© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Prevalence of unruptured intracranial aneurysms
in the Hong Kong general population and comparison with individuals with symptoms or history of cerebrovascular disease
A paper from the Hong Kong Society of Interventional and Therapeutic Neuroradiology Endorsed by
the Hong Kong Stroke Society
Simon CH Yu, MD, FRCR1,2; PW Cheng, FRCR3; Gregory E Antonio, MD, FHKCR3; Sabrina CC Chan, MPhil1,2; Tiffany WW Lau, MSc1,2; Hector TG Ma, MD, FHKCR3; for The Hong Kong Society of Interventional and Therapeutic Neuroradiology
1 Department of Imaging and Interventional Radiology, The Chinese University of Hong Kong, Hong Kong
2 Vascular and Interventional Radiology Foundation Clinical Science Centre, The Chinese University of Hong Kong
3 Scanning Department, St Teresa’s Hospital, Hong Kong
Corresponding author: Prof Simon CH Yu (simonyu@cuhk.edu.hk)
Abstract
Introduction: We aimed to estimate the prevalence
of unruptured intracranial aneurysms among the
general population in Hong Kong, which has not yet
been determined; we also estimated its prevalence
among individuals who have symptoms or history of
cerebrovascular disease.
Methods: This retrospective cross-sectional study
included the first cerebral magnetic resonance
angiography (MRA) records of Hong Kong citizens
who underwent MRA in a single hospital between
July 1994 and December 2009. Records were
excluded for individuals with repeat examination or
a personal/family history of intracranial aneurysm.
The overall prevalence of unruptured intracranial
aneurysms in Hong Kong was estimated from the
sex- and age-specific prevalences in the General
group, as well as census data regarding the sex and
age composition of the Hong Kong population.
Results: In total, data on 6637 individuals were
included. Asymptomatic individuals were assumed
to represent the general public and allocated into a
General group (n=3597); the remaining individuals
were allocated into a Symptom group (n=2409) or a
cerebrovascular disease (CVD) group (n=707). The
prevalence of unruptured intracranial aneurysms was
significantly lower in the General group (176/3597,
4.9%) than in the Symptom group (152/2409, 6.3%; P=0.018). The prevalences in women and men were
5.9% (107/1809) and 3.9% (69/1788), respectively,
in the General group (P=0.004). These prevalences
generally increased with age. The prevalences did
not significantly differ between the General and
CVD groups.
Conclusions: The estimated overall prevalence of
unruptured intracranial aneurysm in the Hong Kong
population was 3.6%. The prevalence of unruptured
intracranial aneurysm was significantly higher in the
Symptom group than in the General group.
New knowledge added by this study
- The estimated overall prevalence of unruptured intracranial aneurysm in the Hong Kong population is 3.6%, according to the study findings and census data regarding the current sex and age composition of the Hong Kong population.
- The prevalence of unruptured intracranial aneurysm in individuals with any single or combination of symptoms related to intracranial aneurysms, with or without a history of cerebrovascular disease, is significantly higher than the prevalence in individuals without any such symptoms or history of cerebrovascular disease.
- Among all groups and subgroups, the prevalence of unruptured intracranial aneurysm was consistently higher in women than in men.
- This analysis of unruptured intracranial aneurysm prevalence in individuals with symptoms and individuals with a known history of cerebrovascular disease provides useful information for physicians who must counsel such patients.
- Estimation of the overall prevalence of unruptured intracranial aneurysm in the Hong Kong population provides useful information for medical service planning by health authorities.
Introduction
Intracranial aneurysms constitute approximately 80%
of all nontraumatic subarachnoid haemorrhages.1
Aneurysmal subarachnoid haemorrhage could
be associated with 30-day mortality of 45%, and
approximately half of the survivors will have
irreversible brain damage.2 Knowledge of the
intracranial aneurysm prevalence in a population
allows health authorities to assess the severity of
the problem and formulate appropriate healthcare
policies. The prevalence of unruptured intracranial
aneurysm has considerably varied among studies
according to the detection method used.3 4 5 6 7 8 9 10 11 12 13 14 15 Notably,
the prevalence of unruptured intracranial aneurysm
generally increases with imaging sensitivity. Studies
that used three-dimensional time-of-flight magnetic
resonance angiography (MRA) with 3-T magnetic
resonance imaging (MRI) showed a prevalence of
7.0% in a general population of Chinese adults age
35 to 75 years.14 Time-of-flight MRA is an ideal
imaging technique for the analysis of intracranial
aneurysm prevalence because of its non-invasive
nature and its diagnostic accuracy, which is
comparable to the accuracy of digital subtraction
angiography.16 17 Information concerning the
prevalence of intracranial aneurysms in the general
population is important but has been unavailable in
Hong Kong. We aimed to determine the prevalences
of unruptured intracranial aneurysms in the Hong
Kong population, individuals with symptoms related
to intracranial aneurysms, and individuals with
cerebrovascular disease (CVD).
Methods
Study design
Data on cerebral MRA examinations of Hong Kong
residents conducted at St Teresa’s Hospital, a private
community hospital that serves patients throughout
Hong Kong, were extracted from hospital electronic
records. Data were excluded if they were repeat
MRA examinations or if the individual had a known
history of ruptured/unruptured aneurysm or a
family history of cerebral aneurysm.
Magnetic resonance angiography was the
first-line imaging method used for assessment of
intracranial vessels at St Teresa’s Hospital during
the study period. Information retrieved from clinical
records included the indication for MRA, presenting
symptoms, medical history, family history, and MRA
findings. Three groups were formed for analysis: a
Symptom group that consisted of individuals who
presented with any single symptom or combination
of symptoms such as headache, any neurological
symptoms related to intracranial aneurysms
such as localised pain above or behind the eye,
nausea, vomiting, or any visual symptom related to
intracranial aneurysms (eg, diplopia, vision blurring, proptosis, or ptosis); a General group that consisted
of individuals without any symptoms that were
criteria for inclusion in the Symptom group and
without a known history of CVD; and a CVD group
that consisted of individuals with a known history
of ischaemic stroke, transient ischaemic attack,
intracranial stenosis, a history of intracerebral
haemorrhage, arteriovenous malformation, or any
other CVD other than cerebral aneurysm. The
prevalences of cerebral aneurysm within these
groups were recorded and compared among groups.
The characteristics of aneurysms in the General
group were extensively characterised.
Magnetic resonance angiography
The usual contra-indications for MRI were adopted.18
Magnetic resonance angiography was performed
with a Siemens MAGNETOM MRI scanner (1.5T
Vision, 1.5T Sonata, 1.5T Avanto, 3T Trio) using
non-contrast time-of-flight sequence (repetition
time 21-40 ms, echo time 3.8-7.2 ms, flip angle
18°-25°, matrix 195×512 to 250×512, field of view
200-230, slab 3-6, slices per slab 36-48, slice thickness
0.5-0.6 mm, acquisition time 4.32-8.45 minutes, with
or without magnetic transfer). All MRI examinations
were performed and reported by the same team
of radiographers and radiologists; each member
had at least 5 years of experience. The diagnosis of
aneurysms in each participant was based on definite
findings in the radiology report. Cases involving
an inconclusive diagnosis of aneurysm without
confirmatory computed tomography angiography
or digital subtraction angiography findings were not included. Aneurysm types were saccular or fusiform.
Aneurysm sizes were recorded as ≤5 mm, >5 mm
to <10 mm, 10 to 20 mm, or >20 mm. Aneurysm
locations were internal carotid artery, middle
cerebral artery, anterior cerebral artery, posterior
cerebral artery, or vertebrobasilar artery. Anterior
communicating artery aneurysms were included
in the anterior cerebral artery location category.
Posterior communicating artery aneurysms were
included in the posterior cerebral artery location
category.
Analysis of aneurysm prevalence
Prevalence analysis was based on participants, rather
than aneurysms. In the General group, sex- and age-specific
prevalences were analysed. The age threshold
that demarcated the greatest change in prevalence
was identified using odds ratio (OR) for the General
group overall, as well as for all male participants
and for all female participants within the General
group. The prevalences in the General group overall,
as well as its sex- and age-specific subgroups, were
compared with the prevalences in the Symptom and
CVD groups. The sizes and locations of unruptured
intracranial aneurysms were analysed in the General
group. For participants with multiple aneurysms,
the largest aneurysm was selected for size and
location analysis. The prevalence in the Hong Kong
population was estimated from the sex- and age-specific
prevalence in the General group in this
study, with reference to the sex and age composition
of the Hong Kong population. Because this cross-sectional
analysis involved a long study period (ie,
15 years), a separate analysis of the sex- and age-specific prevalences of aneurysms among
participants examined in the final 5 years was
performed to determine whether any significant
variations in sex- and age-specific prevalences
occurred over time.
Statistical analysis
Statistical analyses were conducted using SPSS
for Windows (version 20.0; IBM Corp, Armonk
[NY], United States). All categorical variables are
presented as number and percentage. All continuous
variables are presented as median and interquartile
range. Comparisons of prevalences among groups
and subgroups were carried out using the Chi
squared test. The Mann-Whitney U test was used
for comparisons of continuous variables. P<0.05
was considered to indicate statistical significance.
Comparisons of aneurysm prevalences between
participant groups according to an age threshold
were conducted using OR and 95% confidence
interval (95% CI).
Results
Participant characteristics
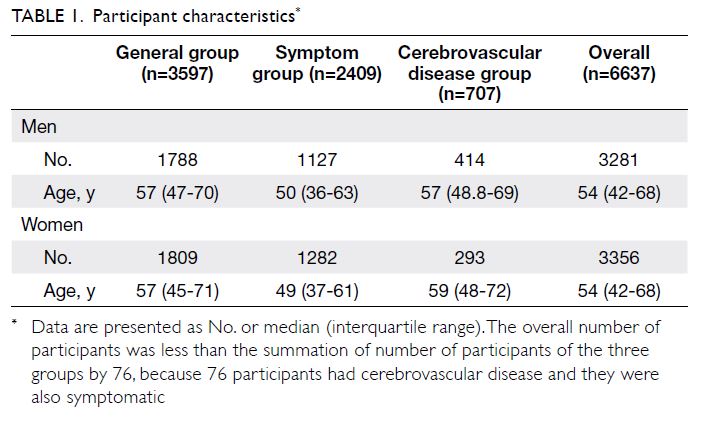
During the study period between July 1994 and
December 2009, 8959 cerebral MRA examinations
were conducted; 97.9% of the examined individuals
were Chinese. Among them, 2252 repeat MRA
examinations and 70 individuals with known history
of ruptured/unruptured aneurysm or a family history
of cerebral aneurysm were excluded (Fig 1). Finally,
first cerebral MRA examinations of 6637 individuals
were included for analysis (Table 1).
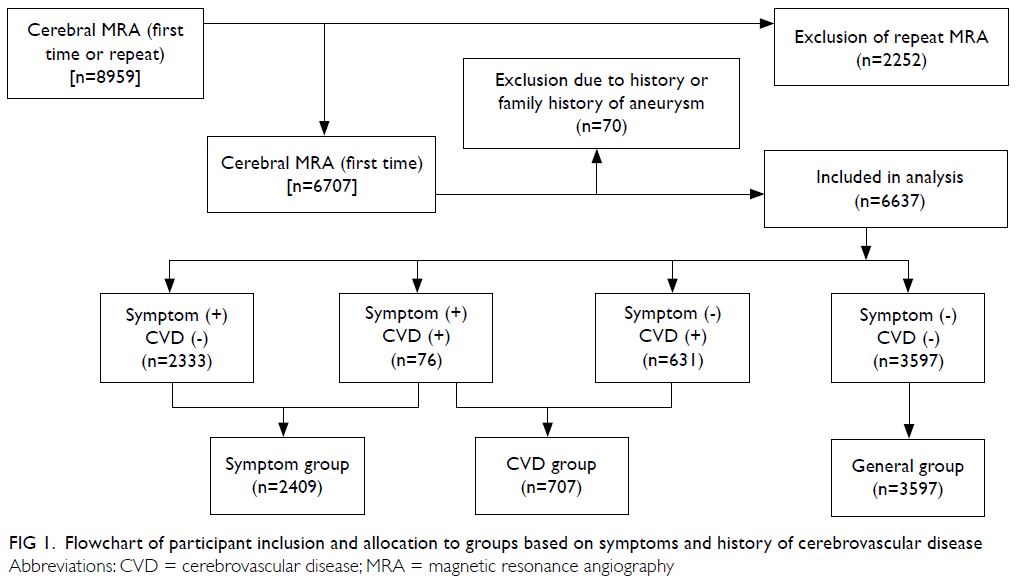
Figure 1. Flowchart of participant inclusion and allocation to groups based on symptoms and history of cerebrovascular disease
Prevalences in the General group, stratified
according to sex and age
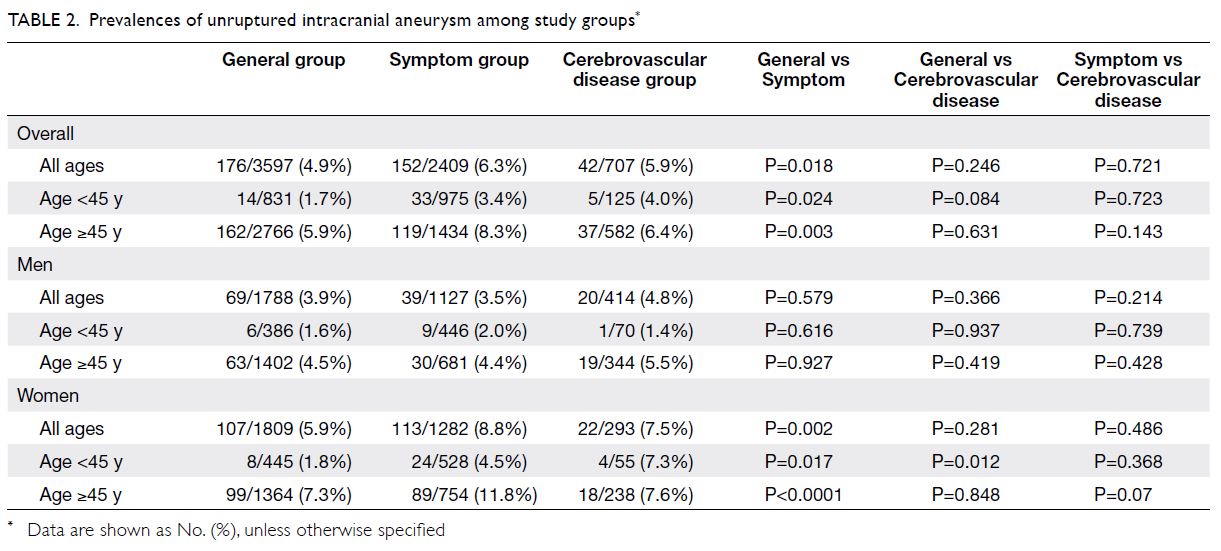
Table 1 shows the prevalences of unruptured
intracranial aneurysm among the study groups. In
the General group, the overall prevalence was 4.9%;
the prevalences in women and men were 5.9% and
3.9%, respectively (P=0.004) [Table 2]. The prevalence
was significantly higher in women than in men for
almost all age ranges; it generally increased with age
(Fig 2). The age threshold with the greatest change
in unruptured intracranial aneurysm prevalence
was 45 years in the General group overall (OR=3.1;
95% CI, 1.9-4.9), among men in the General group
(OR=3.6, 95% CI, 1.6-8.3), and among women in
the General group (OR=2.9, 95% CI, 1.6-5.2). In the
General group overall, as well among men and women
in the General group, the prevalences significantly
differed between participants age <45 years
and participants age ≥45 years (Table 2).
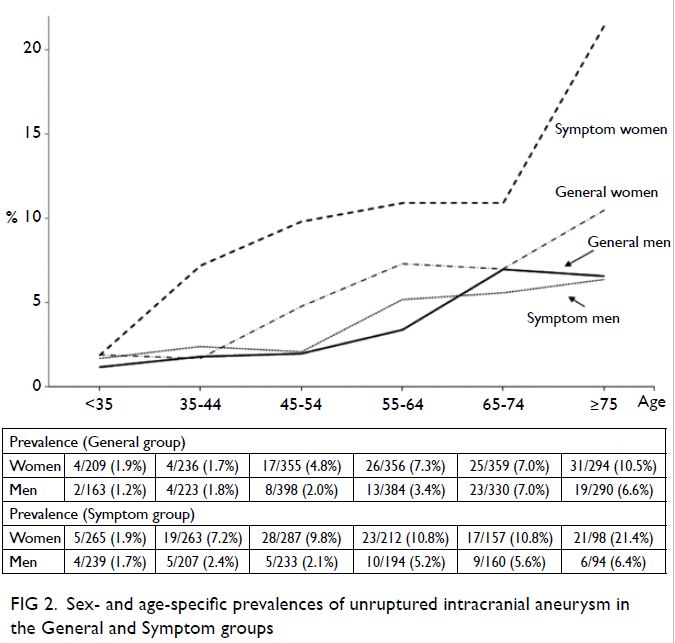
Figure 2. Sex- and age-specific prevalences of unruptured intracranial aneurysm in the General and Symptom groups
Estimation of prevalence in the Hong Kong
population
In the General group, the prevalences of unruptured
intracranial aneurysm in men age <35, 35 to 44,
45 to 54, 55 to 64, 65 to 74 and >74 years were
1.2%, 1.8%, 2%, 3.4%, 7% and 6.6%, respectively;
the corresponding prevalences in women were
1.9%, 1.7%, 4.8%, 7.3%, 7%, and 10.5%, respectively.
Census data for Hong Kong from 2019 indicated
that the numbers of men in the above age ranges
were 1.25 million, 0.4652 million, 0.4896 million,
0.5952 million, 0.3804 million and 0.2514 million,
respectively; the numbers of women in those
age ranges were 1.3542 million, 0.7141 million,
0.6601 million, 0.6404 million, 0.394 million and 0.3262 million, respectively.19 Thus, we estimated
the overall prevalence of unruptured intracranial
aneurysm in the Hong Kong population to be 3.6%.
There were no statistically significant differences in
sex- and age-specific prevalences among participants
examined in the final 5 years of the study, compared
with participants examined throughout the 15.5-year
study period (Table 3).
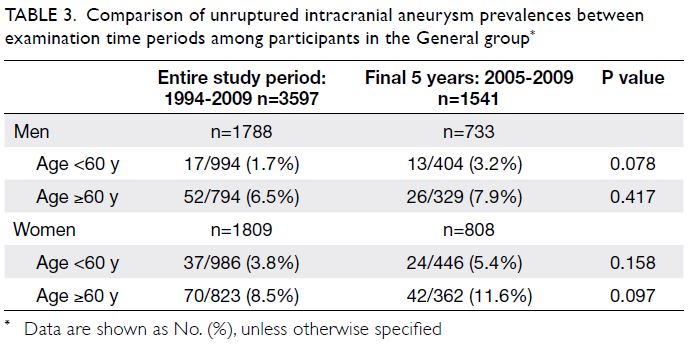
Table 3. Comparison of unruptured intracranial aneurysm prevalences between examination time periods among participants in the General group
Comparison of prevalences between the
General group and the other groups
The unruptured intracranial aneurysm prevalence
was significantly higher in the Symptom group
than in the General group (6.3% vs 4.9%, P=0.018)
[Table 2]. The prevalence was also significantly
higher in the Symptom group than in the General
group among all women participants, participants age <45 years, participants age ≥45 years, women age
<45 years, and women age ≥45 years. Otherwise, the
prevalences of unruptured intracranial aneurysm
did not significantly differ between the General
group (overall or subgroups) and the other main
groups (Table 2).
Comparison of prevalence ratios between
age-range subgroups and between the
General and Symptom groups
Using the prevalence at age 35 to 44 years as the
reference value, the prevalences for the subgroups
of age 45 to 54, 55 to 64 and 65 to 74 years were
2.8-fold, 4.3-fold and 4.1-fold greater than the
reference value, respectively, for women in the General group; these prevalences were 1.1-fold,
1.9-fold and 3.9-fold greater than the reference
value, respectively, for men in the General group.
For the subgroups of age 35 to 44, 45 to 54, 55 to 64
and 65 to 74 years, the prevalence ratios of women
to men were 0.9, 2.4, 2.1 and 1, respectively, in the
General group. Additionally, the prevalence ratios of
the Symptom group to the General group in the four
age subgroups varied from 4.2 to 1.5 for women and
from 1.5 to 0.8 for men (Table 4, Fig 2).
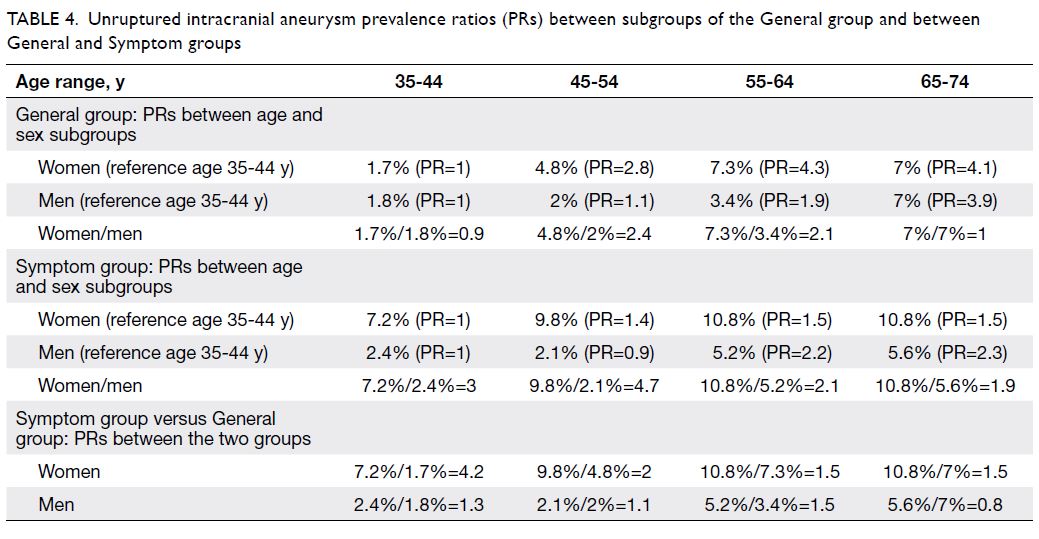
Table 4. Unruptured intracranial aneurysm prevalence ratios (PRs) between subgroups of the General group and between General and Symptom groups
Size and location of unruptured intracranial
aneurysms
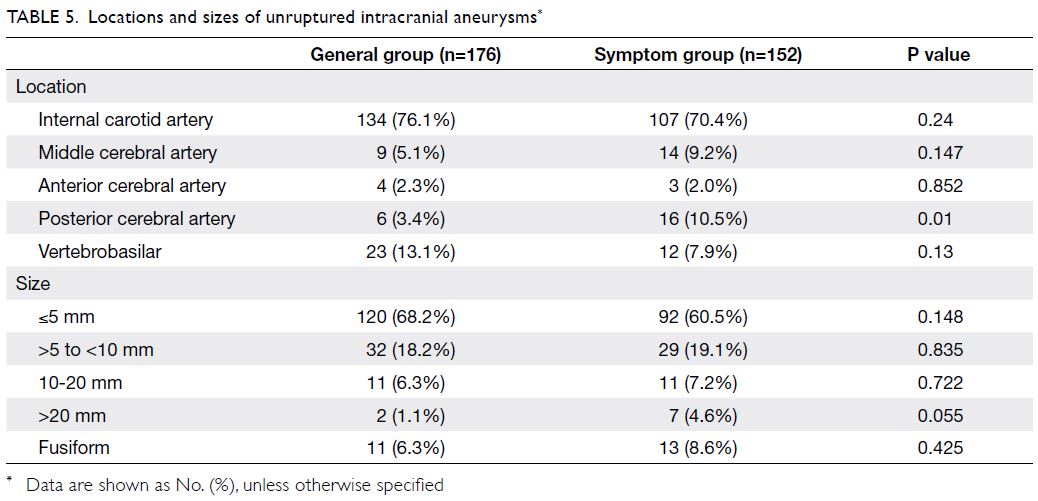
Among 176 participants with one or more aneurysms
in the General group, the largest aneurysm in
each participant was selected for size and location
analysis. Eleven participants (6.3%) had fusiform
aneurysms, while 165 participants (93.8%) had
saccular aneurysms. Furthermore, 157 participants
(89.2%) had a single aneurysm, 16 participants (9.1%)
had two aneurysms, and two participants (1.1%) had
three aneurysms. Mirror aneurysm occurred in six
participants (3.4%): five men and one woman. Mirror
aneurysms were located in the cavernous internal
carotid artery in two participants and in the non-cavernous
internal carotid artery in four participants.
The mirror aneurysms were bilaterally symmetrical;
they measured ≤5 mm (four participants), 5-10 mm
(one participant), and 10-20 mm (one participant).
The size and location distributions of aneurysms
in the General and Symptom groups are shown in
Table 4. The proportion of posterior cerebral artery
aneurysms was significantly greater in the Symptom
group than in the General group (10.5% vs 3.4%,
P=0.01) [Table 5].
Discussion
It is resource-intensive to determine the unruptured
intracranial aneurysm prevalence in any population
because of the need for large-scale studies with
prospective and random selection of participants, as
well as the utilisation of accurate diagnostic means for
aneurysm detection. To achieve this objective within
the constraints of a hospital-based retrospective
study, our study model used a hospital that served the
whole population of Hong Kong; study participants
comprised individuals without a family history,
past history, or symptoms related to intracranial
aneurysms, all of whom were referred to the hospital
for body check with MRA. These individuals were
assumed to be closely representative of a random
sample of the Hong Kong population because
there was no identifiable medical reason when they
presented themselves to a doctor, therefore the
sample was not biased. Because the prevalence of
unruptured intracranial aneurysm is sex- and age-dependent,
11 the overall prevalence is dependent on the sex and age composition of participants in the
study sample. Sex- and age-specific prevalences are
more meaningful than overall prevalences because
they allow comparisons among distinct target groups
in the same study and in other studies. The analysis
of unruptured intracranial aneurysm prevalence in
individuals with symptoms and individuals with a
known history of CVD provides useful information
for physicians who must counsel such patients.
Studies of intracranial aneurysm prevalence
have multiple limitations. Retrospective studies
tend to show lower prevalence rates than do
prospective studies.4 13 20 21 22 Prevalences vary
according to the modality of aneurysm detection,
such that prevalence rates tend to be much lower in autopsy studies than in arteriogram studies or
MRA studies. Published prevalences have been
0.4% to 0.5% in retrospective autopsy studies,4 3.1%
to 4.1% in prospective autopsy studies,4 0.65% to
4.4% in retrospective arteriogram studies,4 3% to
6.8% in prospective arteriogram studies,4 3.2% to
4.3% in retrospective MRA studies,21 22 and 5% to
7% in prospective MRA studies.13 14 The overall
prevalences are also limited by the sex and age
compositions of participants in each study. Autopsy
and hospital-based retrospective studies usually
have biased samples comprising individuals who
presented to the hospital with clinical indications for
investigation. Furthermore, the identification of an
intracranial aneurysm at autopsy is greatly affected by the interest and enthusiasm of the examiner23;
intracranial aneurysms are commonly overlooked
at autopsy.24 These observations may explain the
generally low prevalence rates of 0.2% to 2.2%
reported in autopsy studies.6 25 26 27
Unruptured intracranial aneurysms are
more common in women and relatively older
individuals.4 11 14 21 Comparisons of unruptured
intracranial aneurysm prevalence between published
studies may not be meaningful without considering
the sex ratio and age distribution of the study samples;
such comparisons are not feasible for studies in which
sex ratio and age distribution data are unavailable,
and such studies are not uncommon. We compared
our results with findings from a prospective study of
Chinese individuals in Shanghai,14 in which the sex- and
age-specific prevalences had been analysed; both
studies shared some common trends. In the previous
study, the overall prevalence was 7%; moreover,
prevalence increased with age and the female-to-male
prevalence ratio decreased with increasing age.
These prevalence patterns were similar to patterns
observed in the current study. Notably, the age- and
sex-specific prevalences were consistently higher
in the Shanghai study14 than in the current study,
which suggests differences in intracranial aneurysm
prevalence between the two populations.
There were two main limitations in this study.
First, its duration (15 years) was relatively long.
Although there were prevalence studies which
involved cerebral arteriogram or autopsy lasting for
up to 11 years or 30 years respectively,6 20 studies
involving MRA typically lasted for 2 to 4 years.14 21
However, the results obtained from the long study
period can be regarded as similar to the aggregate
results of a series of consecutive short retrospective
studies. The overall age- and sex-specific prevalences
obtained during the long study period can be
regarded as the average value of age- and sex-specific
prevalences in the individual shorter studies. A
major concern related to a long study period is the
potential for variations in population demographics,
particularly with respect to age and sex. Because
analyses of age- and sex-specific prevalence were
conducted in the present study, variations in age
and sex composition throughout the population in
various time periods were presumed not to affect
the analysis outcome. The overall prevalence of a
particular disease at any time point can be calculated
from the sex and age composition of the population
at that particular time point, together with the age- and
sex-specific prevalences of that disease. Many
published studies report an overall prevalence, which
is meaningful only for a specific time period because
it is dependent on the age and sex composition of
the population during the study period. Age- and
sex-specific prevalences are more meaningful than
an overall prevalence, they could be regarded as part of the natural process of the disease specific
to the population and are expected to exhibit fewer
changes over time, therefore, they are more directly
applicable to clinical practice. Consistent with that
expectation, we found no statistically significant
differences in age- and sex-specific prevalences in
the final 5 years of the study period, compared with
the study period overall.
Second, the assumption that the General group
is a close representative of the general population
in Hong Kong requires validation because certain
factors associated with high aneurysm risk may
be more common among individuals referred for
examination via MRA. Based on the selection
criteria for the General group, selection bias may
have caused this group to be poorly representative of
the general population in Hong Kong. To minimise
the potential for such bias, factors associated with a
high risk of cerebral aneurysm were addressed by the
exclusion of individuals with a family history, past
history, or symptoms related to cerebral aneurysm.
Additionally, the proportions of individuals with
hypertension and a smoking habit in the General
group did not significantly differ from those
proportions in the wider Hong Kong population.
Finally, potential biases involving advanced age and
female sex were addressed with age- and sex-specific
analyses.
In conclusion, the estimated overall prevalence
of unruptured intracranial aneurysm in the Hong
Kong population was 3.6%. The prevalence was
significantly higher in the Symptom group than
in the General group. However, the unruptured
intracranial aneurysm prevalences did not differ
between the General and CVD groups, or between
the Symptom and CVD groups.
Author contributions
Concept or design: SCH Yu.
Acquisition of data: PW Cheng, GE Antonio, HTG Ma, SCC Chan.
Analysis or interpretation of data: SCH Yu, TWW Lau, SCC Chan.
Drafting of the manuscript: SCH Yu, PW Cheng.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: PW Cheng, GE Antonio, HTG Ma, SCC Chan.
Analysis or interpretation of data: SCH Yu, TWW Lau, SCC Chan.
Drafting of the manuscript: SCH Yu, PW Cheng.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
The authors declare that they have no conflict of interest.
Acknowledgement
The authors thank the following individuals for substantial contributions to data interpretation and manuscript revision:
HKM Cheng, BMH Lai, GKC Wong, VKY Pang, ACO Tsang,
DPH Wong, KM Leung, R Lee, TKT Chan, and CB Tan.
Funding/support
This study was funded by the Vascular and Interventional
Radiology Foundation. The funding body had no involvement
in the design of the study; in the collection, analysis, and
interpretation of data; or in writing the manuscript.
Ethics approval
This study was approved by the Chinese University of Hong Kong–New Territories East Cluster Clinical Research Ethics
Committee (CRE-2010-381). The requirement for informed
consent was waived owing to the retrospective nature of the
study.
References
1. Brown RD. Unruptured intracranial aneurysms. Semin Neurol 2010;30:537-44. Crossref
2. Graves EJ. Detailed diagnoses and procedures, national hospital discharge survey, 1990. Vital Health Stat 13
1992;113:1-225.
3. Ujiie H, Sato K, Onda H, et al. Clinical analysis of incidentally discovered unruptured aneurysms. Stroke
1993;24:1850-6. Crossref
4. Rinkel GJ, Djibuti M, Algra A, van Gijn J. Prevalence and risk of rupture of intracranial aneurysms: a systematic
review. Stroke 1998;29:251-6. Crossref
5. International Study of Unruptured Intracranial Aneurysms Investigators. Unruptured intracranial aneurysms—risk of rupture and risks of surgical intervention. N Engl J Med
1998;339:1725-33. Crossref
6. Iwamoto H, Kiyohara Y, Fujishima M, et al. Prevalence
of intracranial saccular aneurysms in a Japanese
community based on a consecutive autopsy series during
a 30-year observation period. The Hisayama study. Stroke
1999;30:1390-5. Crossref
7. Katzman GL, Dagher AP, Patronas NJ. Incidental
findings on brain magnetic resonance imaging from 1000
asymptomatic volunteers. JAMA 1999;282:36-9. Crossref
8. Wardlaw JM, White PM. The detection and management of unruptured intracranial aneurysms. Brain 2000;123:205-21. Crossref
9. Horikoshi T, Akiyama I, Yamagata Z, Nukui H. Retrospective analysis of the prevalence of asymptomatic
cerebral aneurysm in 4518 patients undergoing magnetic
resonance angiography—when does cerebral aneurysm
develop? Neurol Med Chir (Tokyo) 2002;42:105-12. Crossref
10. Vernooij MW, Ikram MA, Tanghe HL, et al. Incidental findings on brain MRI in the general population. N Engl J
Med 2007;357:1821-88. Crossref
11. Vlak MH, Algra A, Brandenburg R, Rinkel GJ. Prevalence of
unruptured intracranial aneurysms, with emphasis on sex,
age, comorbidity, country, and time period: a systematic
review and meta-analysis. Lancet Neurol 2011;10:626-36. Crossref
12. Agarwal N, Gala NB, Choudhry OJ, et al. Prevalence of
asymptomatic incidental aneurysms: a review of 2685
computed tomographic angiograms. World Neurosurg
2014;82:1086-90. Crossref
13. Chan DY, Abrigo JM, Cheung TC, et al. Screening for
intracranial aneurysms? Prevalence of unruptured
intracranial aneurysms in Hong Kong Chinese. J Neurosurg
2016;124:1245-9. Crossref
14. Li MH, Chen SW, Li YD, et al. Prevalence of unruptured
cerebral aneurysms in Chinese adults aged 35 to 75 years: a
cross-sectional study. Ann Intern Med 2013; 159:514-21. Crossref
15. Igase K, Matsubara I, Igase M, Miyazaki H, Sadamoto K.
Initial experience in evaluating the prevalence of
unruptured intracranial aneurysms detected on 3-Tesla
MRI. Cerebrovasc Dis 2012;33:348-53. Crossref
16. Li MH, Cheng YS, Li YD, et al. Large-cohort comparison
between three-dimensional time-of-flight magnetic
resonance and rotational digital subtraction angiographies
in intracranial aneurysm detection. Stroke 2009;40:3127-9. Crossref
17. Li MH, Li YD, Tan HQ, Gu BX, et al. Contrast-free MRA
at 3.0 T for the detection of intracranial aneurysms.
Neurology 2011;77:667-76. Crossref
18. T Dill. Contraindications to magnetic resonance imaging.
Heart 2008;94:943-8. Crossref
19. Census and Statistics Department, Hong Kong SAR
Government. Available from: www.censtatd.gov.hk/en/web_table.html?id=1A. Accessed 18 Sep 2020.
20. Winn HR, Jane JA Sr, Taylor J, Kaiser D, Britz GW. Prevalence of asymptomatic incidental aneurysms: review
of 4568 arteriograms. J Neurosurg 2002;96:43-9. Crossref
21. Harada K, Fukuyama K, Shirouzu T, et al. Prevalence
of unruptured intracranial aneurysms in healthy
asymptomatic Japanese adults: differences in gender and
age. Acta Neurochir (Wien) 2013;155:2037-43. Crossref
22. Imaizumi Y, Mizutani T, Shimizu K, Sato Y, Taguchi J.
Detection rates and sites of unruptured intracranial
aneurysms according to sex and age: an analysis of MR
angiography–based brain examinations of 4070 healthy
Japanese adults. J Neurosurg 2018;130:573-8. Crossref
23. Chason JL, Hindman WM. Berry aneurysms of the circle
of Willis; results of a planned autopsy study. Neurology
1958,8:41-4. Crossref
24. Stehbens WE. Aneurysms and anatomical variation of cerebral arteries. Arch Pathol 1963;75:45-64.
25. Housepian EM, Pool JL. A systematic analysis of
intracranial aneurysms from the autopsy file of the
Presbyterian Hospital, 1914 to 1956. J Neuropathol Exp
Neurol 1958,17:409-23. Crossref
26. McCormick WF, Nofzinger JD. Saccular intracranial aneurysms: an autopsy study. J Neurosurg 1965;22:155-9. Crossref
27. Inagawa T, Hirano A. Autopsy study of unruptured incidental intracranial aneurysms. Surg Neurol 1990;34:361-5. Crossref