Hong Kong Med J 2022 Feb;28(1):45–53 | Epub 23 Jul 2021
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Questionnaire survey on knowledge, attitudes,
and behaviour towards viral hepatitis among the Hong Kong public
Henry LY Chan, MD1,2; Grace LH Wong, MD1,3,4,5; Vincent WS Wong, MD1,3,4,5; Martin CS Wong, 1,6; Carol YK Chan, PhD7; Shikha Singh, PhD8
1 Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong
2 Department of Internal Medicine, Union Hospital, Hong Kong
3 Department of Medicine and Therapeutics, The Chinese University of Hong Kong, Hong Kong
4 Medical Data Analytic Centre (MDAC), The Chinese University of Hong Kong, Hong Kong
5 Institute of Digestive Disease, The Chinese University of Hong Kong, Hong Kong
6 JC School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong
7 Gilead Sciences, Hong Kong
8 Kantar Health, Singapore
Corresponding author: Dr Henry LY Chan (hlychan@cuhk.edu.hk)
Abstract
Introduction: We aimed to identify gaps in
knowledge, attitudes, and behaviours towards viral
hepatitis among the Hong Kong public and provide
insights to optimise local efforts towards achieving
the World Health Organization’s viral hepatitis
elimination target.
Methods: A descriptive, cross-sectional, self-reported
web-based questionnaire was administered
to 500 individuals (aged ≥18 years) in Hong Kong.
Questionnaire items explored the awareness and
perceptions of viral hepatitis-related liver disease(s)
and associated risk factors in English or traditional
Chinese.
Results: The majority (>80%) were aware that
chronic hepatitis B and/or C could increase the
risks of developing liver cirrhosis, cancer, and/or
failure. Only 55.8% had attended health screenings
in the past 2 years, and 67.6% were unaware of their
family’s history of liver diseases. Misperceptions
surrounding the knowledge and transmission
risks of viral hepatitis strongly hint at the presence
of social stigmatisation within the community.
Many misperceived viral hepatitis as airborne or
hereditary, and social behaviours (casual contact or
dining with an infected person) as a transmission
route. Furthermore, 62.4% were aware of hepatitis B
vaccination, whereas 19.0% knew that hepatitis C
cannot be prevented by vaccination. About 70%
of respondents who were aware of mother-to-child
transmission were willing to seek medical
consultation in the event of pregnancy. Gaps in knowledge as well as the likelihood of seeking
screening were observed across all age-groups and
education levels.
Conclusions: Comprehensive hepatitis education
strategies should be developed to address gaps in
knowledge among the Hong Kong public towards
viral hepatitis, especially misperceptions relevant
to social stigmatisation and the importance of
preventive measures, including vaccination and
screening, when exposed to risk factors.
New knowledge added by this study
- General awareness of potential risks of viral hepatitis developing into liver cirrhosis, cancer, or liver failure.
- Many still had misperceptions in terms of knowledge and transmission risk of viral hepatitis, suggestive of social stigma or discrimination towards infected individuals.
- Gaps in knowledge about viral hepatitis and likeliness to seek medical screening were observed across all age-groups, especially in respondents with secondary or higher education.
- We emphasise the importance of preventive measures including screening, diagnosis, treatment, and care to effectively manage viral hepatitis in Hong Kong.
- It is essential to develop universal education strategies to address misperceptions relevant to social stigmatisation, aligning with the community’s preferences for various information media channels to optimise information reception.
Introduction
Viral hepatitis is a major public health burden
worldwide and is the predominant aetiology of liver
cirrhosis and/or liver cancer.1 2 At least 325 million
individuals were reported to be infected with
viral hepatitis B (HBV) and/or C (HCV).2 3
Hong Kong is considered an endemic area with
intermediate incidence of HBV infection.4 In a local
epidemiological study conducted between 2015
and 2016, the seroprevalence of hepatitis B surface
antigen (HBsAg) was estimated at 7.8% among the
general population.5 In contrast, the prevalence rate
of HCV infection in Hong Kong has remained low.6
The seroprevalence of anti-HCV positivity among
new blood donors was 0.06% in 2017, compared with
0.11% in 2008.6 The local HCV prevalence among
the general population between 2015 and 2016 was
estimated at 0.5%,5 which has remained relatively unchanged since 1992.7
In 2016, the World Health Organization
(WHO) implemented a global elimination strategy
targeted to achieve at least a 90% diagnosis rate
of all viral hepatitis cases, an 80% treatment rate
for all diagnosed cases, and a 90% reduction in
the incidence of viral hepatitis cases.3 Recent
epidemiological studies in Hong Kong revealed that
the diagnosis and treatment uptake rates within
the community were significantly lacking, hovering
around 50% compared with the WHO’s 90%/80% targets.5 8 It has been suggested that inadequate
knowledge and awareness about viral hepatitis B and
C within Hong Kong’s community might be driving
this deficiency.5 8 9 10 In other parts of the world,
social stigma arising from poor knowledge has been
reported to reduce diagnosis and treatment rates
among high-risk individuals.11 12 13
In 2020, the Hong Kong Viral Hepatitis
Action Plan (HKVHAP) 2020-2024 was launched
to facilitate achieving the WHO’s eradication
target goals by 2030. The action plan outlined four
major strategies: (1) Awareness, (2) Surveillance,
(3) Prevention, and (4) Treatment to monitor and
implement local efforts towards achieving the
WHO’s 2030 elimination target.14
In the present study, we aimed to explore
the knowledge, attitudes, and behaviour within
Hong Kong’s general population pertaining to viral
hepatitis and related risk factors. Furthermore, in
this study, we sought to identify potential gaps in
existing knowledge, attitudes, and behaviour related
to the WHO’s global viral hepatitis elimination
strategy to optimise local efforts towards the WHO’s
target goal.
Methods
Study population
Potential respondents were recruited through an
existing, general purpose (ie, not healthcare-specific)
web-based consumer panel via email in February
2020. Respondents who were aged ≥18 years,
had access to online or comfort with web-based
administration, and were able to read English or
traditional Chinese were eligible to participate in
the study. There were no exclusion criteria for this
study. All eligible respondents explicitly agreed to
join the panel and provided informed online consent
to participate in the study.
Assuming 95% confidence intervals and 50%
response distribution, responses collected from
500 adult individuals were deemed sufficient to
provide descriptive estimates with 4.33% margin of
error.
Study design
Items pertaining to awareness and perceptions
of liver diseases among the general public were
explored using a self-administered web-based
survey. The survey questionnaire was developed
in English and translated into traditional Chinese.
The translation was validated by a linguist from a
translation company who is a native speaker of the
language. The developed questionnaire was reviewed
and finalised by a steering committee comprising
gastroenterology and/or hepatology experts from
11 countries/territories as part of a regional liver
index study (Lee Mei-hsuan et al, unpublished). All respondents completed the questionnaire in either
English or Chinese. Only de-identified data were
collected.
Survey questionnaire
The internal consistency of the questionnaire from the regional liver index study was assessed by
Cronbach’s alpha (threshold: alpha >0.7). As part
of this study’s objective to explore the knowledge,
attitudes, and behaviour of Hong Kong’s public
towards viral hepatitis-related liver diseases, seven
items were extracted from the questionnaire used in
a regional liver index study. These items pertained
to the awareness and knowledge of liver diseases as
well as the respondents’ attitudes and behaviours
towards screening and diagnosis of liver diseases
(online supplementary Appendix 1; Q1-7).
Seven screener questions (online
supplementary Appendix 1; S1-7) pertaining to the
respondents’ socio-demographic characteristics,
including age, sex, education, monthly household
income, and their awareness of different types of
hepatitis were also included in this study.
Respondents who indicated their awareness
of ‘hepatitis B’ or ‘hepatitis C’ in screener item S7
proceeded to answer Q1(I)-Q2(I) or Q1(II)-Q2(II).
Female respondents who correctly recognised the
statement ‘from a pregnant mother to her baby’ in
Q2f(I) or Q2f(II) proceeded to answer Q3c.
Descriptive analysis
This study was exploratory and descriptive in nature. Respondents’ characteristics and responses
to the survey questions were summarised and
are presented as frequencies and percentages. No
statistical analyses were performed.
Missing data were random; all data were
reported, including those of respondents who
declined to answer certain screener questions, such
as on monthly household income. Missing data for
any question were excluded from analysis of that
question only, not from the whole study.
Results
Study population characteristics
Among the respondents, 68.0% were aged ≥35 years,
and 56.0% were female. Among the respondents,
59.0% had completed university or higher education,
and 76.0% possessed private insurance. About 70%
of respondents had a monthly household income of
≥HK$30 000. The respondents’ sex, age, education
level, and household income were reflective of Hong
Kong’s population.15 Approximately half of the
respondents (55.8%) self-reported having attended
health screenings within the last 2 years, and about
32.4% of them were aware of their family history
pertaining to liver diseases (Table 1).
General knowledge and awareness of
hepatitis B and C
A higher proportion of respondents were aware of
hepatitis B (93.0%, 465/500) than hepatitis C (46.4%,
232/500) [online supplementary Appendix 2]. The
majority (>80%) were aware that hepatitis B and
C can cause liver failure and increase the risks of
developing liver cirrhosis and liver cancer (Fig 1a).
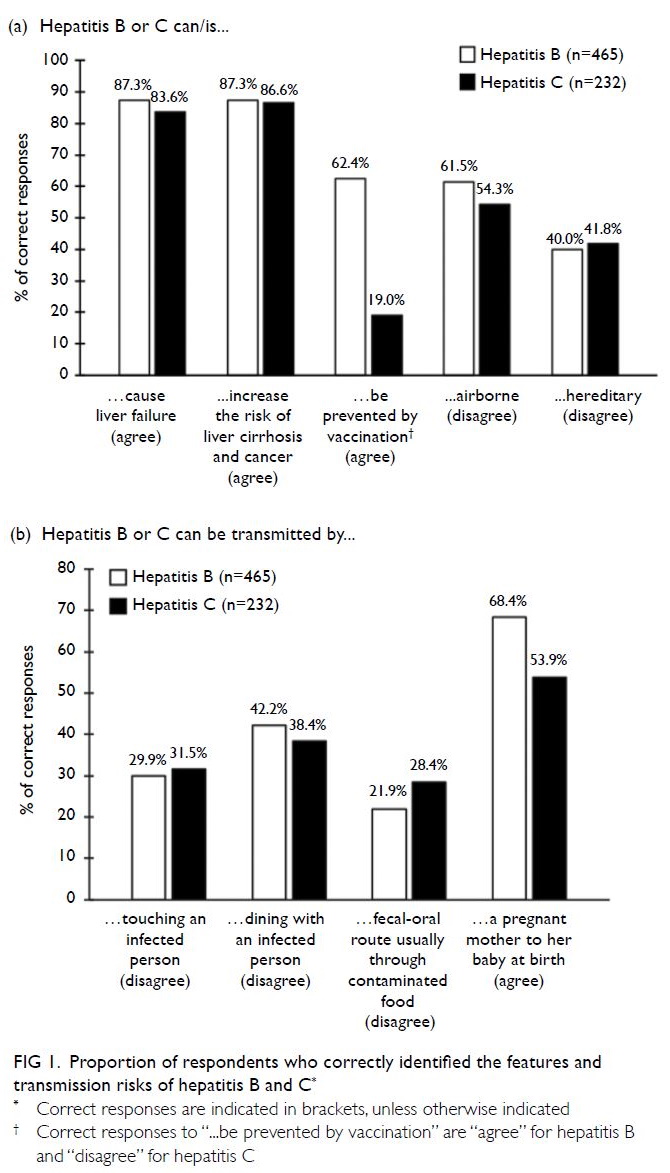
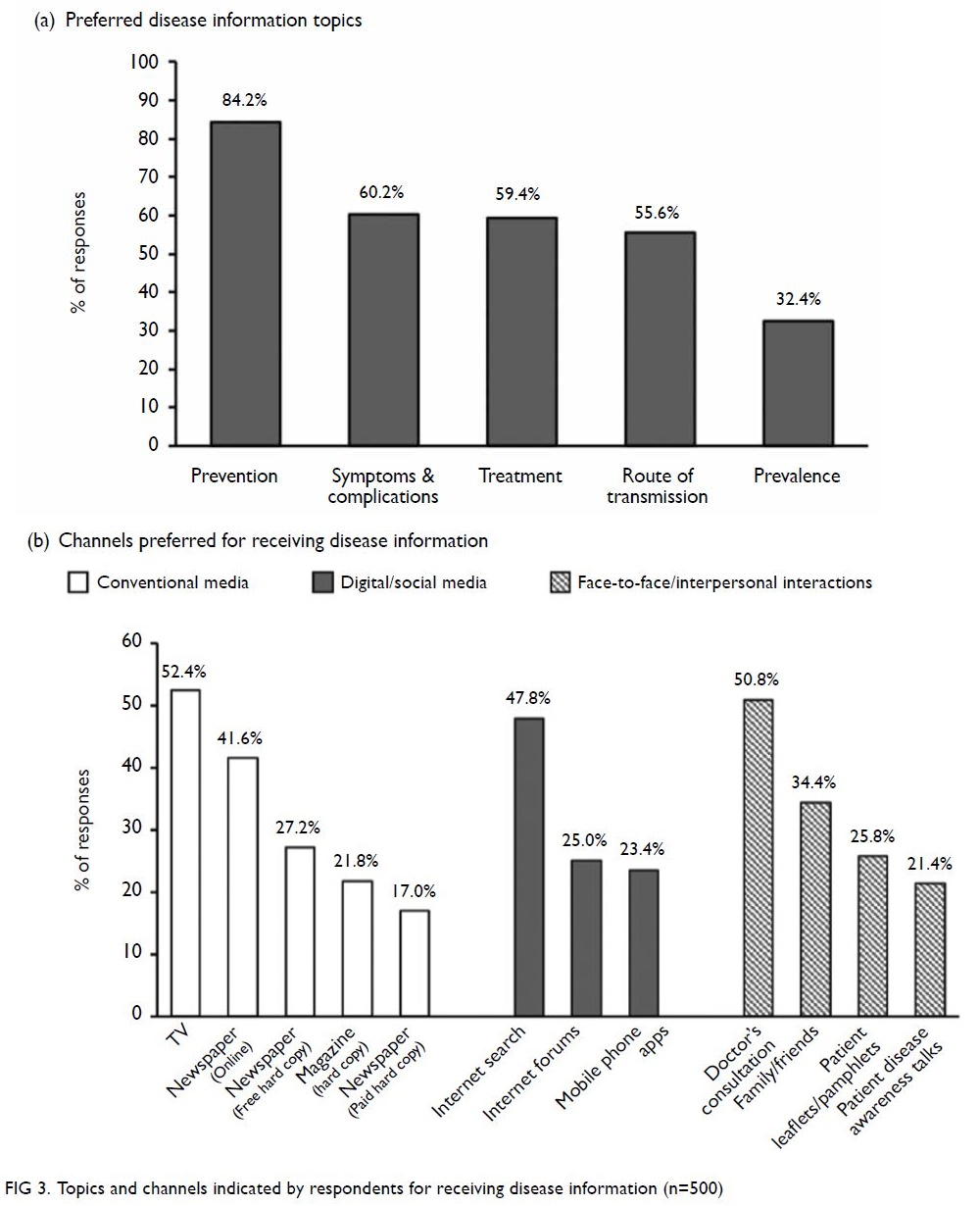
Figure 1. Proportion of respondents who correctly identified the features and transmission risks of hepatitis B and C
About 60% of respondents who were aware of
hepatitis B knew that HBV is not airborne (61.5%)
and can be prevented by a vaccine (62.4%). Only
approximately 40% (186/465) of the respondents
were aware that hepatitis B is not hereditary (Fig 1a).
In contrast, only 19.0% (n=44/232) of those aware
of hepatitis C knew that it cannot be prevented by
vaccination, and about half knew that it is neither
airborne (54.3%) nor hereditary (41.8%) [Fig 1a].
About half of the respondents aged <25 years
(58.2%) and 55 to 64 years (46.9%) were not aware
that hepatitis B is preventable by vaccination. More
than half of the respondents across all age-groups were unaware that hepatitis B is not hereditary,
with the highest proportion aged <25 years (80.0%).
A substantial proportion of respondents (>35%)
with either secondary or university education
misperceived hepatitis B to be airborne (38.5%;
39.8%) or hereditary (62.0%; 59.7%) [online supplementary Appendix 3].
More than 70% of respondents across all age-groups and >80% with secondary school or university
education misperceived that a vaccine could prevent
hepatitis C. About half of subjects aged 25 to 44 years
and ≥65 years were not aware that hepatitis C is
not airborne, whereas >70% of those aged 25 to
34 years and ≥65 years misperceived hepatitis C
to be hereditary. More than half of respondents
with university (61.0%) or postgraduate (51.9%)
education misperceived hepatitis C as hereditary
(online supplementary Appendix 4).
Knowledge about the transmission risks of
hepatitis B and C
At least 30% of respondents rightly perceived that
(1) touching an infected person (HBV: 29.9%; HCV:
31.5%), (2) the faecal-oral route (21.9%; 28.4%); or (3)
dining with an infected person (42.2%; 38.4%) were
not possible modes of transmission of viral hepatitis
B and C (Fig 1b). More than half of the respondents
were aware of the mother-to-child transmission risk
of HBV (68.4%) and HCV (53.9%) [Fig 1b]. Awareness
of other transmission modes of HBV and HCV are
detailed in online supplementary Appendix 2.
More than 60% of respondents across all age-groups and those with at least secondary school
education did not correctly identify the transmission
risks of HBV (online supplementary Appendix 5):
more than half with secondary or university
education misperceived touching (73.3%; 70.4%) or
dining with an infected person (60.4%; 56.2%) as
HBV transmission risks.
With regard to hepatitis C, more than half of
the respondents aged ≥35 years and at least 60% of
individuals with at least secondary-level education
were unaware or incorrectly identified with the
statements regarding social interaction and food
contamination as HCV transmission risks. Notably,
no respondents with the primary school education
level were aware of hepatitis C (online supplementary Appendix 6).
Likelihood of attending health screening in
the event of family planning
Among the 280 female respondents, 65% correctly identified mother-to-child transmission as a
transmission risk of viral hepatitis B and/or C
(Fig 2). Among these respondents, 70.3% expressed
that they were extremely likely or likely to seek a
doctor’s consultation to get tested if they were or
intended to become pregnant (Fig 2).
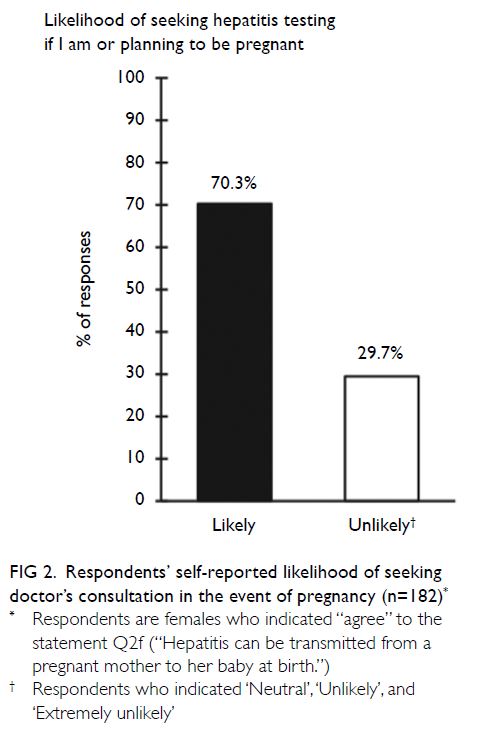
Figure 2. Respondents’ self-reported likelihood of seeking doctor’s consultation in the event of pregnancy (n=182)
About one-fifth of the respondents with
university (25.3%) or postgraduate (21.4%) education
indicated that they were unlikely (neutral, unlikely,
or extremely unlikely) to get tested for viral hepatitis
in the event of pregnancy planning. About 40% of
the respondents aged <25 years (46.7%) expressed
that they were unlikely to seek screening if they
wanted to become or became pregnant (Table 2).
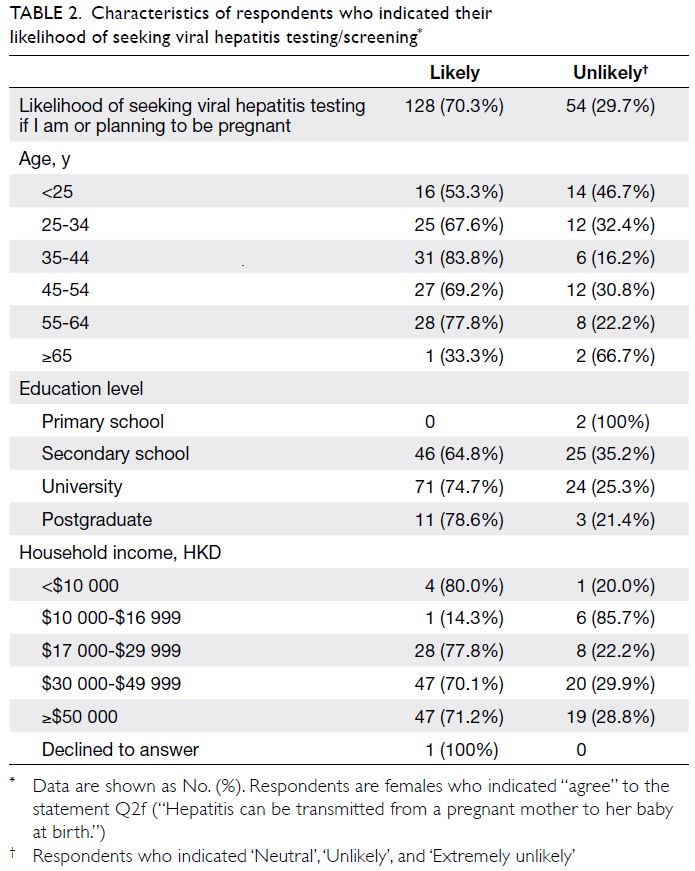
Table 2. Characteristics of respondents who indicated their likelihood of seeking viral hepatitis testing/screening
Preferred disease information topics and
channels
The top three disease information topics that
the respondents stated that they would like to
understand more were disease prevention (84.2%),
disease symptoms and complications (60.2%), and
treatment (59.4%) [Fig 3a].
Among the various information dissemination
channels, about half of the respondents preferred
TV (conventional media [52.4%]), internet
search (digital/social media [47.8%]) and doctor’s
consultation (face-to-face/interpersonal interactions
[50.8%]) [Fig 3b].
Discussion
There was an improved general awareness (>80%)
about the sequelae of HBV and HCV compared with that observed in 2010 (>70%).16 However, a
substantial proportion (>60%) of respondents across
all age-groups and education levels in Hong Kong
held misconceptions about HBV and HCV and their
transmission risks.
The local awareness of HBV vaccination
among Hong Kong respondents (62.4%) was higher
than that of Nigeria (31.9%)17 but lower than that
of Singapore (75.1%).18 Among those unaware of
hepatitis B vaccination in Hong Kong, the majority
were aged ≥25 years. This is concerning because
these respondents were born before the rollout of
the local vaccination programme in 1988. Extensive
global and local studies have reported that the
implementation of HBV vaccination effectively
reduced the incidence and seroprevalence of HBV-associated
viral hepatitis.3 6 14 19 20 A recent study
in Nigeria showed a relationship between HBV
vaccination and knowledge about viral hepatitis,17
suggesting an unmet need to improve knowledge
about HBV to increase HBV vaccination uptake,
particularly in older adults.
Moreover, in this study, we observed a general
local misperception that a vaccine is available
for HCV, which has been similarly observed
globally,18 21 although we observed a slightly higher
local awareness rate (19.0%) than that in Singapore
(15.0%).18 This lack of awareness pertaining to HCV
might impede the adoption of correct preventive
measures against hepatitis C infection.22
Both the WHO’s hepatitis elimination
strategy and HKVHAP 2020-2024 emphasised the
importance of combating any forms of stigmatisation
or discrimination in the implementation of
awareness and communication strategies to improve
health outcomes among high-risk individuals.3 14
Social stigmatisation and discrimination stem from
the lack of knowledge within society12 23 and among healthcare practitioners.10 Misperceptions such
as the idea that hepatitis can be spread by sharing
of food or eating utensils, the faecal-oral route, or
touching an infected person (perceived by >60% of
the study’s respondents) often underlie the social
stigmatisation surrounding viral hepatitis.16 18 23 24
These often result in the avoidance of casual contact,
self-isolation,11 23 or denial of potential employment
or professional advancement,25 26 as experienced
by infected individuals across the world. Many
respondents without HBV infection in China
expressed discomfort about being in close contact
or sharing meals with HBV-infected individuals
and felt that they should not be allowed to work
in restaurants or with children.25 Similarly, 55.2% respondents in a 2019 Korean survey thought HCV
patients should use separate towels and dishes,27 which is an indication of the misperception of HCV
transmission by causal contact.
Over time, these social behaviours arising from
misperceptions could result in a paradox for those
infected with viral hepatitis, as stigma and shame
could lead them to conceal their condition and
avoid seeking the necessary medical treatment.26 28
Therefore, there is a need to adopt a comprehensive
approach to raise community awareness and
knowledge to tackle stigmatisation against infected
individuals.
The belief that viral hepatitis is hereditary (ie, it could be inherited through ‘bad genes’29) could
potentially result in the misunderstanding that there
are no preventive measures against viral hepatitis. In
fact, mother-to-child transmission is a major route
of hepatitis B transmission in Asia. The potential
confusion between a vertically transmitted disease
and a hereditary one could impede efforts to reduce
community transmission of viral hepatitis, as many
might not bother to find out more information or
proactively seek screening.
The HBsAg seropositivity screening during
pregnancy and neonatal vaccination are integral
parts of HKVHAP and the WHO’s hepatitis
elimination strategy to prevent mother-to-child
transmission.3 14 Prevention of perinatal transmission
of HBV in Hong Kong includes an additional viral
load screening of HBsAg-seropositive mothers to
guide maternal antiviral therapy. Approximately
70% of pregnant women in Hong Kong (between
May 2017 and December 2019) reportedly did not
undergo viral load testing or regular hepatological
surveillance before pregnancy.30 This is an important
public health issue, as viral load in mothers who
are hepatitis B carriers is a key influencing factor of
immunoprophylaxis success in their babies.31 Among
the 280 female respondents, only 128 (45.7%) were
aware of the risk of mother-to-child transmission
and likely to seek medical consultation in the event
of pregnancy, suggesting a gap in women’s awareness and knowledge about viral hepatitis in Hong Kong.
Besides vertical transmission, horizontal
spread is also an important means of HBV infection.
In this study, 67.6% of respondents were unaware of
their family’s history of liver disease(s), and only 50%
knew that sexual contact is a transmission risk of HBV
and HCV (online supplementary Appendix 2). This
suggests an unmet need to educate the community
about not only mother-to-child transmission, but
also other transmission risks. More robust education
efforts are needed to raise the population’s level of
knowledge and awareness about viral hepatitis
to work towards the WHO’s elimination goal.
Such outreach efforts could be aligned with the
respondents’ preferences for information media
channels such as TV, internet search, and doctor’s
consultation to optimise community reception.
This study has some limitations. Being a self-administered
cross-sectional study based on self-reported
data, the study is subject to recall bias. As
such, data validation could not be performed, and
no causal associations could be made. Respondents
who lack internet access or comfort with online
administration could be underrepresented.
Furthermore, this study did not consider factors that
could influence respondents’ levels of knowledge
and/or awareness or attitudes towards HBV and
HCV (eg, respondents’ health consciousness or
vaccination or hepatitis status). With <60% having
attended a health screening in the past 2 years
and <70% expressing a high likelihood of medical
consultation when exposed to risk factors, it would
be insightful to explore the reasons for these gaps
in proactive health-seeking behaviours. This would
facilitate addressing and dispelling concerns to
promote precautionary measures and health-seeking
behaviours to reduce community transmission.
As this study is exploratory and descriptive
in nature, statistical analyses were not performed
to evaluate factors associated with the gaps in
knowledge, awareness, and/or practices pertaining
to hepatitis B and C; thus, the associations of
respondents’ characteristics could not be identified
in this study. Additional analyses would be warranted
in future studies to confirm any independent factors
associated with the community’s levels of knowledge
and awareness.
Conclusions
In this study, we found that respondents had a
general awareness of hepatitis B and C. However, our
findings revealed gaps in respondents’ knowledge
and understanding of the transmission risks of
hepatitis B and C as well as awareness of their family
history related to liver disease(s). The findings
suggest that there may be social stigmatisation or
discrimination against people with HBV and HCV within the community, which may deter some from
undergoing screening and diagnosis.
It is essential to develop targeted education
strategies with special attention towards addressing
misperceptions relevant to social stigmatisation
or discrimination and raise the importance of
preventive measures such as vaccination and
screening when exposed to risk factors. Outreach
of such targeted education efforts should be aligned
with the community’s preferred information
channels to maximise information accessibility.
Author contributions
Concept or design: All authors.
Acquisition of data: S Singh.
Analysis or interpretation of data: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: S Singh.
Analysis or interpretation of data: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
HLY Chan is an advisor to AbbVie, Aligos, Arbutus, Gilead
Sciences, GSK, Hepion, Janssen, Merck, Roche, Vaccitech,
Venatorx, and Vir Biotechnology; and a speaker for Gilead
Sciences, Mylan, and Roche.
GLH Wong has served as an advisory committee
member for Gilead Sciences; as a speaker for Abbott, Abbvie,
Bristol-Myers Squibb, Echosens, Furui, Gilead Sciences,
Janssen and Roche; and received a research grant from Gilead
Sciences.
VWS Wong served as a consultant or advisory board
member for 3V-BIO, AbbVie, Allergan, Boehringer Ingelheim,
the Center for Outcomes Research in Liver Diseases,
Echosens, Gilead Sciences, Hanmi Pharmaceutical, Intercept,
Inventiva, Merck, Novartis, Novo Nordisk, Perspectum
Diagnostics, Pfizer, ProSciento, Sagimet Biosciences,
TARGET PharmaSolutions, and Terns; and a speaker for
AbbVie, Bristol-Myers Squibb, Echosens, and Gilead Sciences.
He has received a grant from Gilead Sciences for fatty liver
research. He is also a Co-founder of Illuminatio Medical
Technology Limited.
As an editor of the Journal, MCS Wong was not involved in the peer review process for this article.
Acknowledgement
The authors acknowledge valuable support from Dr Vince
Grillo of Kantar Health overseeing the development of the
project. The authors thank Dr Amanda Woo of Kantar Health
for providing medical writing and editorial support, which
was funded by Gilead Sciences, Hong Kong, in accordance
with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3). The translation of the questionnaire
from English to traditional Chinese was performed by
GlobaLexicon Limited, United Kingdom and funded by Gilead
Sciences, Hong Kong. The authors acknowledge the members
of the steering committee for their contribution in reviewing
and finalising the questionnaire: Dr Mei-hsuan Lee, National Yang Ming Chiao Tung University (Taiwan); Dr Sang-hoon
Ahn, Yonsei University College of Medicine (South Korea);
Dr Henry LY Chan, Union Hospital (Hong Kong); Dr Asad
Choudhry, Chaudhry Hospital (Pakistan); Dr Rino Alvani
Gani, University of Indonesia (Indonesia); Dr Rosmawati
Mohamed, University of Malaya (Malaysia), Dr Janus P Ong,
University of the Philippines (Philippines); Dr Akash Shukla,
King Edward Memorial Hospital, Global Hospital (India); Dr
Chee-kiat Tan, Singapore General Hospital (Singapore); Dr
Tawesak Tanwandee, Siriraj Hospital, Mahidol University
(Thailand); and Dr Pham-thi Thu Thuy, Ho Chi Minh Medic
Medical Center (Vietnam).
Funding/support
This study was funded by Gilead Sciences, Hong Kong. Kantar Health, Singapore, received funding from Gilead Sciences,
Hong Kong, for the conduct of the study and development of
the manuscript.
Ethics approval
All eligible respondents explicitly agreed to join the panel and provided informed online consent to participate in the study.
References
1. Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol 2019;70:151-71. Crossref
2. World Health Organization. Hepatitis in the Western Pacific. Available from: https://www.who.int/westernpacific/health-topics/hepatitis. Accessed 3 Aug 2020.
3. World Health Organization. Global Health Sector
Strategy on Viral Hepatitis, 2016-2021: towards ending
viral hepatitis. Available from: https://apps.who.int/iris/bitstream/handle/10665/246177/WHO-HIV-2016.06-eng.pdf;jsessionid=F5934335456A761C7349258535E3E5EC?sequence=1. Accessed 14 Dec 2020.
4. Lin AW, Wong KH. Surveillance and response of hepatitis B
virus in Hong Kong Special Administrative Region, 1988-2014. Western Pac Surveill Response J 20163;7:24-8. Crossref
5. Liu KS, Seto WK, Lau EH, et al. A territory-wide prevalence
study on blood-borne and enteric viral hepatitis in Hong
Kong. J Infect Dis 2019;219:1924-33. Crossref
6. Viral Hepatitis Control Office, Special Preventive
Programme, Centre for Health Protection, Department of
Health, Hong Kong SAR Government. Surveillance of viral
hepatitis in Hong Kong—2017 update report. Available
from: https://www.chp.gov.hk/files/pdf/viral_hepatitis_report.pdf. Accessed 14 Jan 2021.
7. Chan GC, Lim W, Yeoh EK. Prevalence of hepatitis C infection in Hong Kong. J Gastroenterol Hepatol 1992;7:117-20. Crossref
8. Hui YT, Wong GL, Fung JY, et al. Territory-wide
population-based study of chronic hepatitis C infection
and implications for hepatitis elimination in Hong Kong.
Liver Int 2018;38:1911-9. Crossref
9. Lao TT, Sahota DS, Suen SS, Lau TK, Leung, TY. Chronic
hepatitis B virus infection and rubella susceptibility in
pregnant women. J Viral Hepat 2010;17:737-41. Crossref
10. Paterson BL, Backmund M, Hirsch G, Yim C. The depiction of stigmatization in research about hepatitis C. Int J Drug
Policy 2007;18:364-73. Crossref
11. Zacks S, Beavers K, Theodore D, et al. Social stigmatization and hepatitis C virus infection. J Clin Gastroenterol
2006;40:220-4. Crossref
12. Mokaya J, McNaughton AL, Burbridge L, et al. A blind
spot? Confronting the stigma of hepatitis B virus (HBV)
infection—a systematic review. Wellcome Open Res
2018;3:29. Crossref
13. Marinho RT, Barreira DP. Hepatitis C, stigma and cure.
World J Gastroenterol 2013;19:6703-9. Crossref
14. Viral Hepatitis Control Office, Department of Health, Hong
Kong SAR Government. Hong Kong Viral Hepatitis Action
Plan 2020-2024. Available from: https://www.hepatitis.gov.hk/english/document_cabinet/action_plan.html. Accessed 4 Dec 2020.
15. Census and Statistics Department, Hong Kong SAR
Government. Population and Household Statistics Analysed
by District Council District. Available from: https://www.statistics.gov.hk/pub/B11303012019AN19B0100.pdf. Accessed 14 Jan 2021.
16. Leung CM, Wong WH, Chan KH, et al. Public awareness of
hepatitis B infection: a population-based telephone survey
in Hong Kong. Hong Kong Med J 2010;16:463-9.
17. Eni AO, Soluade MG, Oshamika OO, Efekemo OP,
Igwe TT, Onile-ere OA. Knowledge and awareness of
hepatitis B virus infection in Nigeria. Ann Glob Health
2019;85:56. Crossref
18. Tan CK, Goh GB, Youn J, Yu JC, Singh S. Public awareness
and knowledge of liver health and diseases in Singapore.
J Gastroenterol Hepatol 2021 Mar 18. Epub ahead of
print. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/jgh.15496. Accessed 2 May 2021. Crossref
19. Meireles LC, Marinho RT, Van Damme P. Three decades
of hepatitis B control with vaccination. World J Hepatol
2015;7:2127-32. Crossref
20. Posuwan N, Wanlapakorn N, Sintusek P, et al. Towards the
elimination of viral hepatitis in Thailand by the year 2030. J
Virus Erad 2020;6:100003. Crossref
21. Ha S, Timmerman K. Awareness and knowledge of
hepatitis C among health care providers and the public: a
scoping review. Can Commun Dis Rep 2018;44:157-65. Crossref
22. Wait S, Kell E, Hamid S, et al. Hepatitis B and hepatitis C in
southeast and southern Asia: challenges for governments.
Lancet Gastroenterol Hepatol 2016;1:248-55. Crossref
23. Lee H, Fawcett J, Kim D, Yang JH. Correlates of hepatitis B
virus-related stigmatization experienced by Asians:
a scoping review of literature. Asia-Pac J Oncol Nurs
2016;3:324-34. Crossref
24. Smith-Palmer J, Cerri K, Sbarigia U, et al. Impact of stigma
on people living with chronic hepatitis B. Patient Relat
Outcome Meas 2020;11:95-107. Crossref
25. Huang J, Guan ML, Balch J, et al. Survey of hepatitis B
knowledge and stigma among chronically infected patients
and uninfected persons in Beijing, China. Liver Int
2016;36:1595-603. Crossref
26. Northrop JM. A dirty little secret: stigma, shame and
hepatitis C in the health setting. Med Humanit 2017;43:218-24. Crossref
27. Choi GH, Jang ES, Kim JW, Jeong SH. A survey of the
knowledge of and testing rate for hepatitis C in the general
population in South Korea. Gut Liver 2020;14:808-16. Crossref
28. Gautier RL, Wallace J, Richmond JA, Pitts M. The personal
and social impact of chronic hepatitis B: a qualitative
study of Vietnamese and Chinese participants in Australia.
Health Soc Care Community. 2020. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/hsc.13197.
Accessed 27 Jan 2021. Crossref
29. Haga SB, Barry WT, Mills R, et al. Public knowledge of and
attitudes toward genetics and genetic testing. Genet Test
Mol Biomarkers 2013;17:327-35. Crossref
30. Hui PW, Ng C, Cheung KW, Lai CL. Acceptance of
antiviral treatment and enhanced service model for
pregnant patients carrying hepatitis B. Hong Kong Med J
2020;26:318-22. Crossref
31. Cheung KW, Seto MT, Wong SF. Towards complete
eradication of hepatitis B infection from perinatal
transmission: review of the mechanisms of in utero
infection and the use of antiviral treatment during
pregnancy. Eur J Obstet Gynecol Reprod Biol 2013;169:17-23. Crossref