Hong Kong Med J 2022 Feb;28(1):7–15 | Epub 18 Feb 2022
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Clinical outcomes of fast-track total knee
arthroplasty for patients aged >80 years
TP Leung, MB, ChB; CH Lee, FHKCOS, FHKAM (Orthopaedic Surgery); Esther WY Chang, MSc; QJ Lee, FHKCOS, FHKAM (Orthopaedic Surgery); YC Wong, FHKCOS, FHKAM (Orthopaedic Surgery)
Joint Replacement Centre, Yan Chai Hospital, Hong Kong
Corresponding author: Dr TP Leung (fos.markleung@gmail.com)
Abstract
Introduction: Because of the ageing population in
Hong Kong, there is an increasing incidence of total
knee arthroplasties (TKA) conducted in patients
aged >80 years.
Methods: This retrospective case-control study enrolled all patients who were aged >80 years and
underwent fast-track primary TKA between 2011
and 2015. Their outcomes were compared with the
outcomes of a matched control group of younger
patients who underwent fast-track TKA in the same
period.
Results: In total, 220 patients were included in this
study with a follow-up period of at least 2 years
(mean=3.2 years; range, 2-5 years); 112 (51%)
were octogenarians and 108 (49%) were non-octogenarians.
Greater improvement in Knee
Society Score was found in the octogenarian group
at 1 year after surgery (46 ± 19 vs 39 ± 16, P=0.018).
The incidence of complications was higher in the
octogenarian group (15.2% vs 4.6%, P=0.009). There
were no significant differences in the incidence of
major complications, the rate of intensive care unit
admission, or the 1-year mortality rate between the two groups. After adjustment for confounding
factors, Charlson Comorbidity Index >5, history of
major cerebrovascular accident, and history of peptic
ulcer disease were predictive of complications after
fast-track TKA (P=0.039, P=0.016, and P=0.007,
respectively); octogenarian status was not predictive
of complications.
Conclusions: Octogenarians had greater
improvement in Knee Society Score at 1 year after
fast-track TKA, compared with non-octogenarians,
but there were no significant differences in the
incidences of mortality or major complications.
New knowledge added by this study
- The octogenarian group exhibited greater improvement in functional outcomes after fast-track total knee
arthroplasty, compared with younger patients.
- Charlson Comorbidity Index >5, history of major cerebrovascular accident, and history of peptic ulcer disease
were predictive of complications after fast-track total knee arthroplasty.
- Age alone should not be a contra-indication to total knee arthroplasty because there were no significant differences in major complications or mortality rate for patients aged >80 years who underwent fast-track total knee arthroplasty.
- Fast-track total knee arthroplasty could be useful for managing the growing osteoarthritis burden among older adults in Hong Kong, thus improving their quality of life.
Introduction
Because of the ageing population in Hong Kong,
the incidence of total knee arthroplasty (TKA) for
patients aged >80 years is expected to increase.1 2
The optimal age for arthroplasty has generally been
regarded as between 60 and 80 years. Age was
previously identified as an independent risk factor
for mortality and major complications after TKA. For
example, Kreder et al3 reported a 2.5-fold increase
in the risk of acute myocardial infarction and a
3.4-fold increase in mortality among octogenarians undergoing TKA, compared with a cohort aged 65
to 79 years. Arthroplasties in patients aged >80 years
were declined by surgeons or patients because of the
expected high rates of postoperative morbidity and
mortality.4 5 6
With preoperative preparations intended to
minimise perioperative complications and blood
loss, a recent study suggested that TKA could be
a safe procedure among patients aged >80 years.7
The incidences of TKA in patients aged >80 years
have been increasing in various knee registries.8 9 10 11 12 However, the traditional approach of declining knee
arthroplasties in patients aged >80 years remains
popular in Hong Kong. This approach does not meet
the increasing needs of the ageing population.
The current study investigated whether
octogenarians could achieve similar clinical
outcomes after TKA, compared with younger
patients. The null hypothesis was that short-term
function and complications would not significantly
differ between patients aged >80 years and patients
aged ≤80 years after fast-track primary TKA.
Methods
Study design and setting
This retrospective case-control study was carried out in the Total Joint Replacement Centre in Yan
Chai Hospital in Hong Kong between 2011 and
2015. The results of TKA procedures performed in
the institute during the study period were reviewed;
all patients were followed up for at least 2 years
(mean=3.2 years; range, 2-5 years).
Study population
All patients who were aged >80 years and underwent
primary TKA during the study period were included
in the analysis. Their outcomes were compared with
the outcomes in a similar number of younger patients
(aged ≤80 years) with a matched sex ratio and body
mass index (BMI). The indications for TKA were
primary osteoarthritis of the knee and rheumatoid
arthritis of the knee. The exclusion criteria in this
study were revision TKA and simultaneous bilateral TKA. The contra-indications for TKA in both groups
included active local or remote infection, poor skin
condition, recent stroke and myocardial infarction
(ie, within 1 year), poor cardiopulmonary reserve
(eg, congestive heart failure and chronic obstructive
pulmonary disease), and cirrhosis. For patients who
had undergone percutaneous coronary intervention
involving dual antiplatelet therapy, TKA was delayed
for 1 year.
Data retrieval and measurement
Data retrieval was performed using the Clinical Management System in our institute. The procedure
code for retrieval was ‘81.54 total knee replacement’.
All operative records and out-patient records
were reviewed. All outcome measurements were
performed by independent observers (ie, orthopaedic
specialist nurses) who were blinded to the details of
treatment.
Baseline characteristic and outcome variables
Baseline characteristics were compared between
the two groups; these included age, sex, BMI,
co-morbidities, Charlson Comorbidity Index,
preoperative haemoglobin level, and type of
anaesthesia. Primary outcome measures included
the knee range of motion (ROM), Knee Society Score
(KSS), Western Ontario and McMaster Universities
Osteoarthritis Index (WOMAC), complication
rates, and mortality rates. Secondary outcome
measures included the need for blood transfusion,
postoperative admission to the intensive care unit
(ICU), length of hospitalisation ,and postoperative
ambulatory status.
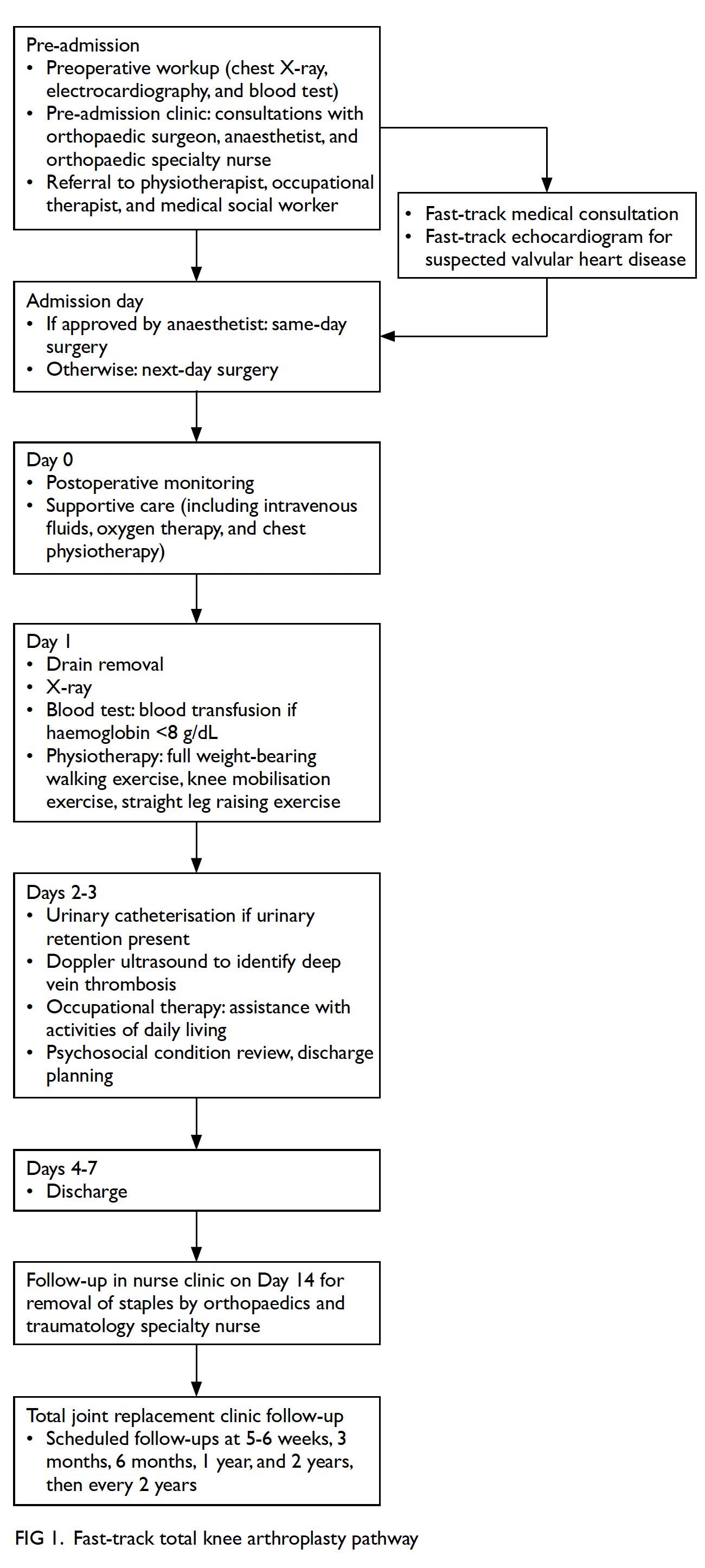
Fast-track protocol
Using the fast-track protocol, a multidisciplinary
approach was adopted in the perioperative period
(Fig 1). Patients were examined in the pre-admission
clinic by an orthopaedic surgeon, an anaesthetist,
and an orthopaedic specialty nurse. Preoperative
workups with blood tests (eg, complete blood
count, liver function test, renal function test,
random glucose, and haemoglobin), chest X-rays,
and electrocardiography were performed in the
pre-admission clinic. Blood pressure and BMI
measurements were also conducted in the pre-admission
clinic; blood pressure <160/90 mm Hg
was required. The presence of local skin problems
and other acute infections (eg, skin, oral, or
urinary tract) were ruled out. Previous histories of
deep vein thrombosis (DVT), bleeding tendency,
gastrointestinal bleeding, and haemorrhagic stroke
were recorded. Finally, other pre-existing medical
conditions (eg, thyroid disease and obstructive
sleep apnoea) were evaluated in the pre-admission
clinic. The anaesthetist carried out a preoperative assessment and determined the anaesthesia
modality (general or spinal); spinal anaesthesia was
preferred unless contra-indicated. If patients had
poorly controlled hypertension and diabetes, they
were referred to a fast-track pathway for assessment
by a family physician to optimise and titrate medical
therapy for hypertension and diabetes. Fast-track
echocardiography was also conducted with support
from cardiologists to assess baseline cardiac function
and suspected valvular problems. After patients had
received explanations of TKA, as well as its benefits
and risks, they provided written informed consent to
undergo the surgical procedure.
Education to manage patient expectations was
conducted by a nursing specialist. Prior to surgery,
a physiotherapist provided patients with education
concerning the rehabilitation pathway (ie, exercise,
home care, and the arrangement of walking aids). An
occupational therapist performed an Activities of
Daily Living assessment and conducted appropriate
home modifications. A medical social worker
performed a psychosocial assessment and discharge
planning; for patients with anticipated discharge
problems, short-term placement was arranged
prior to surgery. The aim of this multidisciplinary
preoperative preparation protocol was to reduce the
in-patient period and promote early postoperative
ambulation for successful rehabilitation.
Most patients were admitted for same-day
surgery. If the anaesthetist requested a short period
of monitored preoperative optimisation, patients
were admitted for next-day surgery. The criteria for
next-day surgery included the presence of insulin-dependent
diabetes mellitus requiring overnight
dextrose-potassium-insulin infusion, the presence
of chronic obstructive pulmonary disease, and the
need for pacemaker adjustment prior to surgery.
Surgical techniques and perioperative
management
All arthroplasties were performed via the medial parapatellar approach using a tourniquet, a
posterior-stabilised implant, and a bone plug in the
intramedullary canal or navigation without canal
violation, followed by cementation, haemostasis
with a tourniquet, a compression bandage, and
low-suction pressure drainage at 200 mm Hg for
24 hours. For 4 days after surgery, the analgesic
regimen included acetaminophen 1 g 4 times daily
and sustained-release oral diclofenac 100 mg daily for
4 days. Patients were provided a patient-controlled
analgesia pump with intravenous morphine.
Continuous femoral nerve block was performed.
Patients were reviewed by Acute Pain Service staff
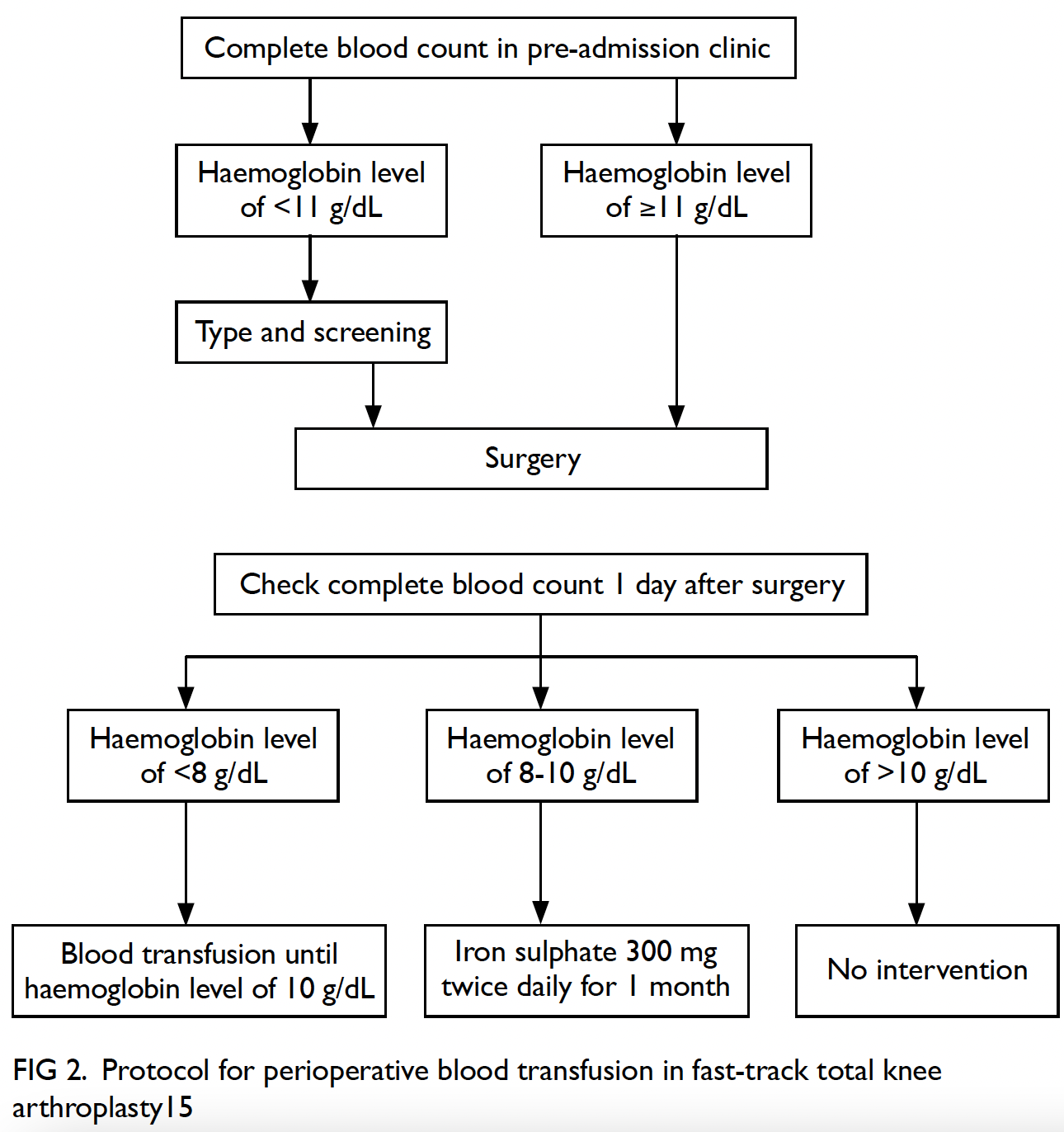
beginning on postoperative day 0. The complete
blood count was checked on postoperative day 1.
For patients with a haemoglobin level <8 g/dL, blood transfusion was initiated until the haemoglobin
level reached 10 g/dL (Fig 2). Ice therapy, walking,
and ROM exercise were initiated on day 1. A foot
pump was used for mechanical DVT prophylaxis
throughout the hospital stay. Pharmacological
prophylaxis for DVT was initiated only in patients
with a history of venous thromboembolism.
Nursing specialists assessed the wound, dressing,
and drain; they also conducted fall risk assessment
and prevention. Physiotherapists and occupational
therapists worked in a coordinated manner to
facilitate ROM exercise, gait rehabilitation, activities
of daily living maintenance, and early caregiver
training. Basic requirements for discharge included
knee flexion range of 90°, quadriceps muscles
strength of grade 3, and stable walking ability.
All patients were assessed by a nurse in the
clinic at 2 weeks after surgery to evaluate the wound
status and remove staples. They were then evaluated
by surgeons at 1, 3, 6, 12, and 24 months after surgery,
via clinical and radiographic examinations.
Statistical analysis
Data analysis was performed using SPSS (Windows
version 20.0; IBM Corp, Armonk [NY], United States).
Normal distributions of the data were assessed by
the Shapiro–Wilk normality test for each series of measurements. Univariate analysis was performed
using the Chi squared test and unpaired t tests,
respectively, for categorical and numerical data with
normal distributions. Comparisons of parameters
with non-normal distributions were performed
using the Mann–Whitney U test. To adjust for the
confounding effects of multiple variables (eg, type
of anaesthesia, Charlson Comorbidity Index, and
other baseline co-morbidities), multivariate analysis
was performed with multiple logistic regressions.
The high-risk group was defined as Charlson
Comorbidity Index >5, on the basis of previous
findings regarding the risk of complications in
TKA.13 Data were reported as mean ± standard
deviation unless otherwise specified. Statistical
significance was defined as P<0.05. In addition, power
analysis to determine the sample size was performed
using G*Power (version 3.1.9.1),14 assuming that
power >0.80 was indicative of an appropriate sample
size.
Results
Patient characteristics
In total, 1788 patients underwent primary TKA
during the study period (Table 1). Of these patients,
112 (6.3%) were aged >80 years (octogenarian
group; mean age, 82.7 ± 1.6 years; range, 81-89);
80 patients (71.4%) in the octogenarian group were
women. From the remaining patients, 108 sex- and
BMI-matched patients aged ≤80 years (mean age,
66.4 ± 8.7 years; range, 43-80) were selected at
random and assigned to the control group (ie, non-octogenarian
group). The mean follow-up interval
for all patients was 3.2 years (range, 2-5 years).
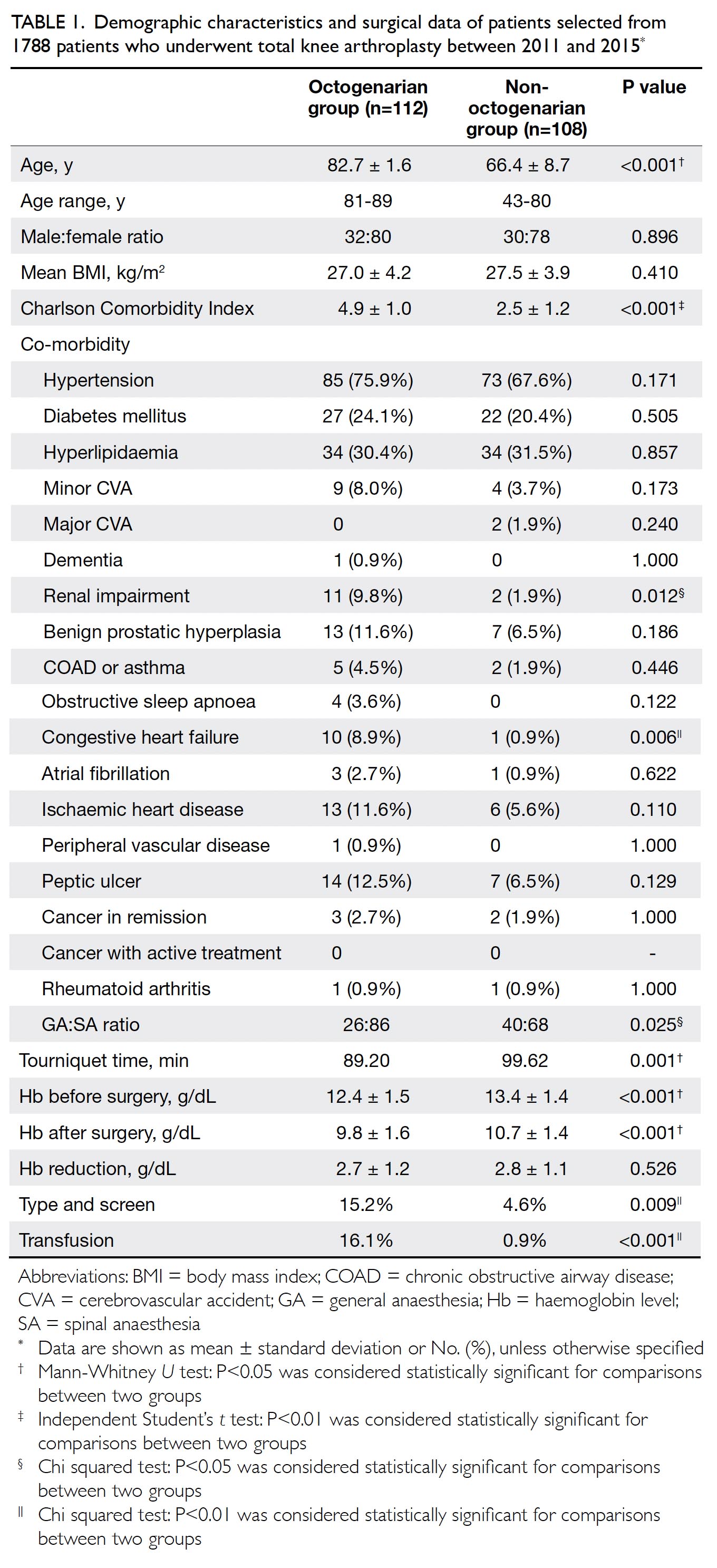
Table 1. Demographic characteristics and surgical data of patients selected from 1788 patients who underwent total knee arthroplasty between 2011 and 2015
The indication for TKA in most patients
(218 patients, 99.1%) was primary osteoarthritis of
the knee joint. Two patients (0.9%) had rheumatoid
arthritis of the knee joint. There was no significant
difference between groups in the number of patients
with rheumatoid arthritis. The octogenarian group
had a significantly higher Charlson Comorbidity
Index (4.9 ± 1.0 vs 2.5 ± 1.2, P<0.001), along with
higher incidences of renal impairment and congestive
heart failure.
More cases were performed with spinal
anaesthesia in both groups. The ratio of general to
spinal anaesthesia was lower in the octogenarian
group (26:86 vs 40:68, P=0.025). Tourniquet time was
significantly lower in the octogenarian group than
in the non-octogenarian group (89.20 ± 17.25 mins
vs 99.62 ± 23.94 min, P=0.001). Preoperative
and postoperative haemoglobin levels were both
significantly lower in the octogenarian group. Both
groups exhibited similar degrees of reduction in
haemoglobin levels. More blood transfusions were
recorded in the octogenarian group (16.1% vs 0.9%,
P<0.001).
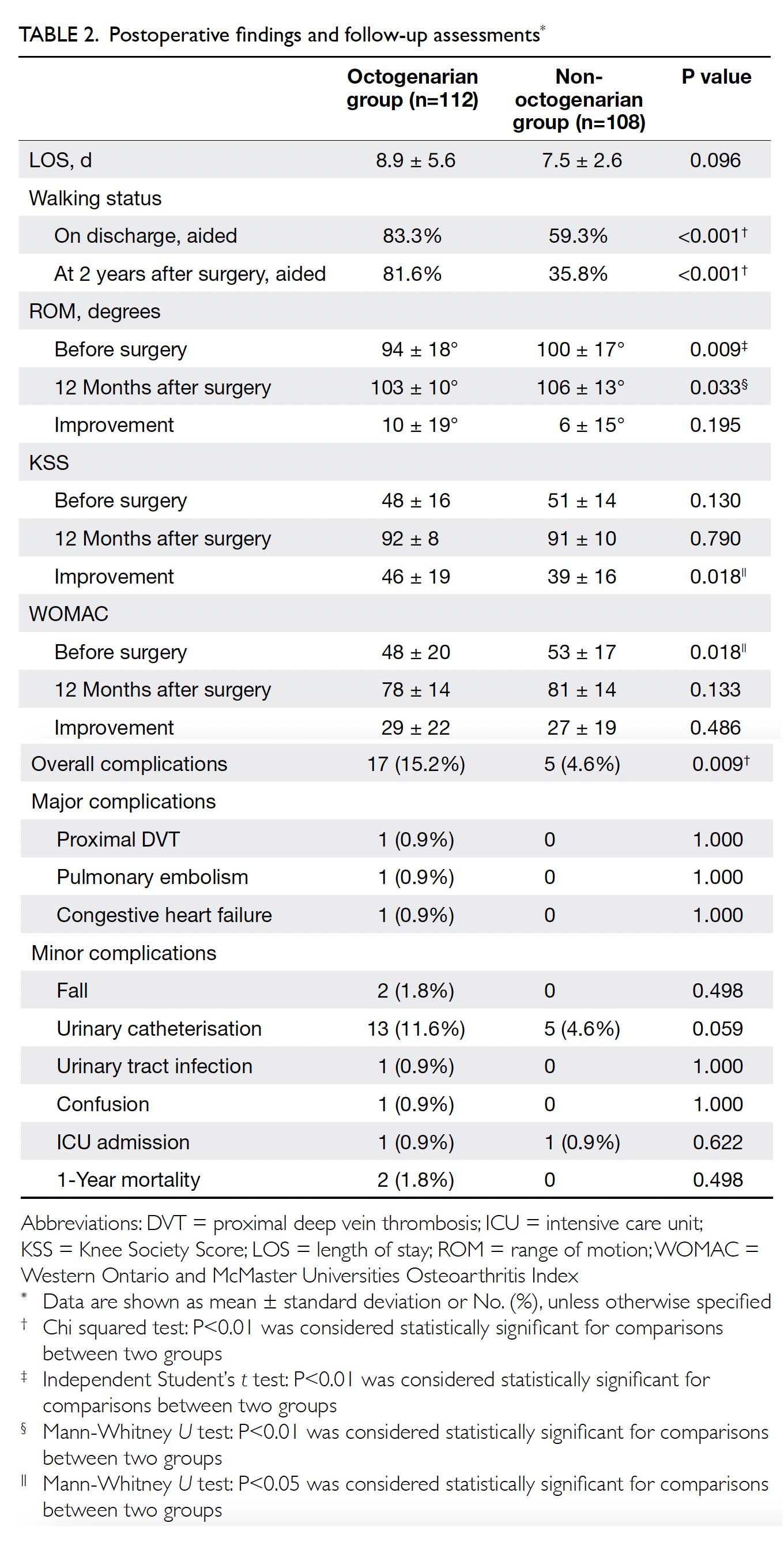
Length of stay and changes in functional
outcomes
The length of stay did not significantly differ between groups (octogenarian: 8.9 ± 5.6 d vs non-octogenarian:
7.5 ± 2.6 d, P=0.096) [Table 2].
Significantly more patients in the octogenarian
group required a walking aid upon discharge (83.3%
vs 59.3%, P<0.001). At 2 years after surgery, more
patients in the octogenarian group continued to
require a walking aid (81.6% vs 35.8%, P<0.001).
The octogenarian group exhibited a worse
preoperative ROM (94 ± 18° vs 100 ± 17°, P=0.009)
and WOMAC score (48 ± 20 vs 53 ± 17, P=0.018), but
the improvements in these outcomes at 12 months
after surgery were identical in both groups. In
contrast, greater improvement in KSS was observed
in the octogenarian group at 12 months after surgery
(46 ± 19 vs 39 ± 16, P=0.018), despite a similar
preoperative score. Importantly, our sample size of
112 octogenarian patients and 108 non-octogenarian
patients exhibited 83.7% power to detect a difference
in the primary outcome of KSS improvement after
surgery between groups when such a difference was
present.
Complications and mortality
The incidence of major complications tended to be
greater in the octogenarian group, although this
difference was not statistically significant (2.7%
vs 0%, P=0.087) [Table 2]. The incidence of overall
complications was significantly higher in the
octogenarian group (15.2% vs 4.6%, P=0.009). Despite
the higher preoperative Charlson Comorbidity Index
in the octogenarian group, there were no significant
differences in the individual incidences of falls,
urinary tract infection, proximal DVT, pulmonary
embolism, confusion, and congestive heart failure, or
in the rates of ICU admission and 1-year mortality.
Notably, urinary catheterisation tended to occur
more frequently in the octogenarian group, although
this difference was not statistically significant (11.6%
vs 4.6%, P=0.059).
Logistic regression was performed to ascertain
the effects of octogenarian status, Charlson
Comorbidity Index >5, anaesthesia type, tourniquet
time, preoperative ROM, and histories of multiple
conditions (ie, renal impairment, congestive
heart failure, major cerebrovascular accident,
ischaemic heart disease, and peptic ulcer disease)
on the likelihood that patients would experience
complications after fast-track TKA. The model
explained 26.7% (Nagelkerke R2) of the variance
in complications and correctly classified 90.0% of
patients. Patients with Charlson Comorbidity Index
>5 were 5.69-fold more likely to exhibit complications
than were patients with a Charlson Comorbidity
Index ≤5 (P=0.039; odds ratio [OR]=5.69; 95% confidence interval [CI]=1.09-32.60). A history of
major cerebrovascular accident (P=0.016; OR=45.03;
95% CI=2.05-991.54) and a history of peptic ulcer
disease (P=0.007; OR=5.51; 95% CI=1.58-19.17)
were also significantly associated with an increased
likelihood of exhibiting complications (Table 3).
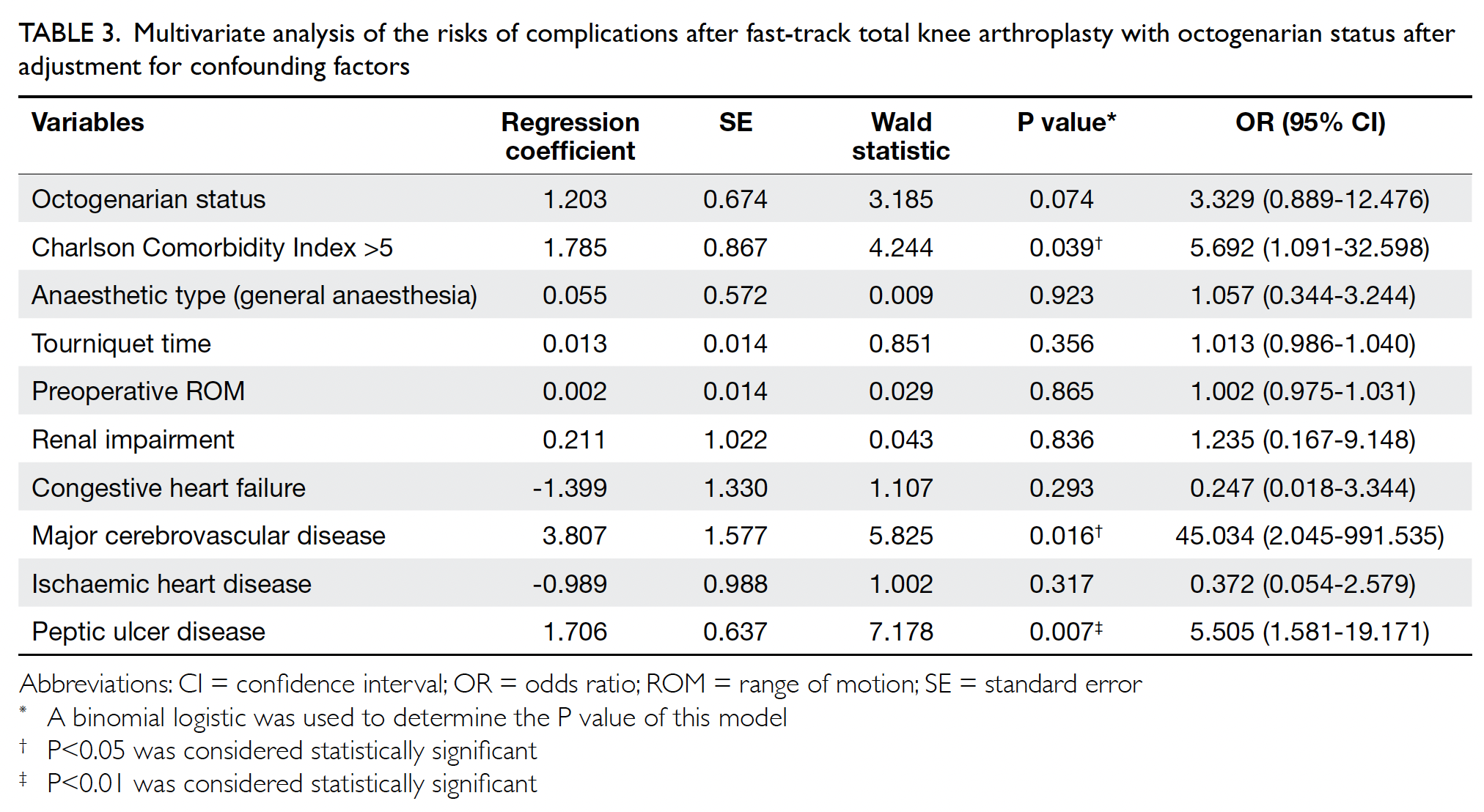
Table 3. Multivariate analysis of the risks of complications after fast-track total knee arthroplasty with octogenarian status after adjustment for confounding factors
Discussion
To our knowledge, this is the first study in Hong
Kong concerning the clinical outcomes of fast-track
TKA for patients aged >80 years. We found higher
incidences of preoperative co-morbidities, anaemia,
postoperative transfusion, and postoperative
complications. Importantly, the improvements
in functional outcomes at 1 year after fast-track
TKA among octogenarians were comparable with
or better than the improvements among younger
patients. Our findings support the use of fast-track
TKA in this older group of patients; they
indicate small and acceptable increases in the risks
for such patients. This study focused on patient
outcomes in our centre from 2011 to 2015. Because
of protocol improvements in subsequent years,
including opioid-sparing analgesia, local infiltrative
anaesthesia, the use of oral tranexamic acid, and
1 year of physiotherapy, the length of stay and the
patient outcomes are expected to improve.
Haemoglobin reduction and blood product
management
In this study, the octogenarian group exhibited a
lower preoperative haemoglobin level. The higher
incidence of anaemia among octogenarians in
the general population may be related to ageing,
particularly because of reduced erythropoietin
production, as well as anaemia secondary to iron,
nutritional deficiency, or chronic disease.14 These
factors presumably contributed to the significant
increases in the rates of transfusion and ‘type and
screen’ in the octogenarian group, despite a similar
haemoglobin reduction and the use of 8 g/dL
as the transfusion threshold in both groups.15
Because perioperative anaemia and allogenic blood
transfusion have been associated with an increased
risk of postoperative infection, longer hospital
stay, and greater mortality,16 iron supplements
and autologous transfusion were used to increase
the preoperative haemoglobin level and reduce
the postoperative transfusion rate. Our fast-track
protocol-driven blood management with a single
transfusion threshold provides a good balance
between adequate treatment of perioperative
anaemia and unnecessary blood transfusion. This
balance was reflected by the absence of significant
increases in periprosthetic infection and mortality in
the octogenarian group.
Length of stay
The length of stay tended to be greater in the
octogenarian group in the present study. Maiorano
et al17 suggested that the mean length of stay was
shorter in patients with a higher modified Barthel
Index Score; better functional status may lead to
more rapid rehabilitation progress. Furthermore, we observed a better preoperative WOMAC score
in younger patients (53 ± 17 vs 48 ± 20, P<0.05),
consistent with the findings by Maiorano et al.17 A
phenomenon unique to Hong Kong is the confined
living area in most homes, which may increase the
difficulty in using a walking aid at home. In the present
study, 83.3% of patients in the octogenarian group
required a walking aid upon discharge. Additionally,
temporary residential service was required more
frequently upon discharge; this arrangement might
have contributed to the increased length of stay.
However, prior anticipation of discharge difficulty
and the multidisciplinary approach in our fast-track
TKA protocol helped to limit the length of
stay, leading to an increase of only 1.4 days in the
octogenarian group.
Functional outcomes
In this study, both groups had comparable outcomes
at 12 months after surgery in terms of improvements
in ROM and WOMAC score. The octogenarian
group exhibited greater improvement in KSS at
12 months after surgery. These results support the
use of TKA among octogenarian patients. Good
functional outcomes without pain are important for
ensuring that patients maintain independence in the
activities of daily living. Such independence relieves
the caretaker burden and helps patients return to the
community.
Mortality and complication rate
In this analysis of fast-track TKA, there was no significant difference between octogenarian and
non-octogenarian groups in terms of the 1-year mortality rate, although the octogenarian group had
a higher Charlson Comorbidity Index. Notably, the
all-cause mortality rate within 1 year after surgery
was 1.79% in the octogenarian group; this was lower
than the annual all-cause mortality rates for the
Hong Kong general population in 2013 among men
and women aged 80 to 84 years (6.1% and 3.7%18,
respectively). In the fast-track protocol, all patients
were assessed by an anaesthetist, an orthopaedic
surgeon, and an orthopaedic nurse. Patients with
suboptimally controlled medical condition were
rapidly referred for out-patient treatment by the
appropriate department. For instance, fast-track
echocardiography was arranged for patients with
suspected valvular problems; fast-track management
of poorly controlled hypertension was performed by
family medicine specialists.
Significantly more patients in the octogenarian
group developed complications. Most patients
exhibited minor complication. There were no
significant differences between groups in terms
of major complications (eg, proximal DVT,
pulmonary embolism, and congestive heart failure).
Furthermore, postoperative confusion was rare, in
contrast to the incidence rate of 6.7% reported by
Kuo et al.19 Postoperative maintenance of good pain
control and normal cognitive status is crucial for
rehabilitation and ensuring safety.20 A multimodel
analgesic regimen in the 4 days after surgery was
implemented in our centre to achieve the greatest
degree of analgesia with the fewest side-effects. Each
patient was provided patient-controlled analgesia
comprising morphine infusion, paracetamol, and
nonsteroidal anti-inflammatory drugs.
After adjustment for confounding factors, patients with Charlson Comorbidity Index >5 were
5.69-fold more likely to develop postoperative
complications. The Charlson Comorbidity Index has
been widely used in large studies to predict functional
outcome, implant survival, mortality, and length
of stay after TKA.21 22 Our results were consistent
with the findings by Marya et al13 that a Charlson
Comorbidity Index of >5 was associated with major
complications after bilateral simultaneous TKA. In
addition, we found that patients with past histories
of major cerebrovascular accident and peptic ulcer
disease were more likely to have postoperative
complications. Previous stroke has been identified as
a predictive factor for perioperative acute ischaemic
stroke after TKA,23 whereas peptic ulcer disease has
been associated with periprosthetic fracture after
primary TKA.24 After adjustment for confounding
factors, we found that octogenarian status alone
was not associated with significantly greater risk of
complications after fast-track TKA. Surgeons should
consider patient risk during TKA on the basis of their
individual co-morbidities, rather than age alone.
Urinary catheterisation
There was a considerably higher incidence of urinary
catheterisation in the octogenarian group. Lingaraj
et al25 suggested that 8% of all patients undergoing
TKA develop urinary retention. There is a need to
identify postoperative urinary retention to reduce
the risks of periprosthetic joint infection and renal
impairment. As part of our fast-track protocol, a
protocol-driven management approach was used
for each patient with acute urine retention. Bladder
scans were performed by nurses to assess post-micturition
volume; catheterisation was performed
in patients with any bladder distention. Stimulant
laxative treatment was used to avoid constipation
and alleviate urine retention.
Limitations
There were some limitations in this study. First,
the study was small and the follow-up period was
short (mean, 3.2 years). However, there are generally
few patients aged >80 years who have sufficient
life expectancy for a longer period of follow-up.
Second, this was a retrospective cohort study, with
the inherent limitations of the retrospective design.
Although a prospective randomised controlled trial
is preferable, ethical considerations prohibit the
allocation of octogenarian patients to a non-fast-track
protocol because of their higher operative
risks. Third, although coronal plane deformity and
the degree of soft tissue balance may contribute to
differences in knee functional performance, these
parameters were not measured. Future studies should
include such assessments to more fully characterise
the factors that influence TKA outcomes.
Conclusion
Compared with non-octogenarians, octogenarians
had greater improvement in KSS at 1 year after
fast-track TKA, despite similar preoperative
KSS. Octogenarians had a higher incidence of
complications after TKA. After adjustment for
confounding factors, we found that Charlson
Comorbidity Index >5, history of major
cerebrovascular accident, and history of peptic ulcer
disease were predictive of complications after fasttrack
TKA; importantly, octogenarian status was not
predictive of complications. There were no significant
differences in the length of hospitalisation, incidence
of major complications, rate of ICU admission, or the
1-year mortality rate between the octogenarian and
non-octogenarian groups. Thus, age alone should
not be a contra-indication to TKA.
Author contributions
Concept or design: All authors.
Acquisition of data: CH Lee, EWY Chang.
Analysis or interpretation of data: CH Lee, EWY Chang.
Drafting of the manuscript: TP Leung, CH Lee, QJ Lee.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: CH Lee, EWY Chang.
Analysis or interpretation of data: CH Lee, EWY Chang.
Drafting of the manuscript: TP Leung, CH Lee, QJ Lee.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was approved by the Kowloon West Cluster Research Ethics Committee (Ref: KW/EX-20-068(147-03)).
References
1. Census and Statistics Department, Hong Kong SAR
Government. Hong Kong Population Projection 2012-2041. Available from: https://www.censtatd.gov.hk/media_workers_corner/pc_rm/hong_kong_population_projections_2012_2041/index.jsp. Accessed 31 Jul 2012.
2. Yuen W. Osteoarthritis of knees: the disease burden in
Hong Kong and means to alleviate it. Hong Kong Med J
2014;20:5-6. Crossref
3. Kreder HJ, Berry GK, Mcmurtry IA, Halman SI. Arthroplasty in the octogenarian: quantifying the risks. J
Arthroplasty 2005;20:289-93. Crossref
4. Jämsen E, Puolakka T, Eskelinen A, et al. Predictors of
mortality following primary hip and knee replacement in
the aged. A single-center analysis of 1998 primary hip and
knee replacements for primary osteoarthritis. Acta Orthop
2012;84:44-53. Crossref
5. Scott JE, Mathias JL, Kneebone AC. Postoperative cognitive dysfunction after total joint arthroplasty in the elderly: a meta-analysis. J Arthroplasty 2014;29:261-7.e1. Crossref
6. Mnatzaganian G, Ryan P, Norman PE, Davidson DC, Hiller JE. Total joint replacement in men: old age, obesity
and in-hospital complications. ANZ J Surg 2012;83:376-81. Crossref
7. Klasan A, Putnis SE, Yeo WW, Fritsch BA, Coolican MR,
Parker DA. Advanced age is not a barrier to total
knee arthroplasty: a detailed analysis of outcomes and
complications in an elderly cohort compared with average
age total knee arthroplasty patients. J Arthroplasty
2019;34:1938-45. Crossref
8. Petruccelli D, Rahman WA, de Beer J, Winemaker M.
Clinical outcomes of primary total joint arthroplasty among
nonagenarian patients. J Arthroplasty 2012;27:1599-603. Crossref
9. Shah AK, Celestin J, Parks ML, Levy RN. Long-term results
of total joint arthroplasty in elderly patients who are frail.
Clin Orthop Relat Res 2004;425:106-9. Crossref
10. Hernández-Vaquero D, Fernández-Carreira JM, Pérez-Hernández D, Fernández-Lombardía J, García-Sandoval
MA. Total knee arthroplasty in the elderly. Is there an age
limit? J Arthroplasty 2006;21:358-61.
11. Joshi AB, Markovic L, Gill G. Knee arthroplasty in octogenarians: results at 10 years. J Arthroplasty
2003;18:295-8. Crossref
12. Berend ME, Thong AE, Faris GW, Newbern G, Pierson JL,
Ritter MA. Total joint arthroplasty in the extremely elderly:
hip and knee arthroplasty after entering the 89th year of
life. J Arthroplasty 2003;18:817-21. Crossref
13. Marya SK, Amit P, Singh C. Impact of Charlson indices
and comorbid conditions on complication risk in bilateral
simultaneous total knee arthroplasty. Knee 2016;23:955-9. Crossref
14. Partridge J, Harari D, Gossage J, Dhesi J. Anaemia in the
older surgical patient: a review of prevalence, causes,
implications and management. J R Soc Med 2013;106:269-77. Crossref
15. Lee QJ, Mak WP, Yeung ST, Wong YC, Wai YL. Blood management protocol for total knee arthroplasty to reduce blood wastage and unnecessary transfusion. J Orthop Surg
(Hong Kong) 2015;23:66-70. Crossref
16. Spahn DR. Anemia and patient blood management in hip and knee surgery: a systematic review of the literature.
Anesthesiology 2010;113:482-95. Crossref
17. Maiorano E, Bodini BD, Cavaiani F, Pelosi C, Sansone V. Length of stay and short-term functional outcomes
after total knee arthroplasty: can we predict them? Knee
2017;24:116-20. Crossref
18. Census and Statistics Department, Hong Kong SAR Government. Hong Kong Monthly Digest of Statistics
November 2014. The mortality trend in Hong Kong, 1981
to 2013. Available from: https://www.statistics.gov.hk/pub/B71411FB2014XXXXB0100.pdf. Accessed 17 Nov 2014.
19. Kuo FC, Hsu CH, Chen WS, Wang JW. Total knee arthroplasty in carefully selected patients aged 80 years or
older. J Orthop Surg Res 2014;9:61. Crossref
20. Lynch EP, Lazor MA, Gellis JE, Orav J, Goldman L, Marcantonio ER. The impact of postoperative pain on
the development of postoperative delirium. Anesth Analg
1998;86:781-5. Crossref
21. Kreder HJ, Grosso P, Williams JI, et al. Provider volume and other predictors of outcome after total knee arthroplasty: a population study in Ontario. Can J Surg 2003;46:15-22.
22. Bjorgul K, Novicoff WM, Saleh KJ. Evaluating comorbidities in total hip and knee arthroplasty: available instruments. J Orthop Traumatol 2010;11:203-9. Crossref
23. Menendez ME, Greber EM, Schumacher CS, Lowry Barnes C. Predictors of acute ischemic stroke after total
knee arthroplasty. J Surg Orthop Adv 2017;26:148-53. Crossref
24. Singh JA, Lewallen DG. Association of peptic ulcer disease
and pulmonary disease with risk of periprosthetic fracture
after primary total knee arthroplasty. Arthritis Care Res
(Hoboken) 2011;63:1471-6. Crossref
25. Lingaraj K, Ruben M, Chan YH, Das SD. Identification
of risk factors for urinary retention following total knee
arthroplasty: a Singapore hospital experience. Singapore
Med J 2007;48:213-6.