Hong Kong Med J 2021 Dec;27(6):456.e1–2
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Cullen sign in childhood malignancies
CC Au, MB, BS, MRCPCH1; Karen KY Leung, MB, BS, MRCPCH1; KL Hon, MB, BS, MD1; Junita KY Tung2; Carol LS Yan, MB, BS, MRCPCH1; WF Hui, MB, BS, MRCPCH1; WY Leung, MB, ChB, FRCSEd(Paed)3
1 Department of Paediatrics and Adolescent Medicine, The Hong Kong Children’s Hospital, Hong Kong
2 Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong
3 Department of Surgery, The Hong Kong Children’s Hospital, Hong Kong
Corresponding author: Dr CC Au (aucc@ymail.com)
Introduction
We report four consecutive cases of young children
with Cullen sign in a paediatric intensive care unit
with abdominal malignancies and complications due
to treatment. Two children had solid tumours with
hepatic rupture and two had pancreatitis secondary
to asparaginase use for leukaemia.
Case 1
A 23-month-old boy with ruptured liver metastasis
and stage 4 neuroblastoma presented with abdominal
distension due to a large retroperitoneal mass
invading the liver and encasing the aorta and inferior
vena cava. He required emergency laparotomy for
haemorrhagic shock due to ruptured liver metastasis
and endovascular embolisation of tumoural arteries.
Subsequently there was an extensive subcutaneous
haematoma around the surgical wound. Cullen
sign was detected (Fig 1). Recurrent tumoural
haemorrhage was excluded and surgical exploration
performed to remove blood clots.
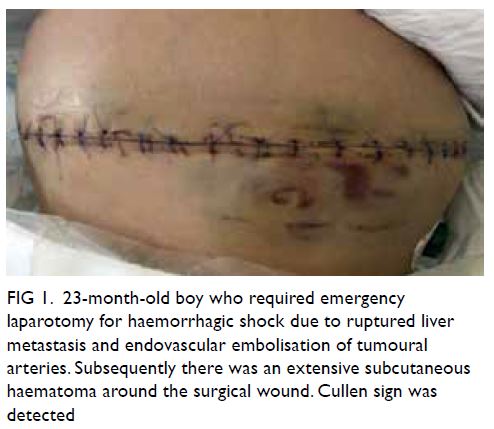
Figure 1. 23-month-old boy who required emergency laparotomy for haemorrhagic shock due to ruptured liver metastasis and endovascular embolisation of tumoural arteries. Subsequently there was an extensive subcutaneous haematoma around the surgical wound. Cullen sign was detected
Case 2
A 5-year-old girl had asparaginase-associated
pancreatitis and common B-cell acute lymphoblastic
leukaemia. She was 6 months into her treatment
protocol and received re-induction phase
chemotherapy including pegaspargase (Oncaspar).
She presented with abdominal pain and vomiting due
to severe acute necrotising pancreatitis. Cullen sign
(peri-umbilicus), Grey Turner sign (flank), and Fox
sign (inguinal ligament) were detected (Fig 2). She required vasopressor and non-invasive ventilation
for systemic inflammatory response syndrome.
She later developed pancreatic pseudocyst and
underwent ultrasound-guided drainage.

Figure 2. 5-year-old girl presented with abdominal pain and vomiting due to severe acute necrotising pancreatitis. Cullen sign (peri-umbilicus), Grey Turner sign (flank), and Fox sign (inguinal ligament) were detected
Case 3
A 5-year-old boy with asparaginase-associated
pancreatitis and B-cell acute lymphoblastic leukaemia
had received re-induction phase chemotherapy
with pegaspargase (Oncaspar) and presented with
abdominal pain and vomiting. He had severe acute
necrotising pancreatitis and systemic inflammatory
response syndrome. Cullen sign (peri-umbilicus)
and Bryant sign (scrotum) were detected (Fig 3). He
required vasopressor support. Later he developed
multiple intrapancreatic and peripancreatic fluid
collections and required repeated computed
tomography-guided aspiration and drainage.

Figure 3. 5-year-old boy presented with abdominal pain and vomiting due to severe acute necrotising pancreatitis and systemic inflammatory response syndrome. Cullen sign (peri-umbilicus) and Bryant sign (scrotum) were detected
Case 4
A 7-year-old boy with ruptured hepatoblastoma
presented with abdominal distension.
Hepatoblastoma involved all liver segments,
extended into the inferior vena cava and had
metastasised to the lungs. He required selective
embolisation of left hepatic artery segments 2
and 3 for active haemorrhage. He had abdominal
compartment syndrome and gross ascites that
required drainage. Cullen sign was detected. (Fig 4)
He was prescribed chemotherapy and consequently
the tumour reduced in size.

Figure 4. 7-year-old boy with abdominal compartment syndrome and gross ascites that required drainage. Cullen sign was detected
Discussion
These four cases illustrate Cullen sign in
paediatric malignancies. General practitioners and
paediatricians should be aware of its diagnostic
implications during clinical examination.
First described in 1918, Cullen sign referred
to periumbilical ecchymosis due to retroperitoneal
haemorrhage of ruptured ectopic pregnancy.1 It has
become one of the classic abdominal signs in acute
pancreatitis. Cullen sign or Grey Turner sign has
been reported present in 3% of acute necrotising
pancreatitis cases. In 1984, these signs were reported
to have a significant mortality rate of 37%,2 but
clinical outcomes of severe acute pancreatitis have
since improved with intensive care. Nevertheless
Cullen sign remains a pointer to serious intra-abdominal
haemorrhage. Haemorrhage can
originate anywhere along an anatomical pathway.
Pathophysiologically, blood tracks from the
retroperitoneum through the gastrohepatic ligament
to the falciform ligament of the liver, then reaches the umbilicus through the round ligament of liver to
form Cullen sign.3 Cullen sign has been reported in
intra-abdominal malignancies, liver cirrhosis, and
rectus sheath haematoma.4 5
Author contributions
All authors contributed to the concept or design of the study, interpretation of the data, drafting of the manuscript, and
critical revision of the manuscript for important intellectual
content. All authors had full access to the data, contributed to
the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, KL Hon was not involved in the peer review process for this article. Other authors have no
conflicts of interest to disclose.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patients were treated in accordance with the Declaration of Helsinki. This study was approved by the Hong Kong
Children’s Hospital Research Ethics Committee (Ref HKCH-REC-2019-009). Patients’ parents consented for publication of
clinical photographs.
References
1. Cullen TS. A new sign in ruptured extrauterine pregnancy. Am J Obstet Gynecol 1918;78:457.
2. Dickson AP, Imrie CW. The incidence and prognosis of body wall ecchymosis in acute pancreatitis. Surg Gynecol
Obstet 1984;159:343-7.
3. Bem J, Bradley EL 3rd. Subcutaneous manifestations of severe acute pancreatitis. Pancreas 1998;16:551-5. Crossref
4. Mabin TA, Gelfand M. Cullen’s sign, a feature in liver disease. Br Med J 1974;1:493-4. Crossref
5. Harris S, Naina HV. Cullen’s sign revisited. Am J Med 2008;121:682-3. Crossref

