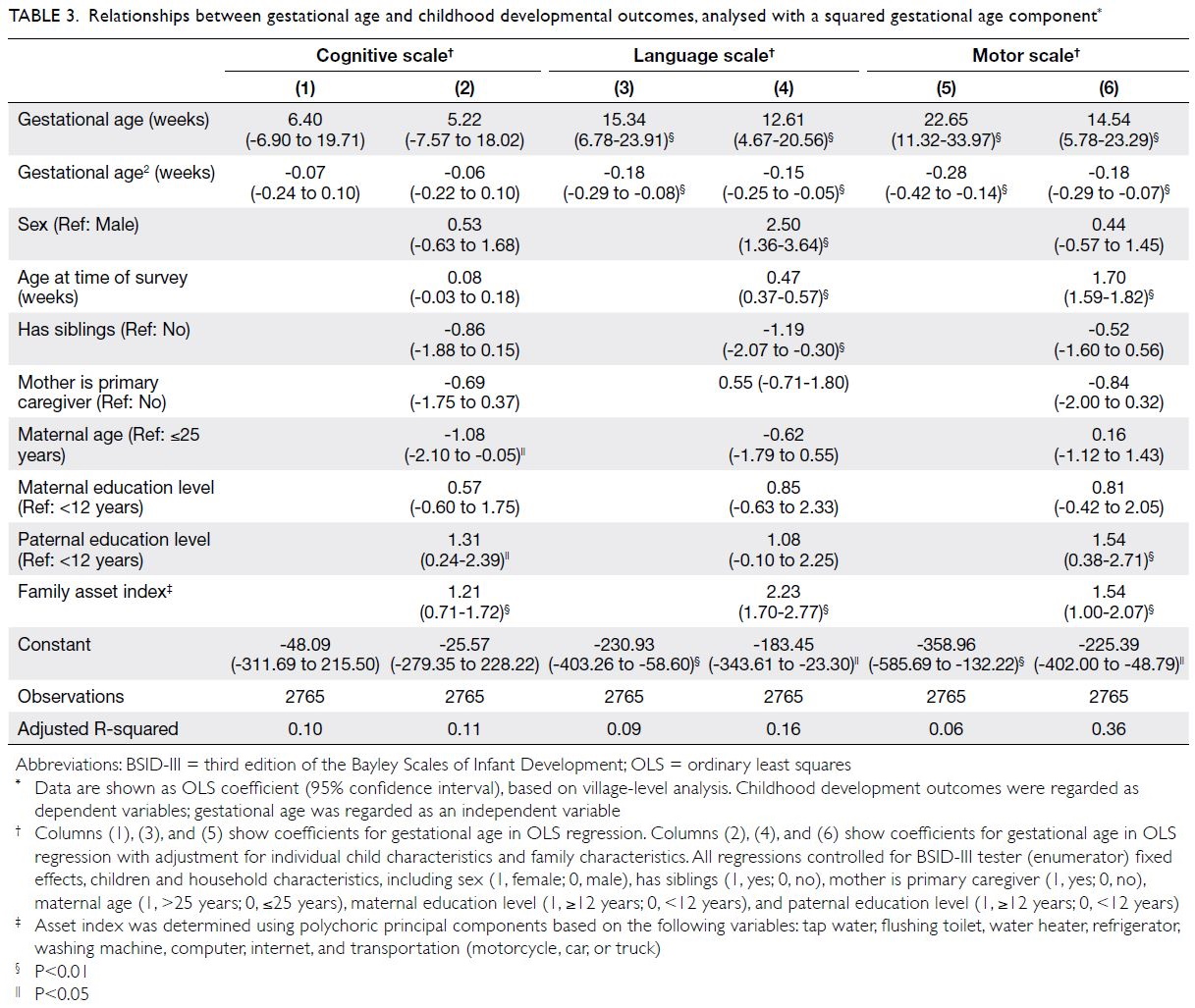
Table 3. Relationships between gestational age and childhood developmental outcomes, analysed with a squared gestational age component
Rate of medically unnecessary caesarean
section delivery and reasons for its selection
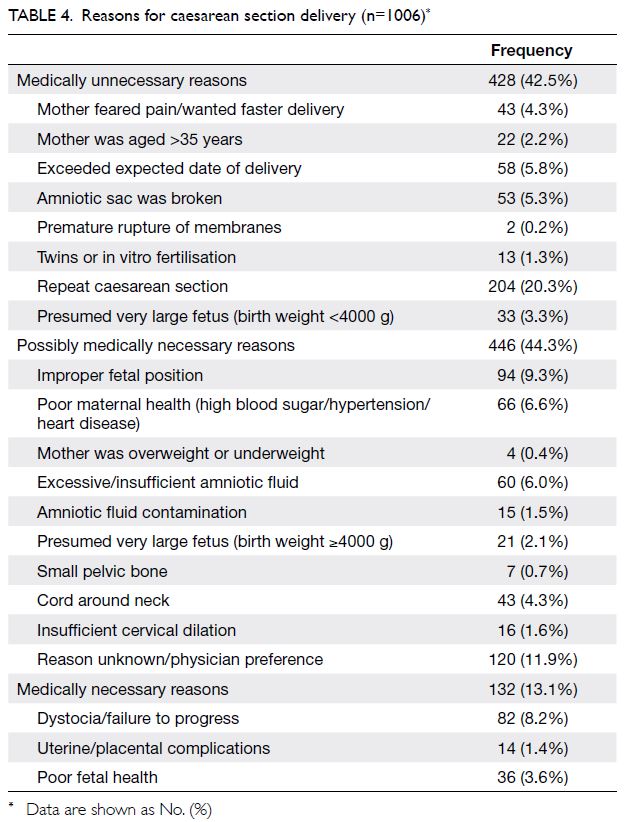
In our sample, more than one-third (36.4%) of the children were delivered by C-section. Of the
medically unnecessary C-section deliveries, 65.2%
were performed at ≤39 weeks of gestation (online supplementary Table 3). Table 4 presents the reasons
given for C-section delivery. Only 13.1% of C-section
deliveries were medically necessary, and >40% of C-section deliveries could clearly be classified
as medically unnecessary. Repeat C-section was
the most common medically unnecessary reason
given for C-section delivery. Additionally, 5.8% of
C-section deliveries were performed because the
expected date of delivery had passed, whereas 5.3%
of C-section deliveries were performed because the
amniotic sac had broken. Finally, 4.3% of C-section
deliveries were performed because the mother
feared pain or desired faster delivery.
Link between unnecessary caesarean section
delivery and gestational age
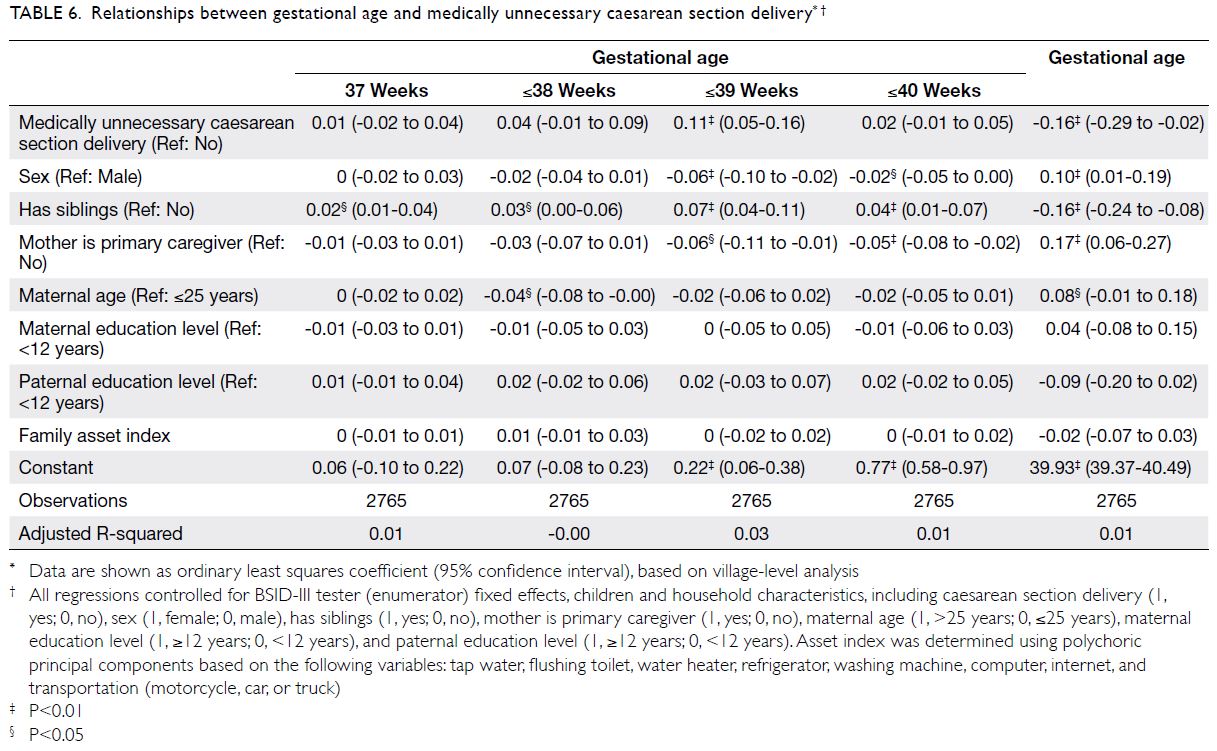
Table 5 shows a series of unadjusted associations
between unnecessary C-section delivery and
gestational ages. Unnecessary C-section delivery
was associated with a significantly greater likelihood
of delivery before 39 weeks of gestation. Delivery at
≤39 weeks of gestation was 65% (P<0.01) more
likely to involve medically unnecessary C-section,
compared with delivery after 39 weeks of gestation.
We also found a significant negative association
between medically unnecessary C-section delivery
and gestational age as a continuous variable.
Specifically, gestational age was 0.18 weeks
lower (P<0.01) in children delivered by medically
unnecessary C-section, compared with children delivered by medically necessary C-section or
possibly medically necessary C-section.
To further explore the relationship between medically unnecessary C-section delivery and
gestational age, we conducted a series of multivariate
regressions with adjustment for child and household
characteristics (Table 6). The results of these analyses
were consistent with the findings of the unadjusted
analyses: medically unnecessary C-section delivery
was significantly associated with lower full-term
gestational age.
Discussion
In this study, we found that higher full-term gestational age was positively associated with better
developmental outcomes among children aged 5 to
24 months in rural China. This finding is consistent with the growing body of international literature
that shows a positive link between gestational age
and developmental outcomes among children born
at full term.7 8 10
However, our data showed a high rate of C-section delivery in rural China, such that 36% of
children were delivered by C-section. This rate is
substantially higher than the 15% rate recommended
by the WHO.26 It is also higher than the rates
in other developing countries, such as Thailand
(34.1%) and India (17.8%).24 Furthermore, nearly half
(42.5%) of the C-section deliveries in our sample
were medically unnecessary. Although the literature
suggests that vaginal delivery after a C-section is safe
and reasonable for most women, many C-section
deliveries in our study were performed because
the mother had a previous C-section. The issue of
repeat C-section delivery is particularly relevant in China since the end of the one-child policy; more
families are choosing to have a second child.37 Our
data suggest that many mothers or their physicians
ignore or are unaware of current guidelines. To
control the high rate of repeat C-section deliveries,
additional efforts are needed to inform women
and physicians that repeat C-section deliveries are
typically unnecessary.
Although painless childbirth methods
including pharmacological (systemic analgesia) and
nonpharmacological methods (hypnosis) have been
developed and widely applied in the past decade,38
4.3% of C-section deliveries in this study were
performed because the mother feared pain. Other
studies have shown that women have an intense fear
of vaginal delivery.39 40 Although this fear contributed
to a small percentage of C-section deliveries in our
study, our finding suggests that women generally
have minimal information about what to expect
during delivery and how to cope with labour pain.
This lack of information may cause women to feel a
lack of control, which can increase their anxiety and
cause some women to develop a catastrophic fear of
labour.41 42 In contrast, communication and support
between pregnant women and their physicians
can greatly improve women’s perceptions and
experiences of childbirth.43 44 Physicians also play a
key role in performing a C-section delivery when it is
medically unnecessary. Physicians may recommend
that women deliver by C-section to avoid the
medical risks (and accompanying litigation) of
vaginal delivery.20 However, we could not explore
this possibility because of data limitations.
In this study, medically unnecessary C-section
delivery was negatively associated with full-term
gestational age. These findings are consistent with
past studies in which gestational age was negatively
associated with the rate of C-section delivery (not
stratified according to medical need).14 45 Importantly,
our study showed that C-section delivery had
reduced full-term gestational age without a clear
medical need. Moreover, the significant association
between full-term gestational age and childhood
development suggested that medically unnecessary C-section delivery could have an impact on early
childhood development.
To our knowledge, this is the first study
to examine the relationship between medically
unnecessary C-section delivery and full-term
gestational age. This is also the first study to
link medically unnecessary C-section delivery
and gestational age to childhood developmental outcomes. Our findings highlight the importance of
avoiding C-section delivery for non-medical reasons,
especially before 39 weeks of gestation.
Physicians should carefully consider the
implications of our findings before they recommend
or agree to perform C-section delivery. Moreover,
physicians should understand the consequences of
performing C-section deliveries at lower full-term
gestational ages; our study and previous literature7 8
suggest that these consequences include worse
developmental outcomes. In particular, physicians
should consider whether a woman has reached
39 weeks of gestation because the ACOG strongly
discourages medically unnecessary C-section
delivery before 39 weeks.13 Considering that repeat
C-section is the most common reason for medically
unnecessary C-section delivery, physicians and
pregnant women should be informed that vaginal
delivery after a previous C-section is a safe and
feasible option for women without other medical
reasons to deliver by C-section. Finally, given that
some women request C-section delivery because
they fear pain, we recommend that physicians and
hospitals establish consultation and support systems
to help pregnant women understand what to expect
during delivery and to provide guidance concerning
labour pain relief. Increased communication and
support from physicians and nurses has been shown to reduce the fear of childbirth that leads
some women to request C-section delivery41; such
approaches may also be effective in China.
There were four main limitations in this study. First, because the recorded reasons for C-section
delivery were based on caregiver recall, we could
not rule out the potential for recall bias. Second,
although we included adjustment for potential
confounding factors, many other potential
confounding factors might have influenced the
findings. Third, our survey sample comprised
villages in one low-income region of rural China.
Although we attempted to sample villages that
differed in terms of household income, population
size, distance from the county seat, and geographic
location, our sample might not be representative
of all households in rural China. Finally, our study
sought to improve the understanding of medically
unnecessary C-section delivery and its associations
with gestational age and childhood developmental
outcomes—we could not regard these as causal
associations because of the cross-sectional nature
of our dataset. Therefore, in the absence of further
analysis, we could not determine whether medically
unnecessary C-section delivery was associated with
suboptimal childhood developmental outcomes,
and we could not characterise the mechanisms that
underlay associations identified in our study. Future research is needed to clarify the pathophysiological
mechanisms by which medically unnecessary
C-section delivery among children born at full
term is negatively associated with early childhood
developmental outcomes.
Conclusion
Among children born at full term, levels of cognitive,
language, and motor development increased with
increasing gestational age. However, C-section
delivery was negatively associated with gestational
age. A considerable proportion of deliveries in rural
China involved medically unnecessary C-section.
Therefore, the rate of medically unnecessary
C-section delivery, especially when this delivery
method is chosen based on a desire for repeat
C-section, should be reduced. Physicians should
carefully consider the potential consequences
when they recommend or agree to perform C-section
delivery; they should also provide detailed
information that helps pregnant women to gain
greater knowledge about childbirth.
Author contributions
Concept or design: S Li, A Yue.
Acquisition of data: A Yue.
Analysis or interpretation of data: S Li, A Yue.
Drafting of the manuscript: S Li, W Zheng, Q Jiang, Y Li, Y Shi.
Critical revision of the manuscript for important intellectual content: A Yue.
Acquisition of data: A Yue.
Analysis or interpretation of data: S Li, A Yue.
Drafting of the manuscript: S Li, W Zheng, Q Jiang, Y Li, Y Shi.
Critical revision of the manuscript for important intellectual content: A Yue.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
As an International Editorial Advisory Board member of the journal, Y Shi was not involved in the peer review process. Other authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank Dr Y Gao for contributing to the interpretation of data with this study.
Funding/support
This study was supported by a grant from the National Natural Science Foundation of China (Ref 71703083). The funder had no role in study design, data collection/analysis/interpretation or manuscript preparation.
Ethics approval
This study was approved by the Stanford University Institutional Review Board (Ref 35921). Informed consent
was obtained from all participants involved in the study.
References
1. Groeschel S, Tournier JD, Northam GB, et al. Identification
and interpretation of microstructural abnormalities in
motor pathways in adolescents born preterm. NeuroImage 2014;87:209-19.Crossref
2. Peterson BS, Vohr B, Staib LH, et al. Regional brain volume abnormalities and long-term cognitive outcome in preterm infants. JAMA 2000;284:1939-47.Crossref
3. Yang S, Bergvall N, Cnattingius S, Kramer MS. Gestational age differences in health and development among young Swedish men born at term. Int J Epidemiol 2010;39:1240-9. Crossref
4. Davis EP, Buss C, Muftuler LT, et al. Children’s brain development benefits from longer gestation. Front Psychol 2011;2:1. Crossref
5. Zacharia A, Zimine S, Lovblad KO, et al. Early assessment
of brain maturation by MR imaging segmentation in and
premature infants. AJNR Am J Neuroradiol 2006;27:972-7.
6. Kinney HC. The near-term (late preterm) human brain and risk for periventricular leukomalacia: a review. Semin Perinatol 2006;30:81-8. Crossref
7. Rose O, Blanco E, Martinez SM, et al. Developmental scores at 1 year with increasing gestational age, 37-41 weeks. Pediatrics 2013;131:e1475-81. Crossref
8. Espel EV, Glynn LM, Sandman CA, Davis EP. Longer gestation among children born full term influences cognitive and motor development. PLoS ONE 2014;9:e113758. Crossref
9. Yang S, Platt RW, Kramer MS. Variation in child cognitive ability by week of gestation among healthy term births. Am J Epidemiol 2010;171:399-406. Crossref
10. Noble KG, Fifer WP, Rauh VA, Nomura Y, Andrews HF.
Academic achievement varies with gestational age among
children born at term. Pediatrics 2012;130:e257-64. Crossref
11. Spong CY. Defining “term” pregnancy: recommendations
from the Defining “Term” Pregnancy Workgroup. JAMA
2013;309:2445-6. Crossref
12. Reddy UM, Bettegowda VR, Dias T, Yamada-Kushnir T,
Ko CW, Willinger M. Term pregnancy: a period of
heterogeneous risk for infant mortality. Obstet Gynecol
2011;117:1279-87. Crossref
13. American College of Obstetricians and Gynecologists.
ACOG Committee Opinion No. 761: cesarean delivery on
maternal request. Obstet Gynecol 2019;133:e73-7. Crossref
14. Davidoff MJ, Dias T, Damus K, et al. Changes in the
gestational age distribution among U.S. singleton births:
impact on rates of late preterm birth, 1992 to 2002. Semin
Perinatol 2006;30:8-15. Crossref
15. Bettegowda VR, Dias T, Davidoff MJ, Damus K,
Callaghan WM, Petrini JR. The relationship between
cesarean delivery and gestational age among US singleton
births. Clin Perinatol 2008;35:309-23, v-vi. Crossref
16. Ananth CV, Vintzileos AM. Trends in cesarean delivery at
preterm gestation and association with perinatal mortality.
Am J Obstet Gynecol 2011;204:505.e1-8. Crossref
17. Nassar N, Schiff M, Roberts CL. Trends in the distribution
of gestational age and contribution of planned births in
New South Wales, Australia. PLoS One 2013;8:e56238. Crossref
18. Gibbons L, Belizan JM, Lauer JA, Betran AP, Merialdi M,
Althabe FX. The global numbers and costs of additionally
needed and unnecessary caesarean sections performed
per year: overuse as a barrier to universal coverage. World
health report 2010;30:1-31.
19. Weaver JJ, Statham H, Richards M. Are there “unnecessary”
cesarean sections? Perceptions of women and obstetricians
about cesarean sections for nonclinical indications. Birth
2007;34:32-41. Crossref
20. Bettes BA, Coleman VH, Zinberg S, et al. Cesarean
delivery on maternal request: obstetrician-gynecologists’ knowledge, perception, and practice patterns. Obstet
Gynecol 2007;109:57-66. Crossref
21. Penna L, Arulkumaran S. Cesarean section for non-medical
reasons. Int J Gynecol Obstet 2003;82:399-409.Crossref
22. Karlström A, Nystedt A, Johansson M, Hildingsson I.
Behind the myth—few women prefer caesarean section in
the absence of medical or obstetrical factors. Midwifery
2011;27:620-7. Crossref
23. Mi J, Liu F. Rate of caesarean section is alarming in China.
Lancet 2014;383:1463-4. Crossref
24. Lumbiganon P, Laopaiboon M, Gülmezoglu AM, et al.
Method of delivery and pregnancy outcomes in Asia: the
WHO global survey on maternal and perinatal health
2007-08. Lancet 2010;375:490-9. Crossref
25. Long Q, Klemetti R, Wang Y, Tao F, Yan H, Hemminki E.
High caesarean section rate in rural China: is it related to
health insurance (New Co-operative Medical Scheme)?
Soc Sci Med 2012;75:733-7. Crossref
26. World Health Organization, United Nations Children’s
Fund. Monitoring Emergency Obstetric Care: a Handbook.
Geneva: World Health Organization; 2009.
27. Molina G, Weiser TG, Lipsitz SR, et al. Relationship
between cesarean delivery rate and maternal and neonatal
mortality. JAMA 2015;314:2263-70. Crossref
28. Sufang G, Padmadas SS, Fengmin Z, Brown JJ, Stones RW.
Delivery settings and caesarean section rates in China. Bull
World Health Organ 2007;85:755-62. Crossref
29. Deng W, Klemetti R, Long Q, et al. Cesarean section in Shanghai: women’s or healthcare provider’s preferences? BMC Pregnancy Childbirth 2014;14:285.Crossref
30. Li HT, Ye R, Achenbach TM, et al. Caesarean delivery
on maternal request and childhood psychopathology: a
retrospective cohort study in China. BJOG 2011;118:42-8. Crossref
31. Qian Y, Zheng YM, Dill SE, Rozelle S. Correlates of
participation in community-based interventions: evidence
from a parenting program in rural China. PLoS One
2020;15:e0238841. Crossref
32. Luo R, Shi Y, Zhou H, et al. Anemia and feeding practices
among infants in rural Shaanxi Province in China.
Nutrients 2014;6:5975-91. Crossref
33. Madaschi V, Mecca TP, Macedo EC, Paula CS. Bayley-III
scales of infant and toddler development: transcultural adaptation and psychometric properties. Paidéia
2016;26:189-97. Crossref
34. Azari N, Soleimani F, Vameghi R, et al. A psychometric study
of the Bayley scales of infant and toddler development in
Persian language children. Iran J Child Neurol 2017;11:50-6.
35. Bayley N. Bayley Scales of Infant and Toddler Development. 3rd ed. San Antonio (TX): Harcourt Assessment; 2006. Crossref
36. Xiao S, Yan H, Shen Y, et al. Utilization of delivery care among rural women in China: does the health insurance make a difference? A cross-sectional study. BMC Public Health 2010;10:695. Crossref
37. Liang J, Mu Y, Li X, et al. Relaxation of the one child policy
and trends in cesarean section rates and birth outcomes in
China between 2012 and 2016: observational study of nearly
seven million health facility births. BMJ 2018;360:k817. Crossref
38. Aksoy M, Aksoy AN, Dostbil A, Celik MG, Ince I. The
relationship between fear of childbirth and women’s
knowledge about painless childbirth. Obstet Gynecol Int
2014;2014:274303. Crossref
39. Campbell DA, Lake MF, Falk M, Backstrand JR. A randomized control trial of continuous support in labor by a lay doula. J Obstet Gynecol Neonatat Nurs 2006;35:456-64. Crossref
40. Hodnett ED, Gates S, Hofmeyr GJ, Sakala C. Continuous support for women during childbirth. Birth 2005;32:72. Crossref
41. Flink IK, Mroczek MZ, Sullivan MJ, Linton SJ. Pain
in childbirth and postpartum recovery: the role of
catastrophizing. Eur J Pain 2009;13:312-6. Crossref
42. Cheung W, Ip WY, Chan D. Maternal anxiety and feelings
of control during labour: a study of Chinese first-time
pregnant women. Midwifery 2007;23:123-30. Crossref
43. Wang E. Requests for cesarean deliveries: the politics of
labor pain and pain relief in Shanghai, China. Soc Sci Med
2017;173:1-8. Crossref
44. Geissbuehler V, Eberhard J. Fear of childbirth during
pregnancy: a study of more than 8000 pregnant women. J
Psychosom Obstet Gynecol 2002;23:229-35. Crossref
45. MacDorman MF, Mathews TJ, Martin JA, Malloy MH.
Trends and characteristics of induced labour in the United
States, 1989-98. Paediatr Perinat Epidemiol 2010;16:263-73. Crossref