Hong Kong Med J 2021 Dec;27(6):461–3 | Epub 17 Dec 2021
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
COMMENTARY
Critically ill children in paediatric intensive care unit are no less susceptible to infectious diseases amid the COVID-19 pandemic
Karen KY Leung, MB, BS, MRCPCH1; KL Hon, MB, BS, MD1; Patrick Ip, MB, BS, MD2; Renee WY Chan, PhD3,4,5,6
1 Paediatric Intensive Care Unit, Department of Paediatrics and Adolescent Medicine, The Hong Kong Children’s Hospital, Hong Kong
2 Department of Paediatrics and Adolescent Medicine, The University of Hong Kong, Hong Kong
3 Department of Paediatrics, The Chinese University of Hong Kong, Hong Kong
4 Hong Kong Hub of Paediatric Excellence, The Chinese University of Hong Kong, Hong Kong
5 Laboratory for Paediatric Respiratory Research, Li Ka Shing Institute of Health Sciences, The Chinese University of Hong Kong, Hong Kong
6 CUHK-UMCU Joint Research Laboratory of Respiratory Virus & Immunobiology, Department of Paediatrics, The Chinese University of Hong Kong, Hong Kong
Corresponding author: Dr KL Hon (ehon@hotmail.com)
With the lifting of various measures intended to limit
the spread of coronavirus disease 2019 (COVID-19),
paediatric cases have been on the rise, with
approximately 2% to 6% of those infected becoming
critically ill.1 2 3 4 5 6 During the early phase of the
pandemic, a review of 2135 paediatric cases in China
revealed the proportion of severe and critical illness
to be higher in the younger age-group, in particular
infants.5 In a separate report by the United States
Centers for Disease Control and Prevention, 62%
of those aged <1 year were hospitalised compared
with 4.1% to 14% among those aged 1 to 17 years.6
However as the pandemic evolves, the epidemiology
seems to have changed and COVID-19 is now
affecting older children more severely. In the latest
report from the United States, critically ill children
with COVID-19 were predominantly adolescents,
had co-morbidities, and required some form of
respiratory support.7 In many cases, the presence of
acute respiratory distress syndrome was associated
with prolonged paediatric intensive care (PICU) and
hospital stay.8
Recently there has been an emergence of
paediatric hyperinflammatory and shock syndromes
including paediatric inflammatory multisystem
syndrome (PIMS), MIS-C (multisystem inflammatory
syndrome in children), and PIMS-TS (paediatric
inflammatory multisystem syndrome temporally
associated with severe acute respiratory syndrome
coronavirus 2 [SARS-CoV-2]).9 10 These are systemic
diseases involving persistent fever, inflammation and
organ dysfunction associated with SARS-CoV-2;
80% of the patients with this new disease entity
require intensive care support with a 2% fatality
rate.3 11 12 13 Furthermore, COVID-19 is associated with
dysfunction across many organ systems as in PIMS as
well as syndromes such as COVID stress syndrome
and COVID toe syndrome.14
Unlike other respiratory viruses such as
influenza and respiratory syncytial virus, there
has fortunately been no paediatric mortality due
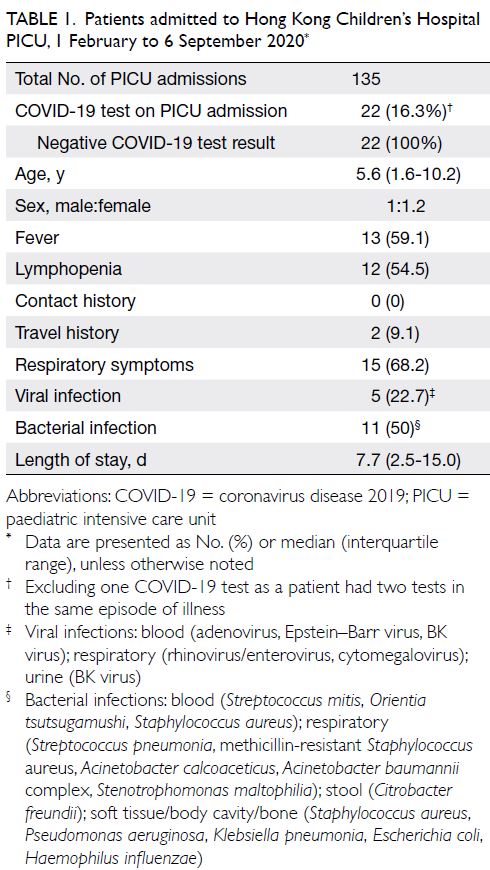
to COVID-19 in Hong Kong. We reviewed all
admissions to the Hong Kong Children’s Hospital
PICU with nasal pharyngeal swab/aspiration for
SARS-CoV-2 between 1 February and 6 September
2020, and found that 22 (16.3%) of our admitted
patients were tested and they were all negative for
COVID-19 (Table 1). During the early stages of
the COVID-19 epidemic in Hong Kong, screening
for COVID-19 was not universal for all PICU
admissions; only patients meeting set criteria were
screened, primarily in-patients, patients acutely
admitted, or patients transferred in who had not
already been tested. Patients who had been tested
negative elsewhere or in-patients with no exposure
were not tested in the initial phase of the pandemic.
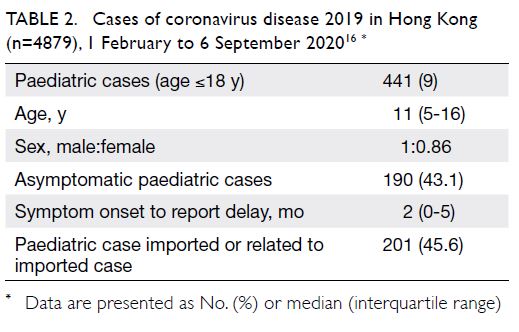
During the same period, there were 441 (9%) of
COVID-19 cases in Hong Kong were aged ≤18 years
(Table 2 15). In addition to SARS-CoV-2, various
viral and bacterial pathogens were isolated in these
paediatric patients with COVID-19. Viruses isolated
include adenovirus, Epstein-Barr virus, and BK
virus in blood samples; rhinovirus, enterovirus, and
cytomegalovirus in respiratory specimens; and BK
virus in urine samples. A wide variety of bacteria were
also isolated, including a case of hyperinflammatory
hemophagocytic lymphohistiocytosis syndrome due
to Orientia tsutsugamushi instead of SARS-CoV-2.
Compared with paediatric patients with SARS-CoV-2
in the community, viral and bacterial infections were
present in 22.7% and 50% of SARS-CoV-2 negative
patients in our PICU cohort, respectively (P<0.001).
The COVID-19 screening criteria changed as the
pandemic evolved and it is now mandatory to screen
every patient admitted to the PICU for COVID-19.
In our opinion, it is unlikely that PICUs in Hong Kong have missed any cases of COVID-19.
During the pandemic, it is easy to overestimate
the prevalence of COVID-19 due to cognitive bias,
and assume all patients with fever are infected
with COVID-19 until proven otherwise, leading
to potential therapeutic errors.16 However, our
observations have concluded that critically ill children are susceptible to contracting a whole host
of infectious diseases. Therefore, in addition to
screening for COVID-19, physicians must also be
vigilant of other pathogens that could affect critically
ill children, and duly take antimicrobial and isolation
precautions within healthcare environments. It
appears that SARS-CoV-2 infection is generally an
asymptomatic or very mild disease in children. In
contrast, serious viral and bacterial infections are
associated with critically ill children tested negative
for SARS-CoV-2.
Author contributions
All authors contributed to the concept or design, acquisition of data, analysis or interpretation of data, drafting of the
manuscript, and critical revision of the manuscript for
important intellectual content. All authors had full access to
the data, contributed to the study, approved the final version
for publication, and take responsibility for its accuracy and
integrity.
Conflicts of interest
As the editor of the journal, KL Hon was not involved in the peer review process for the article. Other authors have no
conflicts of interest to disclose.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. Hon KL, Leung KK. Paediatrics is a big player of COVID-19 in Hong Kong [Letter]. Hong Kong Med J
2020;26:265-6. Crossref
2. Hon KL, Leung KK. Pediatric COVID-19: what disease is this? World J Pediatr 2020;16:323-5. Crossref
3. Hon KL, Leung KK, Leung AK, et al. Overview: the history
and pediatric perspectives of severe acute respiratory
syndromes: novel or just like SARS. Pediatr Pulmonol
2000;55:1584-91. Crossref
4. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020;323:1239-42. Crossref
5. Dong Y, Mo X, Hu Y, et al. Epidemiology of COVID-19 among children in China. Pediatrics 2020;145:e20200702. Crossref
6. CDC COVID-19 Response Team. Coronavirus Disease 2019 in children—United States, February 12-April 2,
2020. MMWR Morb Mortal Wkly Rep 2020;69:422-6. Crossref
7. Derespina KR, Kaushik S, Plichta A, et al. Clinical manifestations and outcomes of critically ill children and
adolescents with Coronavirus Disease 2019 in New York
City. J Pediatr 2020;226:55-63.e2. Crossref
8. Pathak EB, Salemi JL, Sobers N, Menard J, Hambleton IR.
COVID-19 in children in the United States: intensive
care admissions, estimated total infected, and projected
numbers of severe pediatric cases in 2020. J Public Health
Manag Pract 2020;26:325-33. Crossref
9. Joshi K, Kaplan D, Bakar A, et al. Cardiac dysfunction and shock in pediatric patients with COVID-19. JACC Case Rep 2020;2:1267-70. Crossref
10. Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during
COVID-19 pandemic. Lancet 2020;395:1607-8. Crossref
11. Feldstein LR, Rose EB, Horwitz SM, et al. Multisystem inflammatory syndrome in U.S. Children and Adolescents.
N Engl J Med 2020;383:334-6. Crossref
12. Paediatric Intensive Care Society. PICS Statement:
increased number of reported cases of novel presentation
of multi system inflammatory disease. 2020. Available from:
https://pccsociety.uk/wp-content/uploads/2020/04/PICS-statement-re-novel-KD-C19-presentation-v2-27042020.pdf. Accessed 25 Sep 2020.
13. The Royal College of Paediatrics and Child Health. Paediatric multisystem inflammatory syndrome temporally associated with COVID-19 (PIMS)—guidance
for clinicians. 2020. Available from: https://www.rcpch.ac.uk/resources/paediatric-multisystem-inflammatory-syndrome-temporally-associated-covid-19-pims-guidance. Accessed 25 Sep 2020.
14. Rose-Sauld S, Dua A. COVID toes and other cutaneous manifestations of COVID-19. J Wound Care 2020;29:486-7. Crossref
15. Centre for Health Protection, Hong Kong SAR
Government. Latest situation of cases of COVID-19 (as
of 24 September 2020). 2020. Available from: https://www.chp.gov.hk/files/pdf/local_situation_covid19_en.pdf. Accessed 24 Sep 2020.
16. Zagury-Orly I, Schwartzstein RM. Covid-19—A reminder to reason. N Engl J Med 2020;383:e12. Crossref