© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Custom-made double inner-branched aortic arch endograft for the treatment of mycotic aortic arch aneurysm: a case report
Benien JP Hau, BBiomed, MB, BS; YC Chan, MD, FRCS; Stephen W Cheng, MS, FRCS
Division of Vascular and Endovascular Surgery, Department of Surgery, Queen Mary Hospital, The University of Hong Kong, Hong Kong
Corresponding author: Dr YC Chan (ycchan88@hkucc.hku.hk)
Case report
A 76-year-old frail man was admitted to hospital
with fever and delirium. His medical history was
significant for diabetes mellitus, hypertension, and
dyslipidaemia. White blood cell count was 9.3 × 109/L
and C-reactive protein 18.20 mg/dL. Blood cultures
yielded serogroup D Salmonella enteritidis.
Computed tomography (CT) angiogram showed
an aortic arch aneurysm of 4.7 cm (Fig 1a). Gallium
scintiscan confirmed focal uptake at the proximal
aortic arch. He developed progressively worsening
chest discomfort for the subsequent 3 weeks, and
a new CT angiogram showed rapid increase in the
aneurysm size to 5.3 cm (Fig 1b).
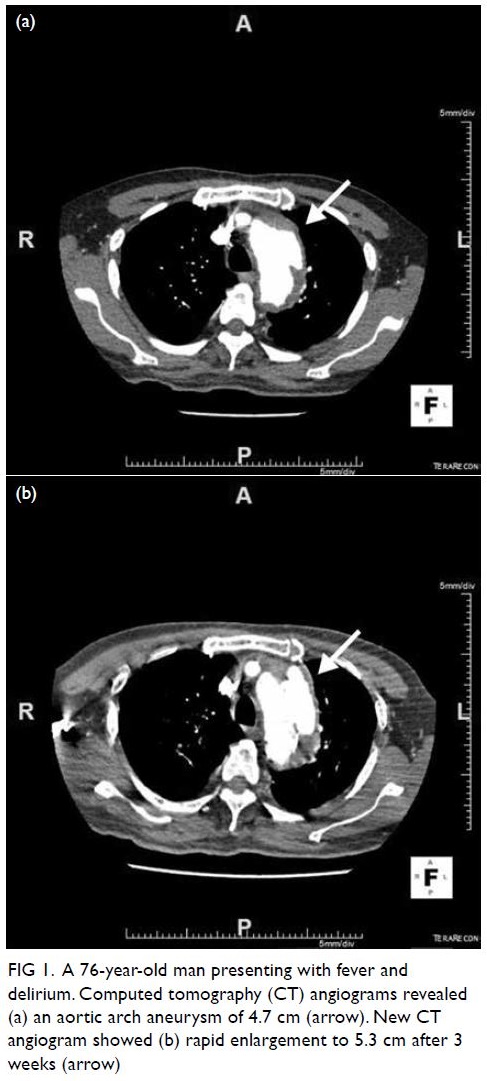
Figure 1. A 76-year-old man presenting with fever and delirium. Computed tomography (CT) angiograms revealed (a) an aortic arch aneurysm of 4.7 cm (arrow). New CT angiogram showed (b) rapid enlargement to 5.3 cm after 3 weeks (arrow)
A diagnosis of mycotic aortic arch aneurysm was
made, and multidisciplinary consultation concluded
that he was too frail to undergo conventional open
repair. A custom-made double inner-branched
aortic arch endograft (Cook Medical, Bloomington
[IN], US) was arranged. During the interim, he
received intravenous ceftriaxone. The left subclavian
artery was revascularised with a left common carotid
artery (CCA) to left subclavian artery bypass as a
first-stage procedure. The custom-made endograft
was available 3 weeks later (Figure 2a,b) and the
endovascular procedure was performed accordingly.
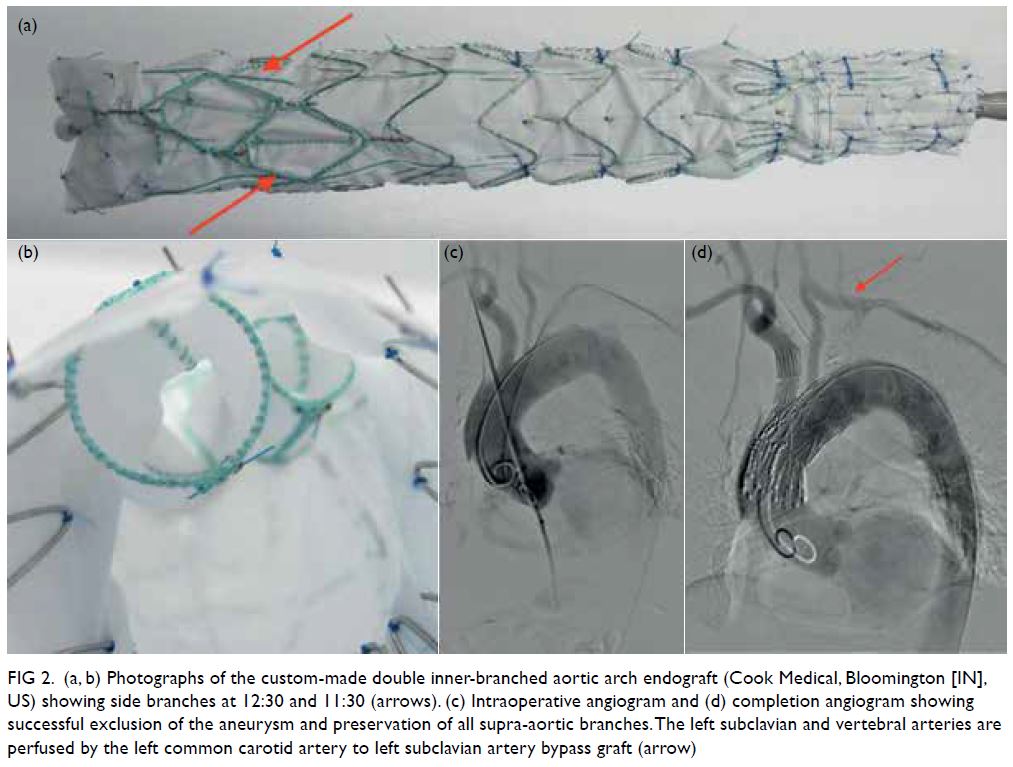
Figure 2. (a, b) Photographs of the custom-made double inner-branched aortic arch endograft (Cook Medical, Bloomington [IN], US) showing side branches at 12:30 and 11:30 (arrows). (c) Intraoperative angiogram and (d) completion angiogram showing successful exclusion of the aneurysm and preservation of all supra-aortic branches. The left subclavian and vertebral arteries are perfused by the left common carotid artery to left subclavian artery bypass graft (arrow)
Briefly, all procedures were performed under
general anaesthesia in a well-equipped hybrid
operating room by experienced endovascular
surgeons. The endografts were flushed with
heparinised saline multiple times to completely
evacuate trapped gas in the sheath. Access was
gained through an open groin cutdown exposing the
common femoral artery and vein, and bilateral neck
cutdowns to expose the right and left CCA. After
full systemic heparinisation and under fluoroscopic
guidance, a Terumo wire and pigtail catheter were
positioned in the left ventricle and exchanged for
a double-curved extended Lunderquist Extra-Stiff
Wire (Cook Medical). The main stent graft body
was then delivered to the aortic arch. The branched
endograft was deployed under fluoroscopy, with
controlled systolic hypotension by an inferior vena
cava occlusion balloon (Coda 46 mm balloon; Cook
Medical) introduced via the right femoral vein. Accurate alignment of the orientation markers with
the coronary and supra-aortic vessels was essential.
After deployment of the main stent graft, the proximal inner branch was sequentially cannulated
in a retrograde fashion through the exposed carotid
arteries. A custom-made thoracic stent graft
extension was used (Cook Medical) to bridge the
proximal inner branch and the innominate artery. A
similar procedure was repeated for the distal inner
branch via the left carotid artery, where a Fluency
self-expanding covered stent (CR Bard, Murray
Hill [NJ], US) was used to bridge the distal inner
branch and the left CCA, taking care not to cover
the left CCA to left subclavian artery bypass. The left
subclavian artery origin was finally occluded with
an Amplatzer vascular plug (St Jude Medical, Saint
Paul [MN], US) to prevent endoleak into the sac.
Completion angiogram showed successful exclusion
of the aneurysm with patent supra-aortic branches
(Fig 2c,d).
The patient recovered well without neurological
sequelae. He was discharged on postoperative
day 13 with lifelong oral ciprofloxacin prescribed.
Computed tomography angiogram at 3 months
(Fig 3a,b) and 1 year (Fig 3c,d) after surgery showed
successful and durable results.
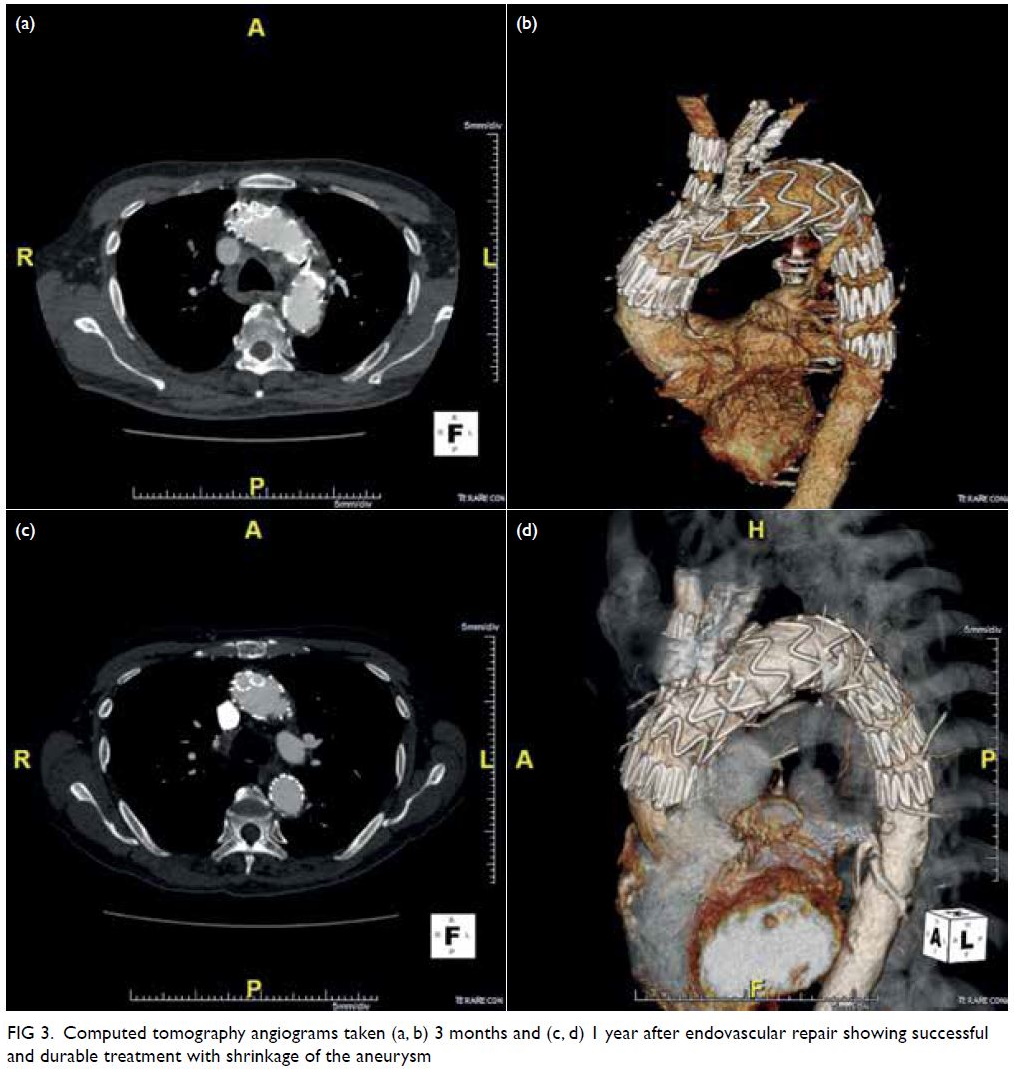
Figure 3. Computed tomography angiograms taken (a, b) 3 months and (c, d) 1 year after endovascular repair showing successful and durable treatment with shrinkage of the aneurysm
Discussion
To the best of our knowledge, this is the first reported use of a custom-made double inner-branched
thoracic aortic endograft for treatment of
Salmonella-related mycotic aortic arch aneurysm. In
septic and frail patients, a custom-made endovascular
device should not generally be first-line treatment as
the manufacturing time may take up to a few months.
However, in our patient, urgency was emphasised
and availability of the stent-graft expedited.
Conventional open repair has always been the
gold standard therapy for mycotic aortic aneurysms,
but endovascular stent grafts may be a temporising
or permanent option in critically ill patients who will
not tolerate open surgery.1 2 Custom-made branched
thoracic endovascular aortic repair now adds to the
armamentarium of options. The use of custom-made
inner-branched thoracic endografts is technically
challenging and requires endovascular expertise and
experience. Meticulous preoperative planning with
analysis using the iNtuition workstation (TeraRecon,
San Mateo [CA], US) is paramount, with reference to
the characteristics of the proximal and distal landing
zones in relation to the diameter, angulation, and
length of the supra-aortic arteries. The cervical left
CCA to left subclavian artery bypass debranching
procedure can be a staged or simultaneous
procedure. The operative technique is well described
in published literature.3 4
As with most endovascular aortic arch repairs,
the most feared complication is of stroke that can
occur when atherosclerotic or gaseous emboli are
released from the arch or proximal supra-aortic
branches during wire and graft manipulation,
from clamping of carotid arteries, or due to peri-operative
fluctuation of blood pressure. Another
major concern after stenting the ascending aorta
is the risk of retrograde type A dissection, which
can be mitigated by controlled hypotension during
the deployment of the stent graft. Care must also
be taken to not cover the orifices of the coronary
arteries with the stent graft.
Off-the-shelf solutions for single and double
inner-branched aortic arch endografts are currently
under development and were not available at the time of preparation of this case report. The
use of a custom-made thoracic endograft is a
major development for these patients who would
otherwise require traditional open repair, frozen
elephant trunk procedure, or hybrid procedures.
Frail elderly patients with co-morbidities or prior
sternotomies would be denied surgery as they
would not tolerate extracorporeal cardiopulmonary
bypass with deep hypothermic circulatory arrest.
Endovascular experience and technical support are
important as the access vessel is remote to the arch.
There is often a fine balance between the procedure
and maintenance of cerebral perfusion. Comparing
non-custom chimney and custom graft for arch
pathology, O’Callaghan et al5 showed that mortality
was higher in the non-custom group (7% vs 18%), and a trend favouring better durability of fenestrated
grafts for sealing and re-intervention rates was noted.
All patients should have regular CT surveillance to
monitor durability and exclude aneurysm-related
complications. Long-term postoperative antibiotic
therapy is also important since endovascular options
preclude debridement of infected tissue.
This new technique involving a custom-made
double inner-branched aortic arch endograft can
be considered in patients with mycotic aneurysms
of the thoracic arch, with favourable and durable
results.
Author contributions
All authors contributed to the concept or design of the study, acquisition of the data, analysis or interpretation of the
data, drafting of the manuscript, and critical revision of the
manuscript for important intellectual content. All authors
had full access to the data, contributed to the study, approved
the final version for publication, and take responsibility for its
accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki. The patient provided written informed consent for
all procedures.
References
1. Chan YC, Morales JP, Taylor PR. The management of mycotic aortic aneurysms: is there a role for endoluminal
treatment? Acta Chir Belg 2005;105:580-7. Crossref
2. Taylor PR, Chan YC. Endovascular treatment in the management of mycotic aortic aneurysms. In: Thompson
MM, Morgan RA, Matsumura JS, Sapoval M, Loftus IM,
editors. Endovascular Intervention for Vascular Disease.
Principles and Practice. Boca Raton: Taylor & Francis
Group; 2008: 235-42.
3. Fiorucci B, Tsilimparis N, Rohlffs F, Heidemann F, Debus ES, Kölbel T. How to confirm catheterization of inner branches
in aortic endografting: The Universal Flush Test. J Endovasc
Ther 2017;24:539-41. Crossref
4. Tsilimparis N, Detter C, Law Y, et al. Single-center experience with an inner branched arch endograft. J Vasc
Surg 2019;69:977-85.e1. Crossref
5. O’Callaghan A, Mastracci TM, Greenberg RK, Eagleton MJ, Bena J, Kuramochi Y. Outcomes for supra-aortic branch
vessel stenting in the treatment of thoracic aortic disease. J
Vasc Surg 2014;60:914-20. Crossref

