Hong Kong Med J 2022 Apr;28(2):178–80 | Epub 8 Apr 2022
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Pain management for painful brachial neuritis
after COVID-19: a case report
Vivian YT Cheung, MB, BS, FHKAM (Anaesthesiology); Fiona PY Tsui, MB, BS, FHKAM (Anaesthesiology); Joyce MK Cheng, BHlthSc, FHKAN (Perioperative)
Department of Anaesthesia, Pamela Youde Nethersole Eastern Hospital, Hong Kong
Corresponding author: Dr Vivian YT Cheung (cyt086@ha.org.hk)
Case report
In October 2020, a 55-year-old Chinese man
travelled from Hong Kong to Paris to attend a family
funeral. He had psoriatic arthropathy in remission
without chronic pain. In November 2020 while still
in France, he and seven family members developed
fever and upper respiratory symptoms, confirmed to
be coronavirus disease 2019 (COVID-19). The family
remained in home isolation and required no medical
treatment. The patient self-treated with traditional
Chinese medication: Lianhua Qingwen herbal
capsules for 1 week. Two weeks later, he returned
to Hong Kong after testing negative for COVID-19.
In December 2020, during mandatory quarantine
on re-entry to Hong Kong, the patient suddenly
developed pain that extended from the neck and
right interscapular region to the shoulder and down
along the ulnar side of the right arm and forearm. The
patient described the pain as shooting and drilling in
nature, constantly severe, worst at the interscapular
region, and aggravated by shoulder movement.
He also reported disturbed sleep and numbness
over his entire right arm and weakened right hand
grip. He had no other joint pain, rash, vesicles, or
fever. At this time, he was still resting alone in a
quarantine hotel and performing no physical work.
Most activities of daily living were manageable but
some, such as bathing and dressing, were difficult.
Diclofenac 100 mg daily and gabapentin 200 mg
3 times daily prescribed at a COVID-19 Clinic were
ineffective. The patient’s younger sister who had
recovered in France without medication reported
similar symptoms in her left arm.
The patient presented to our pain clinic
1 month after pain onset. His motor symptoms had
spontaneously improved although disturbing right
shoulder and interscapular pain with paraesthesia
persisted. There were no muscle wasting, scar, rash,
or trophic changes. The patient’s right arm was
slightly warmer than the left, and upper limb joints
were not swollen or tender and there was full range
of movement. He reported decreased sensation to
light touch, cold and pinprick over the whole right
arm, but his sense of vibration and proprioception
were preserved. No touch or mechanical allodynia or hyperalgesia were noted. Apart from slightly
weakened thumb opposition, other muscle strength,
tendon reflexes and neck examination were
unremarkable.
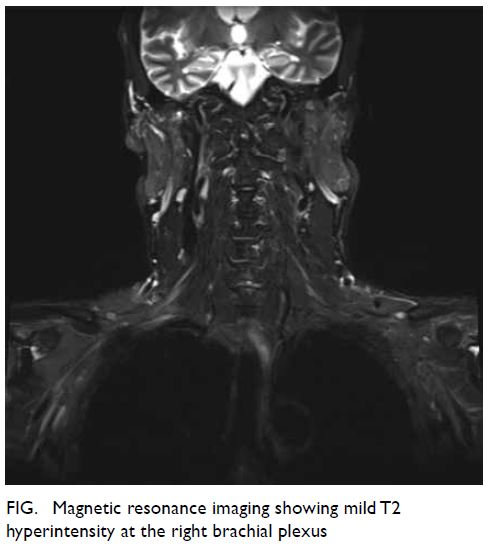
Analgesia was changed to pregabalin 75 mg
twice per day and etoricoxib 90 mg daily as needed,
and the patient was referred for occupational
therapy for grip strengthening. Magnetic resonance
imaging (MRI) in March 2021 revealed mild T2
hyperintensity at the right brachial plexus, suggestive
of resolving neuritis (Fig). There was also cervical
spondylosis without significant intervertebral
foraminal narrowing or cord compression. Nerve
conduction study in March 2021 was normal.
Electromyography was not performed due to good
neurological recovery.
At a subsequent 3-month follow-up
examination in March 2021, the patient reported
continued improvement with little or no pain. He
reported only intermittent paraesthesia and mild
weakness of his right hand and fingers. As a right-hander,
he continued to have trouble turning keys and
using chopsticks and pens. He coped with his office work with a speech-to-text converter to minimise
keyboard usage. He could manage most household
chores, including shopping for groceries, and slept
well. He was calm and grieving appropriately for the
loss of his mother. Pregabalin was gradually reduced,
and he was weaned off etoricoxib.
Discussion
The Coronavirus family is known for its neurotropism
with 36% of COVID-19 infected patients reporting
some form of neurological manifestation.1
Mechanisms involve direct neural infection,
and indirect inflammatory and immunological
reactions. Other possibilities are targeting of
neuronal angiotensin-converting enzyme 2,
vasculitis, thrombosis and iatrogenic, such as prone
position-related effects or neuropathies.2
The pathophysiology of acute brachial neuritis is not well understood but the pre-existence of viral
infection supports immunological mechanisms.
Affected subjects have more lymphocytic activity
to brachial (versus sacral) plexus nerve extracts and
increased antibodies to peripheral nerve myelin. A
hereditary form with mutation-related deficiency in
proteins from the septin family has been identified.2
Our patient took Lianhua Qingwen, a traditional
Chinese medicine prepared from 13 herbs, shown to
bind to angiotensin-converting enzyme 2 and shorten
the course of COVID-19 infection.3 Drug-induced
plexopathy, although less likely, remains possible.
Acute brachial neuritis is self-limiting but
classically presents with excruciating pain at the
shoulder, neck and interscapular region, followed by
shoulder girdle weakness. Diagnosis is clinical and
investigations are supportive. Cervical pathology is
the major differential diagnosis but was excluded in
our patient by MRI that revealed cervical spondylosis
without nerve or cord compression or signal changes.
Given the rheumatological history in our case, active
autoimmune disease was also possible, but he had no
such features.
To the best of our knowledge three cases of
post-COVID-19 brachial neuritis4 5 6 have been
reported but none in Hong Kong. Brachial neuritis
is rare with an incidence of only 1.64 cases per
100 000 person-years, and underreporting is
expected with isolation and restricted healthcare
access during COVID-19. Compared to existing
three cases, two cases similarly involved middle-aged
men with delayed neuropathic symptoms
2 weeks after COVID-19 confirmation. One had
similar symptoms to our patient, whereas the other
two had either purely sensory components or solely
proximal median nerve involvement. Our case
and one existing case demonstrated classical MRI
changes. Nerve conduction study in our patient did
not demonstrate reduced action potential amplitude
in affected nerves, which may have been related to its performance at a later course of the disease.
Given the rarity of the entity and its occurrence
in our patient and his sister, further research to
investigate the role of genetic susceptibility to the
acute form is warranted. Management of brachial
neuritis is supportive and focused on pain control
and functional rehabilitation with physiotherapy and
occupational therapy. There is limited evidence that
steroids and immunoglobulins will hasten recovery
so their use should be balanced against the risk of
viral replication. Currently, there are no established
guidelines for pain management in patients with
or recently recovered from COVID-19. Specific
precautions should be taken in pain management of
these cases.
Paracetamol has limited efficacy for neuropathic
pain. Care should be taken for patients with severe
COVID-19, because viral-induced cytokine storm
can suppress cytochrome P450, increasing the risks
of hepatotoxicity. Nonsteroidal anti-inflammatory
drugs offer effective analgesia for brachial neuritis
by suppressing cyclooxygenase and prostaglandin
production. Although there were early concerns
about ibuprofen-associated decompensation
in patients with COVID-19, this has not been
supported by the World Health Organization after
data review. Meanwhile, cyclooxygenase-2 selective
nonsteroidal anti-inflammatory drugs disturb the
thromboxane A2–prostacyclin balance, potentially
enhancing thrombotic tendency in patients with
COVID-19. Our case illustrates the safe use of
cyclooxygenase-2 inhibitors in a patient recently
recovered from COVID-19. Among antineuropathic
agents, gabapentinoids have relatively few adverse
effects, lower cardiac toxicity, and fewer drug-drug
interactions than tricyclic antidepressants and
serotonin-noradrenaline reuptake inhibitors. Our
patient was initially prescribed a relatively low dose
of gabapentin that may account for its lack of effect.
He was changed to pregabalin at a higher equivalent
dose, with a better pharmacological profile with
linear dose-response relationship and faster onset.
Physicians should be alert to the sedative effects
of analgesia that may worsen COVID-19-related
ventilatory impairment. Opioids should be reserved
for severe refractory pain.
Pain management for patients with or
recently recovered from COVID-19 can be socially
challenging. The need for quarantine delays
presentation and management, and the associated
mental stress and lack of social support may
perpetuate pain. Although telemedicine enables
remote medical care, controversies remain, and
psychological engagement is less effective. Our
patient’s appropriate grief reaction and illness coping
mechanism minimises risk of chronic pain.
Our case report is the first to focus on the
clinical management of brachial neuritis in patients with or recently recovered from COVID-19, and the
first to identify a possible case series within a family.
We hope our report of COVID-19-related brachial
neuritis can promote awareness and understanding.
Future research should focus on its pathophysiology
including genetic susceptibility. Whether COVID-19 vaccination alters the course of acute brachial
neuritis warrants further observation.
Author contributions
Concept or design: VYT Cheung, FPY Tsui.
Acquisition of data: VYT Cheung, JMK Cheng.
Analysis or interpretation of data: VYT Cheung.
Drafting of the manuscript: VYT Cheung.
Critical revision of the manuscript for important intellectual content: FPY Tsui, JMK Cheng.
Acquisition of data: VYT Cheung, JMK Cheng.
Analysis or interpretation of data: VYT Cheung.
Drafting of the manuscript: VYT Cheung.
Critical revision of the manuscript for important intellectual content: FPY Tsui, JMK Cheng.
All authors had full access to the data, contributed to the
study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
We would like to thank Dr Annie Chu for contributing to the
clinical management, and Drs Mandy Au Yeung and Kendrick
Tang for the investigations.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration
of Helsinki. The patient provided informed consent for the
treatment/procedures, and for publication.
References
1. Mao L, Jin H, Wang M, et al. Neurologic manifestations
of hospitalized patients with coronavirus disease 2019 in
Wuhan, China. JAMA Neurol 2020;77:683-90. Crossref
2. Fernandez CE, Franz CK, Ko JH, et al. Imaging review
of peripheral nerve injuries in patients with COVID-19.
Radiology 2021;298:E117-30. Crossref
3. Alam S, Sarker MM, Afrin S, et al. Traditional herbal
medicines, bioactive metabolites, and plant products
against COVID-19: update on clinical trials and mechanism
of actions. Front Pharmacol 2021;12:671498. Crossref
4. Mitry MA, Collins LK, Kazam JJ, Kaicker S, Kovanlikaya A.
Parsonage-turner syndrome associated with SARS-CoV2
(COVID-19) infection. Clin Imaging 2021;72:8-10. Crossref
5. Siepmann T, Kitzler HH, Lueck C, Platzek I, Reichmann H,
Barlinn K. Neuralgic amyotrophy following infection with
SARS-CoV-2. Muscle Nerve 2020;62:E68-70. Crossref
6. Cacciavillani M, Salvalaggio A, Briani C. Pure sensory
neuralgic amyotrophy in COVID-19 infection. Muscle
Nerve 2021;63:E7-E8. Crossref