Hong Kong Med J 2022 Feb;28(1):64–72 | Epub 28 Jan 2021
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
MEDICAL PRACTICE
Admission triage tool for adult intensive care unit
admission in Hong Kong during the COVID-19 outbreak
Gavin M Joynt, MBBCh, FHKAM (Anaesthesiology)1; Anne KH Leung, MB, ChB, FHKAM (Anaesthesiology)2; CM Ho, MB, ChB, FHKAM (Medicine)3; Dominic So, MB, BS, FHKAM (Anaesthesiology)4; HP Shum, MB, BS, MD5; FL Chow, MB, BS, FHKAM (Medicine)6; Alwin WT Yeung, MB, BS, FHKAM (Medicine)7; KL Lee, MB, ChB, FHKAM (Medicine)8; Gloria KY Tang, MB, BS, FHKAM (Medicine)9; WW Yan, MB, BS, FHKAM (Medicine)5; for the Triage Working Group of the Co-ordinating Committee (Intensive Care)
1 Department of Anaesthesia and Intensive Care, The Chinese University of Hong Kong, Hong Kong
2 Department of Intensive Care, Queen Elizabeth Hospital, Hong Kong
3 Department of Intensive Care, Tuen Mun Hospital, Hong Kong
4 Department of Intensive Care, Princess Margaret Hospital, Hong Kong
5 Department of Intensive Care, Pamela Youde Nethersole Eastern Hospital, Hong Kong
6 Department of Intensive Care, Caritas Medical Centre, Hong Kong
7 Department of Medicine and Geriatrics, Ruttonjee & Tang Shiu Kin Hospitals, Hong Kong
8 Department of Intensive Care, United Christian Hospital, Hong Kong
9 Department of Adult Intensive Care, Queen Mary Hospital, Hong Kong
Corresponding author: Prof Gavin M Joynt (gavinmjoynt@cuhk.edu.hk)
Abstract
Intensive care is expensive, and the numbers of
intensive care unit (ICU) beds and trained specialist
medical staff able to provide services in Hong Kong
are limited. The most recent increase in coronavirus
disease 2019 (COVID-19) infections over July to
August 2020 resulted in more than 100 new cases
per day for a prolonged period. The increased
numbers of critically ill patients requiring ICU
admission posed a capacity challenge to ICUs across
the territory, and it may be reasonably anticipated
that should a substantially larger outbreak occur,
ICU services will be overwhelmed. Therefore,
a transparent and fair prioritisation process for
decisions regarding patient ICU admission is
urgently required. This triage tool is built on the
foundation of the existing guidelines and framework
for admission, discharge, and triage that inform
routine clinical practice in Hospital Authority ICUs,
with the aim of achieving the greatest benefit for
the greatest number of patients from the available
ICU resources. This COVID-19 Crisis Triage Tool
is expected to provide structured guidance to
frontline doctors on how to make triage decisions
should ICU resources become overwhelmed by
patients requiring ICU care, particularly during the
current COVID-19 pandemic. The triage tool takes
the form of a detailed decision aid algorithm based
on a combination of established prognostic scores,
and it should increase objectivity and transparency
in triage decision making and enhance decision-making
consistency between doctors within and across ICUs in Hong Kong. However, it remains an
aid rather than a complete substitute for the carefully
considered judgement of an experienced intensive
care clinician.
Introduction
The most recent wave of coronavirus disease 2019
(COVID-19) infections in July to August 2020
resulted in more than 100 new cases per day in Hong
Kong for a prolonged period. The stress experienced
by individual intensive care units (ICUs) in Hong
Kong was demonstrated by the need for an unusually
large number of patient transfers between units to
maximise the available ICU capacity, despite the
implementation of surge strategies. Admission
decisions to ICUs resulting from the added pressure
for ICU beds, as well as social dimensions that were triggered by the COVID-19 outbreak, resulted
in an urgent requirement for contingencies to
inform admission triage practices in the face of
overwhelming ICU demand. Professional bodies
have recommended that triage protocols (clinical
decision support systems), rather than clinical
judgement alone, be used in triage whenever
possible,1 and that such protocols be available to
assist frontline doctors.1 2 Such protocols should be
locally relevant and prepared in advance of the need
for implementation.
This document is built on the existing Admission, Discharge, and Triage Guidelines
that inform routine clinical practice in Hospital
Authority ICUs. The purpose of this COVID-19
Crisis Triage Tool is to provide structured guidance
to frontline clinicians to assist with triage decision
making should ICU resources become overwhelmed
by patients requiring ICU care in Hong Kong.
Background
The Admission, Discharge, and Triage Guidelines
for Adult Intensive Care Services for use in day-to-day ICU operations in Hong Kong were recently
updated in an internal operations circular in 2018. A
brief summary of this guideline follows. Hong Kong
ICUs provide a high standard of intensive care by
international benchmarks.3 However, because of the
expensive nature of intensive care resources, there
are a limited number of ICU beds available in Hong
Kong. Hong Kong has approximately 7.1 critical care
beds per 100 000 population, a low number compared
with other high-income regions in Asia (Singapore:
11.4/100 000, Taiwan: 29/100 000), North America
(Canada: 12/100 000, United States: 20/100 000),
and Europe (Germany: 25/100 000, Belgium:
20/100 000).4 5 Therefore, ICU beds in Hong Kong
are generally reserved for patients with reversible
medical conditions who have reasonable prospects
of substantial recovery, and triage (prioritisation)
decisions are routinely necessary.6 7 The existing
admission and triage guidelines are designed to help
optimise the use of ICU services to achieve the largest possible benefit for the most patients within available
resources, a modified utilitarian ethical approach
that is recommended by ICU professional bodies
internationally.8 9 10 Briefly, patients who require ICU
care are referred to the ICU team for admission
screening. All ICU admission triage decisions are
supervised by a senior, experienced ICU doctor and
implemented according to individual unit policy. In
principle, all triage decisions should be based on the
patient’s medical condition and the benefits likely
to be derived from ICU admission (in comparison
with a lower level of care). Non-medical factors such
as gender, race, religion, education level, and social
status should not be considered when making triage
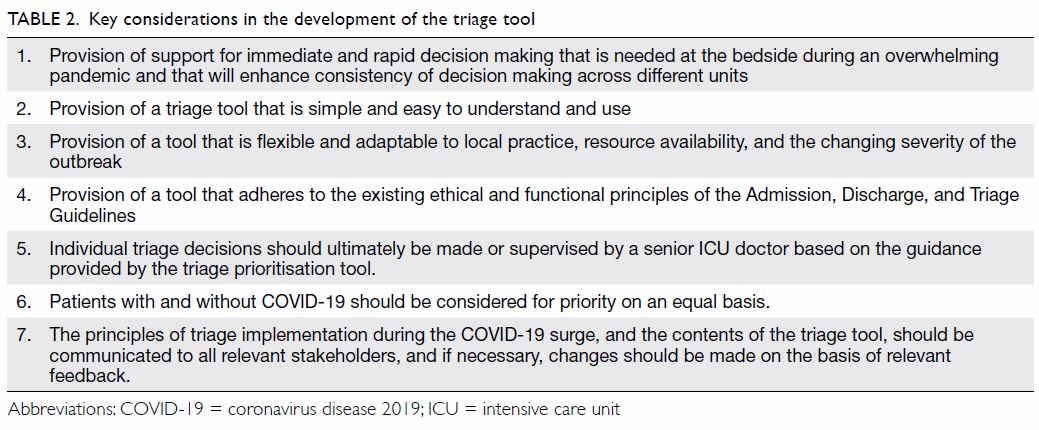
decisions. The existing broad-based framework
that guides individual unit policy (Fig 1) was used
to inform the relevant components of the new
COVID-19 Crisis Triage Tool.
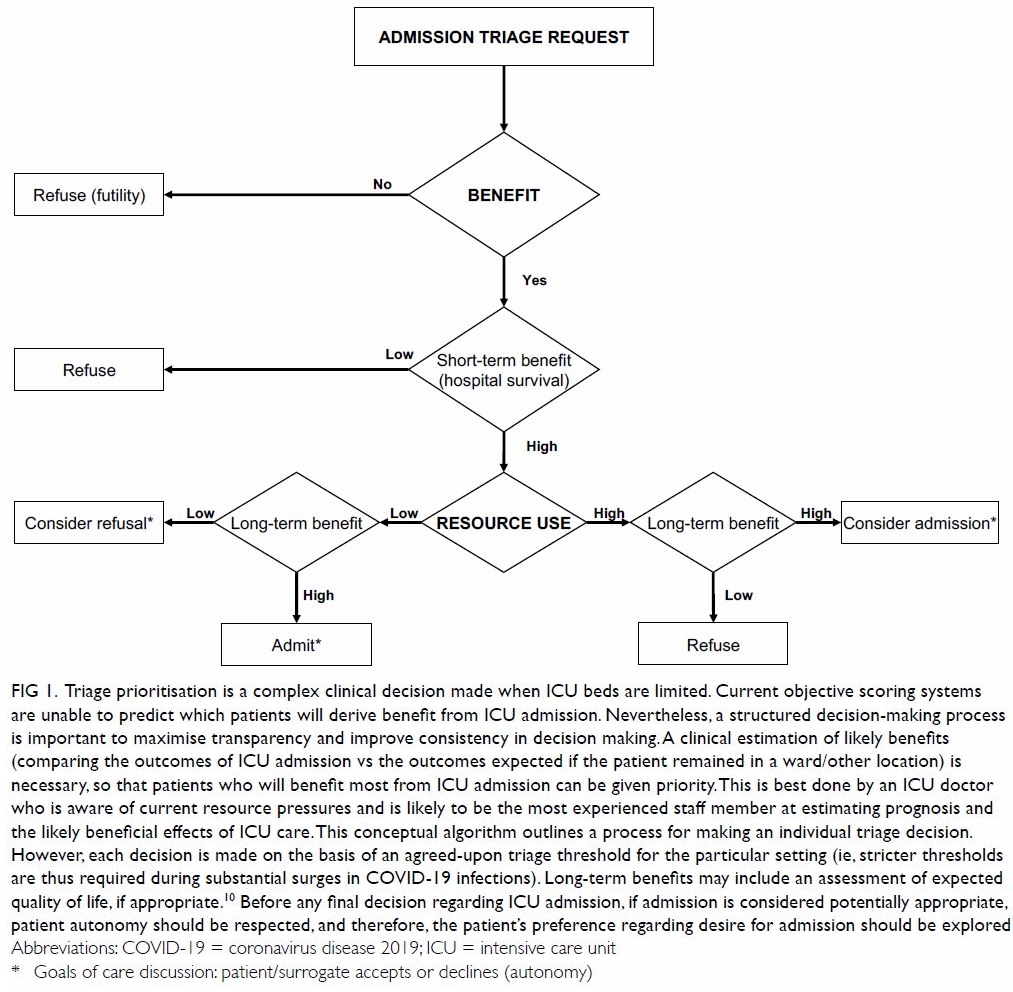
Figure 1. Triage prioritisation is a complex clinical decision made when ICU beds are limited. Current objective scoring systems are unable to predict which patients will derive benefit from ICU admission. Nevertheless, a structured decision-making process is important to maximise transparency and improve consistency in decision making. A clinical estimation of likely benefits (comparing the outcomes of ICU admission vs the outcomes expected if the patient remained in a ward/other location) is necessary, so that patients who will benefit most from ICU admission can be given priority. This is best done by an ICU doctor who is aware of current resource pressures and is likely to be the most experienced staff member at estimating prognosis and the likely beneficial effects of ICU care. This conceptual algorithm outlines a process for making an individual triage decision. However, each decision is made on the basis of an agreed-upon triage threshold for the particular setting (ie, stricter thresholds are thus required during substantial surges in COVID-19 infections). Long-term benefits may include an assessment of expected quality of life, if appropriate.10 Before any final decision regarding ICU admission, if admission is considered potentially appropriate, patient autonomy should be respected, and therefore, the patient’s preference regarding desire for admission should be explored
Maximising existing intensive care
unit capabilities in response to a
surge of COVID-19 cases
Prioritisation for ICU admission in the form of
admission triage can only be justified once all
efforts to maximise available resources have been
exhausted. The Hospital Authority’s existing
infectious disease contingency plan dictates that
the number of available ICU beds be increased and
is based on certain key principles: first, that the
standard of intensive care should be maintained at a
standard similar to that usually provided by Hospital
Authority ICUs, and second, that infection control
procedures that provide a high level of protection
against staff cross-infection with severe acute
respiratory syndrome coronavirus 2 (SARS-CoV-2)
should be maintained. Maintaining these standards
requires the provision of appropriately trained staff
in adequate numbers. Failure to adhere to these
principles may have devastating consequences, as
occurred during the SARS outbreak in 2003.11 The
requirement to maintain these standards necessarily
results in a relatively limited surge capacity12 that may
be incapable of meeting all the demands of a large
COVID-19 transmission surge in the community.
Thus, the overall increase (68 beds) in ICU airborne
infection isolation room beds from Stage I (48 beds)
to Stage III (116 beds) will likely be insufficient.
The Hong Kong Government has plans to
construct a number of temporary community
hospitals for a potentially large surge. However, this
initiative does not include a provision for ICU beds,
and independent preparations will be required to
maximise ICU capacity. In the event that individual
hospitals need to increase ICU capacity beyond that
specified by the existing Contingency Plan Stage III
provisions, a number of key principles should be
adopted (Table 1).
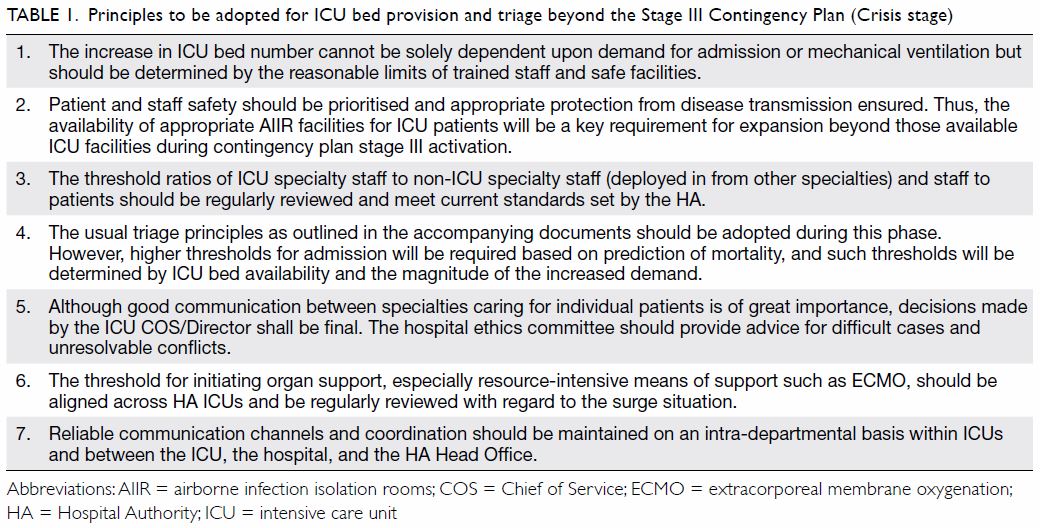
Table 1. Principles to be adopted for ICU bed provision and triage beyond the Stage III Contingency Plan (Crisis stage)
Methods
Despite some previous attempts, no single objective,
evidence-based triage tool in the form of a score or
combination of scores has been shown to effectively
determine appropriate ICU admission priority.13 14 15
Development of a guidance tool was thus initiated
using an iterative process in which possible
combinations of predictive scoring components
were progressively evaluated for face validity by
experienced intensive care specialists. The local
development of this triage tool to accompany the
Admission, Discharge, and Triage Guidelines for
Hong Kong (outlined above) was led by 10 senior ICU
clinical specialists who are currently practising in
ICUs in Hong Kong. The participants included at least
one representative of each of Hong Kong’s hospital
cluster regions. Additionally, each participant
routinely performs triage as a consequence of chronic
ICU bed resource limitations. An initial meeting was
held online, at which all key issues were discussed,
and a draft document of the consensus view
prepared by one author (GMJ). After circulation,
several disagreements were documented. These were
resolved by online voting, with a majority vote used
to resolve persistent disagreement. Three rounds of
online voting resulted in a finalised and universally
supported document. A decision was made to
respect and use the principles laid down in the
pre-existing triage framework but to provide further
detailed clinical guidance to frontline ICU doctors
in Hong Kong regarding COVID-19. The starting
point was to adapt and modify a recently published
COVID-19 triage prioritisation tool developed by an
international expert group.14 This tool took the form
of a decision-making algorithm based on established
ICU prognostic scoring systems that could inform
bedside decision making in the event that ICU bed
capacity becomes overwhelmed by patients with
COVID-19. Therefore, the specific aim of the triage
tool is to provide explicit and uniform guidance to all frontline doctors charged with the responsibility
of triaging ICU admissions. This guidance should
improve the objectivity and consistency of triage
decision making across Hong Kong. The
triage tool was designed to be easily understood,
rapidly implemented, and of high utility. A list of the
major considerations addressed to achieve this goal
is provided in Table 2.
Results
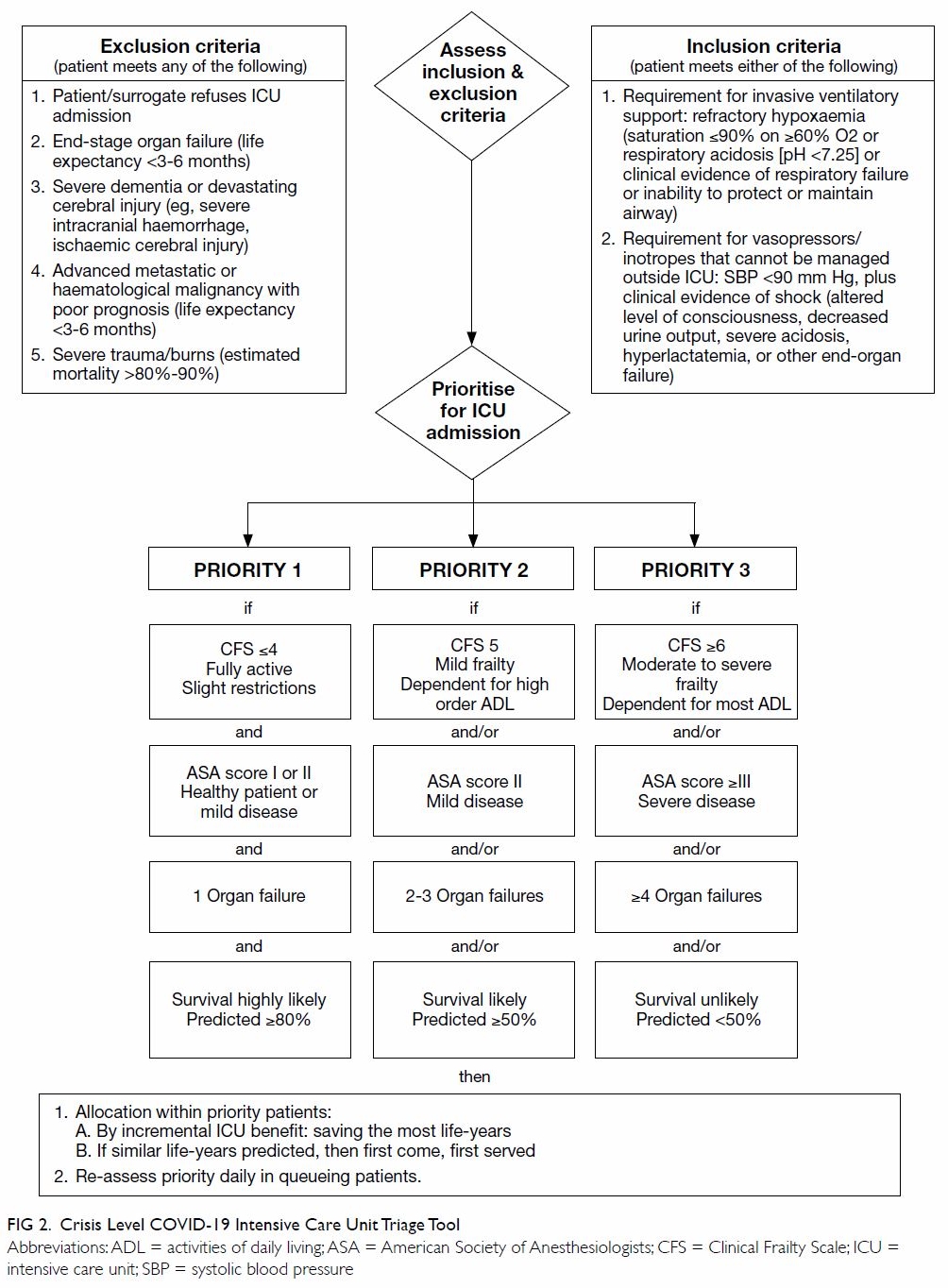
The first inclusion and exclusion criteria chosen for
the triage tool (Fig 2) were those that, when answered,
would rapidly finalise the decision without the need
to proceed further, and thus prevent excessive use of
valuable medical team time. Therefore, we created
clear clinical exclusion criteria. Patients who are too
ill to gain substantial incremental benefits from ICU
care and those who refuse ICU admission on the
basis of the perceived benefits and burdens of ICU
care are excluded.
The explicit exclusion criteria are the same
ones generally used in Hong Kong ICUs under
normal circumstances. We chose general rather than
specific diagnoses, as has been proposed previously,
as specific diagnoses require the construction of
long (but not exhaustive) lists.
The inclusion criteria are also directly
comparable with the major inclusion criteria for ICU
admission during ‘normal’ conditions: they reflect
the need to admit patients who require ICU care to
derive a survival benefit. Thus, patients who are ‘too
well’ (ie, they can be reasonably treated in the ward)
are excluded.
When a patient meets the inclusion criteria
and does not meet any exclusion criteria, they
become a potential ICU admission, and further
priority is determined. Patients are subsequently
chosen for admission based on their priority
rank, ranging from 1—high priority to 3—low
priority. A prioritisation score was developed by including variables that predict short–medium-term
mortality (3-6 months) in the first instance
and are the most compatible with the principle of
‘quick and clear’ decision making. The clinical frailty
scale (CFS) [Fig 3],16 a modified American Society of Anesthesiologists (ASA) score17 to assess co-morbidity
(Table 3), and last, the clinical assessment of
the number of current organ system failures (OSF), that
has previously been well established as an indicator
to assist the prediction of mortality.
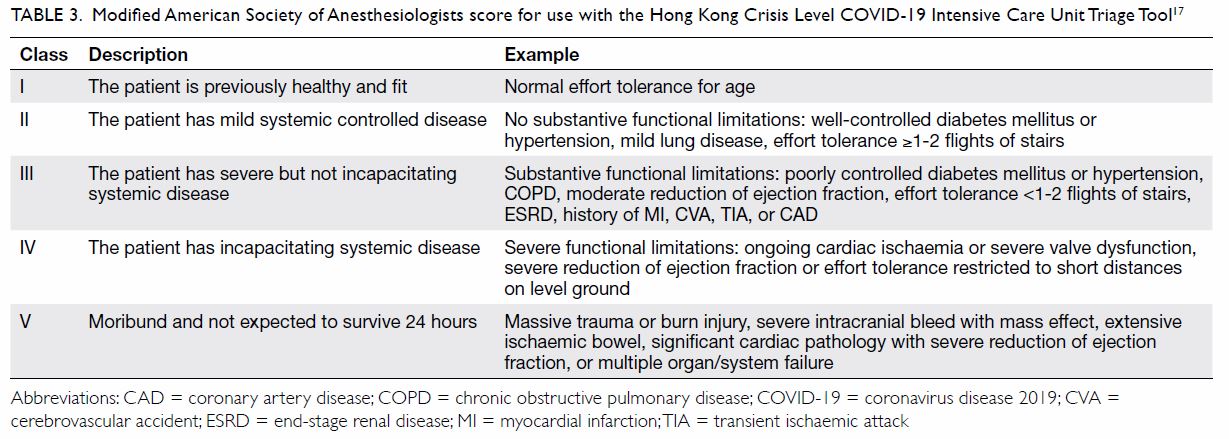
Table 3. Modified American Society of Anesthesiologists score for use with the Hong Kong Crisis Level COVID-19 Intensive Care Unit Triage Tool17
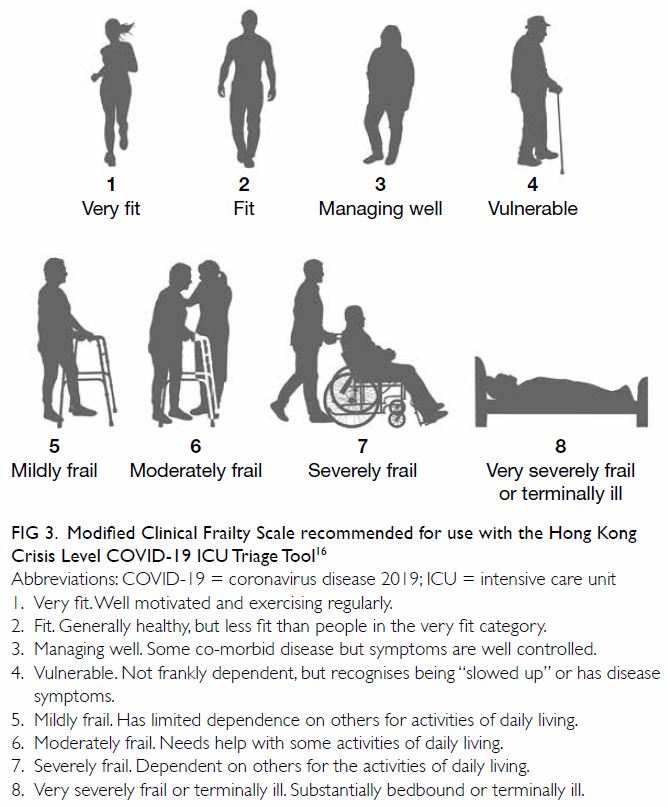
Figure 3. Modified Clinical Frailty Scale recommended for use with the Hong Kong Crisis Level COVID-19 ICU Triage Tool16
Outcome prognostication by the senior
supervising ICU doctor is largely dependent on
knowledge of the factors associated with poor
outcomes and clinical experience. Although key
relevant factors are captured by the tool, because
COVID-19 is a new condition, we provide a table
summarising mortality risk factors in patients with
COVID-19 who are admitted to ICU to further aid prognostication (Table 4).18 19 20 The data were adapted from countries with ICU practices that are
considered generally similar to those in Hong Kong.
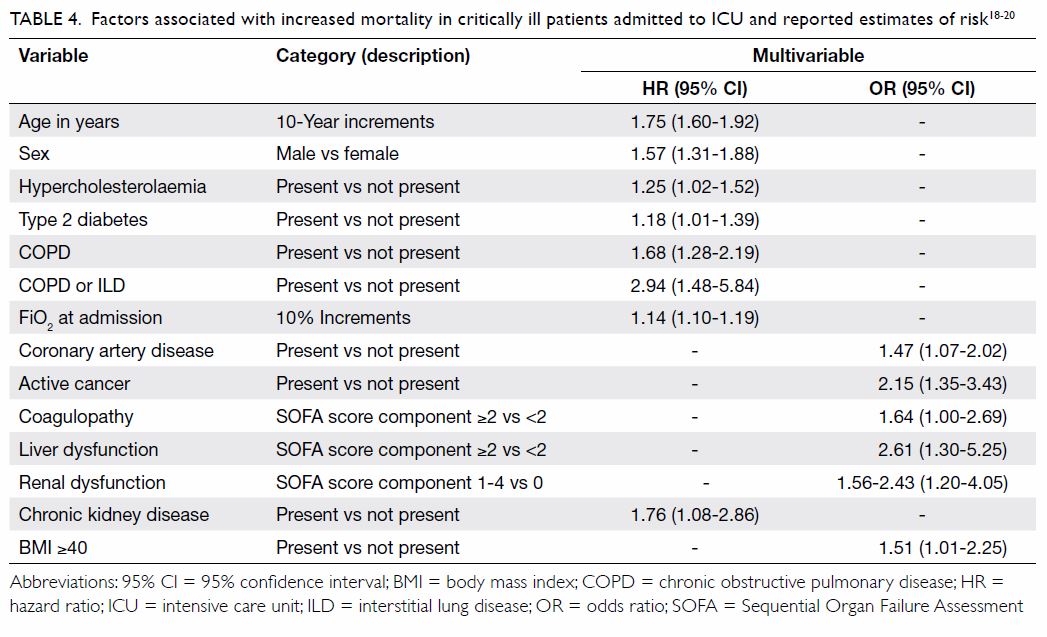
Table 4. Factors associated with increased mortality in critically ill patients admitted to ICU and reported estimates of risk18 19 20
Finally, it has been previously recommended
that time-limited trials may be adopted at the time
of admission.21 A time-limited trial establishes an
agreement between the healthcare team and the
patient/surrogate to apply necessary intensive care
treatment for a pre-determined period of time.
The ICU team keeps the family informed of patient
progress, and when the pre-agreed time limit is
reached, life support therapies are either continued if
the patient has responded positively or withdrawn if
therapy is failing. Setting an appropriate time period
for the trial requires great care,22 and in the setting of
COVID-19, care should be taken to allow sufficient
time for the patient to respond to therapy. The median
number of days of mechanical ventilation and the
length of stay have been reported for patients with
COVID-19 (10 days, and 9 to 12 days, respectively), whose ICU stays are longer than those of patients with other viral pneumonias.18 19
The existing triage framework has been
circulated for comment and feedback from relevant
clinical specialty leadership groups in the Hospital
Authority. Further, the current accompanying tool
has been reviewed by the ad-hoc Hospital Authority
Clinical Ethics Committee Core Group and finalised
after incorporating relevant suggestions for change.
After implementation, the triage working group will
review the need for adjustment and updating of the
guidelines according to local circumstances.
Discussion
The conceptual algorithm recommended herein
broadly follows the existing recommended
framework for individual triage decisions in that
the inclusion criteria are based on a low likelihood
of survival without ICU care (5%-10% or less), if
met. Priorities for admission can then be allocated on the basis of agreed-upon criterion thresholds for
survival, as established in the accompanying triage
tool and adjusted for Hong Kong’s circumstances at a
specific time. Thus, an incremental benefit of at least
40% to 45% would be required to meet the criteria
for priority level 3, but one of at least 70% to 75%
would be required to meet the criteria for priority
level 1. Admission would depend on available
resources after safe maximisation of surge capacity
and the number of patients queuing for admission
(eg, stricter incremental benefit thresholds may
be required during the peak of the pandemic, and
less strict thresholds may be implemented at the
beginning and towards the end). The use of predicted
incremental benefit for decision making has been
previously endorsed by expert consensus groups
when triage is required, both under outbreak and
non-outbreak conditions.1 2 14
The CFS, which has nine variables, was chosen
as the appropriate general health performance
metric, as it meets local practice requirements:
familiarity, ease of use, and having been validated
as a predictor of short- and medium-term ICU
outcomes.23 24 25 26 The well-established ASA score was
chosen for modification to guide assessment of co-morbidities,
as its descriptions are clear, concise,
and logically presented (ASA 2019).17 Further, the
relationship between increasing OSF scores and
higher mortality is well established.27 28 A simple
bedside clinical assessment of organ failure to decide
the number of OSF is recommended, rather than
attempting to determine the SOFA (Sequential Organ
Failure Assessment) score, which requires additional calculations from clinical variables, assessment of
missing variables, and then further prioritisation.29 30
We suggest using a clinical judgement for assessing
end-stage organ failure of the noted organs (eg,
brain, heart, lungs). However, individual units may
choose to use the SOFA score if its calculation is
considered achievable under local circumstances.
After deliberating at length, the group
concluded that the indicative mortalities of the three
chosen variables for determining the priority scores
(general well-being [CFS], co-morbidities [ASA],
and number of OSF) are such that in combination
they are likely to correspond to the subjective
predicted outcomes and survival percentages noted
at the bottom of the notation for each priority score.
The noted predicted survival percentages were
calibrated with the recommendations of previous
consensus expert groups, one who decided to define
‘a minimal acceptable incremental ICU benefit’ in a
resource-limited setting as a 15% to 25% difference
in mortality,10 and the second who adjusted this
difference to be substantially larger (50%) to
account for the increased pressure anticipated in
an outbreak setting.14 The use of the tool to guide
the clinical estimation of likely benefits (outcome of
ICU admission compared with outcome expected if
the patient remained on the ward/other care area)
is necessary for prioritisation of patients who will
benefit most from ICU treatment. Nevertheless,
because individual patients may have overriding
characteristics not captured by the individual or
combined scores, the final decision regarding likely
incremental benefit and subsequent prioritisation should be made by the senior supervising triage doctor.
If there is more than one patient judged to
be within the same priority group, and there is
anticipated queuing for the remaining available
beds, further prioritisation by incremental ICU
benefit, such as saving the most life-years (evaluating
mortality from both acute and chronic disorders)
should be considered. If a tie for ICU admission
candidates remains after these progressive steps, we
recommend that admission be determined by the
first-come, first-served principle.
Because of the complexity of the decision-making
process and the multiple factors that require
careful consideration, final decisions are best made
by an experienced ICU doctor. However, should
uncontrollable circumstances dictate that decisions
need be made by a more junior colleague, the tool
can still provide assistance to guide and enhance
consistent and justifiable decision making. To
prepare for this possibility, preparatory education
should be provided to more junior colleagues
regarding triage decision making to facilitate
appropriate interpretation of this tool.
This tool specifically addresses the triage of
patients for ICU admission. However, when available
ICU resources are overwhelmed, enhanced levels
of care within the ward or available high care areas
should be used for the treatment of cases denied ICU
admission. This could optimise patient outcomes
within the constraints of available alternatives. In this
regard, both invasive and non-invasive mechanical
ventilation is routine practice in the wards and high-care
areas of many hospitals in Hong Kong. This
fact can potentially be harnessed for the treatment
of COVID-19 cases. Patients denied ICU admission
on the basis of triage should be preferentially
considered for diversion to such resources. Hospital-level
coordination and close liaison between hospital
facilities management and those who manage ICU
resources is required to facilitate the appropriate use
of all potentially available resources.31 Although this
tool is designed specifically to guide ICU admission
triage decisions, other users may consider using
the priority assigned by the ICU triage officer to a
refused case to allocate the patient to an appropriate
next level of care.
Many bedside operational factors are part of
the triage process but are not specifically embedded
in this crisis tool. Nevertheless, they are substantially
addressed in the current Admission, Discharge, and
Triage Guidelines, of which the COVID-19 Crisis
Triage Tool is an extension. These include the need
for clear, empathic communication with patients
and surrogates and the implementation of the
appropriate best care plan, including palliation of
symptoms when appropriate, to patients refused ICU
admission. Clear and transparent communication with referring medical teams, mechanisms for
audit and oversight, and channels for feedback and
reassessment are also required.
Important limitations must be acknowledged.
The current guideline is based on the consensus of
experienced Hong Kong clinicians with a history
of performing bedside triage and not high-level,
published medical evidence. Although the prognostic
systems chosen have been well demonstrated
to align with survival prognosis and functional
outcomes, prognostic uncertainty in intensive care
cannot be overcome by a single scoring system. All
prognostic scoring systems, including the CFS,32 have
limitations, and for this reason, the simultaneous use
of multiple scoring methods, as used in this tool, has
been recommended.15
Conclusion
The referral of a patient for ICU care triggers a
complex triage (prioritisation) decision that must
be made when ICU beds are limited. It is expected
that this triage tool, in the form of a detailed decision
aid algorithm, should increase objectivity and
transparency in triage decision making and help to
enhance consistency between doctors both within
and across ICUs in Hong Kong. However, this tool
is an aid rather than a complete substitute for the
carefully considered judgement of an experienced
intensive care clinician.
Author contributions
Concept or design: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: GM Joynt.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: GM Joynt.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. Christian MD, Sprung CL, King MA, et al. Triage: care
of the critically ill and injured during pandemics and
disasters: CHEST consensus statement. Chest 2014;146(4
Suppl):e61S-74S. Crossref
2. Joynt GM, Gopalan DP, Argent AA, et al. The Critical
Care Society of Southern Africa Consensus Statement
on ICU Triage and Rationing (ConICTri). S Afr Med J
2019;109:613-29. Crossref
3. Ling L, Ho CM, Ng PY, et al. Characteristics and outcomes of patients admitted to adult intensive care units in Hong
Kong: a population retrospective cohort study from 2008
to 2018. J Intensive Care 2021;9:2. Crossref
4. Phua J, Faruq MO, Kulkarni AP, et al. Critical care bed
capacity in Asian countries and regions. Crit Care Med
2020;48:654-62. Crossref
5. Murthy S, Wunsch H. Clinical review: international comparisons in critical care—lessons learned. Crit Care
2012;16:218. Crossref
6. Joynt GM, Gomersall CD, Tan P, Lee A, Cheng CA, Wong EL.
Prospective evaluation of patients refused admission to an
intensive care unit: triage, futility and outcome. Intensive
Care Med 2001;27:1459-65. Crossref
7. Shum HP, Chan KC, Lau CW, Leung AK, Chan KW,
Yan WW. Triage decisions and outcomes for patients with
Triage Priority 3 on the Society of Critical Care Medicine
scale. Crit Care Resusc 2010;12:42-9.
8. Nates JL, Nunnally M, Kleinpell R, et al. ICU Admission,
Discharge, and Triage Guidelines: a framework to enhance
clinical operations, development of institutional policies,
and further research. Crit Care Med 2016;44:1553-602. Crossref
9. Blanch L, Abillama FF, Amin P, et al. Triage decisions for
ICU admission: report from the task force of the World
Federation of Societies of Intensive and Critical Care
Medicine. J Crit Care 2016;36:301-5. Crossref
10. Joynt GM, Gopalan DP, Argent AA, et al. The Critical
Care Society of Southern Africa Consensus Guideline
on ICU Triage and Rationing (ConICTri). S Afr Med J
2019;109:630-62. Crossref
11. Legislative Council, HKSAR Government. Report of the
Select Committee to inquiry into the handling of the severe
acute respiratory syndrome outbreak by the Government
and the Hospital Authority. 2004. Available from: https://www.legco.gov.hk/yr03-04/english/sc/sc_sars/reports/sars_rpt.htm. Accessed 15 Sep 2020.
12. Gomersall CD, Tai DY, Loo S, et al. Expanding ICU facilities
in an epidemic: recommendations based on experience
from the SARS epidemic in Hong Kong and Singapore.
Intensive Care Med 2006;32:1004-13. Crossref
13. Guidet B, Hejblum G, Joynt G. Triage: what can we do to
improve our practice? Intensive Care Med 2013;39:2044-6. Crossref
14. Sprung CL, Joynt GM, Christian MD, Truog RD, Rello J, Nates JL. Adult ICU triage during the coronavirus
disease 2019 pandemic: who will live and who will die?
Recommendations to improve survival. Crit Care Med 2020;48:1196-202. Crossref
15. Flaatten H, Beil M, Guidet B. Prognostication in older ICU patients: mission impossible? Br J Anaesth 2020;125:655-7. Crossref
16. Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ
2005;173:489-95. Crossref
17. American Society of Anaesthesiologists. ASA Physical
Status Classification System. 2019. Available from: https://
www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system. Accessed 16 Sep 2020.
18. Gupta S, Hayek SS, Wang W, et al. Factors associated with death in critically ill patients with coronavirus disease 2019
in the US. JAMA Intern Med 2020;180:1-12.Crossref
19. Grasselli G, Greco M, Zanella A, et al. Risk factors
associated with mortality among patients with COVID-19
in intensive care units in Lombardy, Italy. JAMA Intern
Med 2020;180:1345-55. Crossref
20. Cummings MJ, Baldwin MR, Abrams D, et al. Epidemiology, clinical course, and outcomes of critically ill adults with
COVID-19 in New York City: a prospective cohort study.
Lancet 2020;395:1763-70. Crossref
21. Quill TE, Holloway R. Time-limited trials near the end of life. JAMA 2011;306:1483-4. Crossref
22. Vink EE, Azoulay E, Caplan A, Kompanje EJ, Bakker J.
Time-limited trial of intensive care treatment: an overview
of current literature. Intensive Care Med 2018;44:1369-77. Crossref
23. Bagshaw M, Majumdar SR, Rolfson DB, Ibrahim Q,
McDermid RC, Stelfox HT. A prospective multicenter
cohort study of frailty in younger critically ill patients. Crit
Care 2016;20:175. Crossref
24. Bagshaw SM, Stelfox HT, McDermid RC, et al. Association
between frailty and short- and long-term outcomes among
critically ill patients: a multicentre prospective cohort
study. CMAJ 2014;186:E95-102. Crossref
25. Brummel NE, Bell SP, Girard TD, et al. Frailty and subsequent disability and mortality among patients with
critical illness. Am J Respir Crit Care Med 2017;196:64-72. Crossref
26. Flaatten H, De Lange DW, Morandi A, et al. The impact of
frailty on ICU and 30-day mortality and the level of care
in very elderly patients (≥80 years). Intensive Care Med
2017;43:1820-8. Crossref
27. Knaus WA, Draper EA, Wagner DP, Zimmerman JE.
Prognosis in acute organ-system failure. Ann Surg
1985;202:685-93. Crossref
28. Peres Bota D, Melot C, Lopes Ferreira F, Nguyen Ba V,
Vincent JL. The Multiple Organ Dysfunction Score
(MODS) versus the Sequential Organ Failure Assessment
(SOFA) score in outcome prediction. Intensive Care Med
2002;28:1619-24. Crossref
29. Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related
Organ Failure Assessment) score to describe organ
dysfunction/failure. On behalf of the Working Group
on Sepsis-Related Problems of the European Society of
Intensive Care Medicine. Intensive Care Med 1996;22:707-10. Crossref
30. Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial
evaluation of the SOFA score to predict outcome in
critically ill patients. JAMA 2001;286:1754-8. Crossref
31. Joynt GM, Loo S, Taylor BL, et al. Chapter 3. Coordination
and collaboration with interface units. Recommendations
and standard operating procedures for intensive care unit
and hospital preparations for an influenza epidemic or
mass disaster. Intensive Care Med 2010;36(Suppl 1):S21-31. Crossref
32. Darvall JN, Bellomo R, Bailey M, et al. Frailty and outcomes
from pneumonia in critical illness: a population-based
cohort study. Br J Anaesth 2020;125:730-8. Crossref