© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Paediatric acute respiratory distress syndrome
and haemophagocytic lymphohistiocytosis
complications of scrub typhus: a case report
Ronald CM Fung, MB, ChB, MRCPCH1; Karen KY Leung, MB, BS, MRCPCH1; CC Au, MB, BS, MRCPCH2; KN Cheong, MB, BS, MRCPCH2; Mike YW Kwan, MRCPCH3; Grace KS Lam, MB, BS, MRCPCH2; KL Hon, MB, BS, MD1
1 Paediatric Intensive Care Unit, Department of Paediatrics and Adolescent Medicine, The Hong Kong Children’s Hospital, Hong Kong
2 Department of Paediatrics and Adolescent Medicine, The Hong Kong Children’s Hospital, Hong Kong
3 Department of Paediatrics and Adolescent Medicine, Prince Margaret Hospital, Hong Kong
Corresponding author: Dr KL Hon (ehon@hotmail.com)
In June 2020, a previously healthy 7-year-old boy
presented with a 1-week history of persistent fever.
He had an unremarkable medical history, and had
gone hiking a week before the onset of his fever.
He was initially treated for a presumed viral illness
but his condition worsened over the subsequent
2 days. His fever became high and fluctuating, with
a peak of 39°C, and he developed dyspnoea without
cough. He had no headache or body aches. Physical
examination revealed crepitations with diminished
breath sounds over both lung fields and tachypnoea
with a respiratory rate of 30 per minute. Cervical
lymphadenopathy and hepatomegaly were present.
There was no eschar. He had distributive shock
with hypotension (80/40 mm Hg) and tachycardia
(150 beats per minute) and a norepinephrine
infusion was commenced. Within one day, type I respiratory failure became evident with increasing
oxygen requirement from room air to FiO2 0.4 and
continuous positive airway pressure of 6 cmH2O
to maintain oxygen saturation above 90%. The
PaO2:FiO2 ratio was 232.5 mm Hg. Plain radiograph
of the chest revealed bilateral opacities and
peribronchial thickening (Fig). Echocardiography
and lung ultrasound confirmed normal heart
function and the absence of pleural effusion. By
definition, the boy was diagnosed with paediatric
acute respiratory distress syndrome (PARDS: an
acute lung injury occurring within 7 days of a
known clinical insult, with acute hypoxaemia of
PaO2:FiO2 ratio ≤300 when the child is on non-invasive
ventilation, and new infiltrates consistent
with acute pulmonary parenchymal disease on
chest radiograph, which cannot be explained by acute left ventricular heart failure or fluid overload),
where he had progressive respiratory failure and
bilateral diffuse infiltration on chest radiography.1
Further blood tests and bone marrow findings
met the diagnostic criteria for haemophagocytic
lymphohistiocytosis (HLH: a life-threatening
clinical syndrome of systemic hyperinflammation
and progressive immune-mediated organ damage due to excessive immune activation): anaemia
(haemoglobin 8.3 g/dL), thrombocytopenia
(45 × 109/L), hypertriglyceridaemia (4.5 mmol/L),
high ferritin (4467 pmol/L), hypofibrinogenaemia
(0.9 g/L), and elevated soluble CD25 (8569 pg/mL).2
Bone marrow aspiration and trephine biopsy
showed haemophagocytosis. There was no
evidence of Epstein–Barr virus association
on immunohistochemical analysis. Orientia
tsutsugamushi antibody titre of 512 increased to
4096 (ie, more than a fourfold increase) after 2 weeks.
The child was diagnosed with PARDS and secondary
HLH associated with scrub typhus infection and prescribed oral doxycycline 50 mg twice daily
(~3.7 mg/kg/day) for the scrub typhus. Intravenous
dexamethasone 5 g every 12 hours (10 mg/m2/day)
was commenced as treatment of HLH with a starting
dose as per the HLH-2004 study protocol. He became
afebrile within 1 day of commencing treatment
and respiratory distress gradually resolved. He was
weaned off continuous positive airway pressure
ventilation after 3 days. Platelet count rose to
>100 × 109/L after 4 days. Ferritin lowered the day
after treatment and was within normal range after
2 weeks. The boy completed a 1-week course of
doxycycline and dexamethasone was also tapered off
in 1 week.
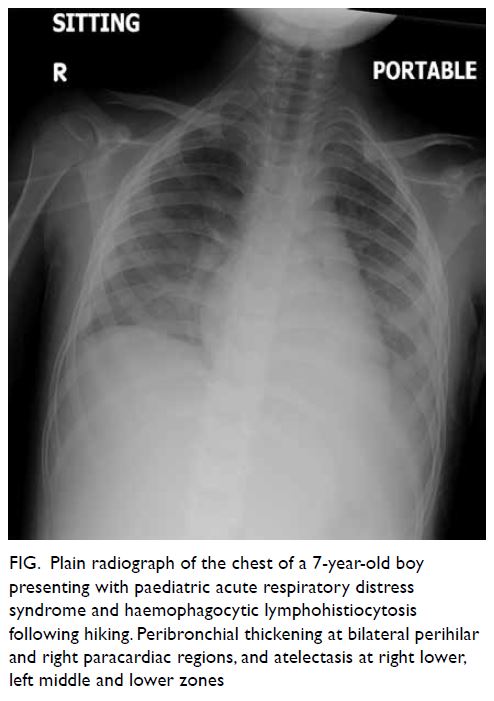
Figure. Plain radiograph of the chest of a 7-year-old boy presenting with paediatric acute respiratory distress syndrome and haemophagocytic lymphohistiocytosis following hiking. Peribronchial thickening at bilateral perihilar and right paracardiac regions, and atelectasis at right lower, left middle and lower zones
Discussion
Our patient presented with non-specific
symptoms of scrub typhus and developed severe
complications including PARDS and HLH without
the pathognomonic eschar. Scrub typhus is caused
by the bacterium O tsutsugamushi and is spread
to humans through the bites of infected chiggers,
Leptotrombidium mites, that can be both a vector
and a reservoir for O tsutsugamushi.3 It is a notifiable
disease in Hong Kong with between 7 and 28 cases
reported each year over the past 10 years.4 Symptoms
of scrub typhus usually begin within 10 days of
being bitten and can range from non-specific signs
including fever, headache, body aches and rash, to
multiorgan failure and death with a median mortality
rate of 6% if left untreated.3 Although eschar is
pathognomonic for scrub typhus, it is rare among
Southeast Asian patients. Laboratory confirmation
of the diagnosis usually requires indirect fluorescent
antibody test and is the mainstay of serologic
diagnosis. Polymerase chain reaction assay of whole
blood sample if available can speed the diagnosis.
Acute respiratory distress syndrome is a serious
complication of scrub typhus; it has been reported in
4% to 22% of cases,5 6 and can involve over 50% of
children who developed secondary HLH associated
with scrub typhus infection.7 The pulmonary
manifestations vary from bronchitis and interstitial
pneumonitis to acute respiratory distress.5 6 Acute
respiratory distress has also manifested in many
patients with HLH due to other causes and has been
reported as the initial manifestation of HLH. Nahum
et al8 reported that 7 of 11 children with HLH and
multiple organ failure exhibited PARDS after HLH
was diagnosed, highlighting the importance of close
monitoring and early intervention for children
with PARDS and HLH. The presentation of acute
respiratory distress syndrome in children differs from
that in adults and a consensus on a formal PARDS
definition was reached in 2015 by the Paediatric
Acute Lung Injury Consensus Conference.1
In some cases, HLH can cause cytokine release syndrome, a life-threatening disorder of
severe excessive inflammation (hyperinflammation)
caused by uncontrolled proliferation of activated
lymphocytes, macrophages and secretion of
inflammatory cytokines.9 Although rare, O
tsutsugamushi is a significant cause of HLH,
especially in Asia.7 The HLH-2004 protocol,
which includes etoposide, dexamethasone and
cyclosporine as the initial therapy, is designed
for treatment of patients with primary HLH.2 For
patients with secondary HLH, treatment of the
underlying infection or malignancy may help control
the HLH and avoid the need for cyclosporine and
etoposide. Single antibiotic therapy with doxycycline,
minocycline, chloramphenicol, azithromycin or
clarithromycin has been reported to result in rapid
defervescence in patients with HLH associated
with scrub typhus.10 Thus, an accurate diagnosis of
scrub typhus in patients with HLH can help timely
targeted antibiotic therapy with subsequent rapid
clinical improvement.
This case illustrates an atypical severe
manifestation of scrub typhus presenting with
non-specific signs and symptoms resulting in
complications including PARDS and HLH. Early
diagnosis and treatment with doxycycline are crucial
to prevent complications. Physicians should be
vigilant for scrub typhus as a potential diagnosis
in a child who presents with pyrexia of unknown
origin and a history of participation in rural outdoor
activities.
Author contributions
Concept or design: RCM Fung, KKY Leung, CC Au, KL Hon.
Acquisition of data: RCM Fung, KL Hon.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: RCM Fung, KKY Leung, KL Hon.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: RCM Fung, KL Hon.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: RCM Fung, KKY Leung, KL Hon.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, KL Hon was not involved in the peer review process. Other authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the tenets of the Declaration of Helsinki. The patient’s parents provided
written informed consent for all treatments and procedures
and consent for publication.
References
1. Pediatric Acute Lung Injury Consensus Conference
Group. Pediatric acute respiratory distress syndrome:
consensus recommendations from the Pediatric Acute
Lung Injury Consensus Conference. Pediatr Crit Care Med
2015;16:428-39. Crossref
2. Henter JI, Horne A, Aricó M, et al. HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic
lymphohistiocytosis. Pediatr Blood Cancer 2007;48:124-31. Crossref
3. Peesapati N, Rohit T, Sunitha S, Pv S. Clinical manifestations and complications of scrub typhus: a hospital-based study from North Andhra. J Assoc Physicians India 2019;67:22-4.
4. Center for Health Protection, Department of Health, Hong
Kong SAR Government. Number of notifiable infectious
diseases by month. 2020. Available from: https://www.chp.gov.hk/en/statistics/data/10/26/43/6896.html. Accessed 25 Jun 2020.
5. Sankuratri S, Kalagara P, Samala KB, Veledandi PK, Crossref
6. Kumar Bhat N, Dhar M, Mittal G, et al. Scrub typhus in children at a tertiary hospital in north India: clinical profile and complications. Iran J Pediatr 2014;24:387-92.
7. Naoi T, Morita M, Kawakami T, Fujimoto S. Hemophagocytic lymphohistiocytosis associated with
scrub typhus: Systematic review and comparison between
pediatric and adult cases. Trop Med Infect Dis 2018;3:19. Crossref
8. Nahum E, Ben-Ari J, Stain J, Schonfeld T. Hemophagocytic lymphohistiocytic syndrome: Unrecognized cause of
multiple organ failure. Pediatr Crit Care Med 2000;1:51-4. Crossref
9. Hon KL, Leung KK, Oberender F, Leung AK. Paediatrics: how to manage septic shock. Drugs Context 2021;10:2021-1-5. Crossref
10. Hon KL, Leung AS, Cheung KL, et al. Typical or atypical
pneumonia and severe acute respiratory symptoms in
PICU. Clin Respir J 2015;9:366-71. Crossref

