Hong Kong Med J 2021 Dec;27(6):437–43 | Epub 3 Dec 2021
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Effects of enhanced recovery after surgery practices on postoperative recovery and length of stay after unilateral primary total hip or knee arthroplasty in a private hospital
Marvin MT Chung, MB, BS, MRCSEd1; Jacobus KF Ng, FHKAM (Anaesthesiology)2,3; FY Ng, FHKCOS, FHKAM (Orthopaedic Surgery)2; PK Chan, FHKCOS, FHKAM (Orthopaedic Surgery)1; KY Chiu, FHKCOS, FHKAM (Orthopaedic Surgery)3,4
1 Department of Orthopaedics and Traumatology, Queen Mary Hospital, Hong Kong
2 Private practice, Hong Kong
3 Hong Kong Sanatorium & Hospital, Hong Kong
4 Department of Orthopaedics and Traumatology, The University of Hong Kong, Hong Kong
Corresponding author: Dr Marvin MT Chung (marvinchung@ortho.hku.hk)
Abstract
Introduction: Enhanced recovery after surgery
(ERAS) practices improve postoperative recovery
and reduce postoperative length of stay (LOS) in
patients undergoing primary total hip arthroplasty
(THA) or total knee arthroplasty (TKA). Our study
investigated whether these promising results could
be reproduced in a private hospital setting.
Methods: In total, 228 patients were included in
the study cohort: the conventional group comprised
117 patients from 2012 to 2014, while the ERAS
group comprised 111 patients from 2017 to 2018.
All patients had undergone unilateral primary THA
or TKA at a private hospital in Hong Kong. The
outcome was postoperative LOS; factors affecting
LOS were also investigated.
Results: No significant differences were found in
any baseline parameters between the two groups of
patients. The mean LOS was significantly shorter
in the ERAS group than in the conventional group
(3.28 ± 1.04 vs 5.16 ± 2.06 days, P<0.001). Moreover,
a significantly greater proportion of patients could
be discharged on or before postoperative day 3 in the
ERAS group, compared with the conventional group
(77.5% vs 13.7%, P<0.001). A significant difference in LOS was observed between general ward and
private ward patients (3.06 ± 0.59 vs 3.66 ± 1.46 days,
P=0.003). Sex, age, and nature of surgery (TKA vs
THA) did not have significant effects on LOS.
Conclusions: The ERAS practices yielded a
significant improvement in postoperative LOS,
compared to conventional practices, among patients
who underwent unilateral primary THA or TKA in
a private hospital.
New knowledge added by this study
- Enhanced recovery after surgery (ERAS) practices in total joint arthroplasty improve postoperative length of stay in the private hospital setting, similar to previous findings in public joint replacement centres.
- Among patients who underwent unilateral primary total hip or knee arthroplasty in a private hospital, postoperative length of stay was lower for patients in general wards than for patients in private wards.
- Standardised ERAS practices could be implemented as a protocol by private hospitals in Hong Kong.
- Although full ERAS implementation may be difficult to achieve in a short period of time, gradual addition of ERAS components could improve patient outcomes in private hospitals.
Introduction
Enhanced recovery after surgery (ERAS) practices
were developed in the 1990s whereby multiple
modalities of intervention1 were introduced
perioperatively to improve postoperative recovery,2
reduce length of stay (LOS),3 and lower the
incidence of perioperative morbidity.4 These
practices have been widely adopted in many
surgical fields,5 6 7 including orthopaedics.8 Further enhancements of postoperative pain management,
venous thromboembolism prophylaxis, and early
mobilisation have led to encouraging results in
primary total hip arthroplasty (THA) and total knee
arthroplasty (TKA); such results have included earlier
recovery,9 LOS reduction,10 improved function,11 and
lower venous thromboembolism incidence12 without
declines in patient satisfaction, postoperative
complication rate,13 or cost.14 The development of ERAS practices has matured with the progressive
introduction of standardised clinical pathways for
all patients receiving THA or TKA,15 also referred as
fast-track hip and knee arthroplasty.16 These ERAS
practices have become the standard of care in most
joint replacement centres.17 18
Because of the ageing population and increasing
incidence of degenerative joint disease,19 the wait
time for elective TKA in a public joint replacement
service can reach 5 years in Hong Kong20; thus,
many patients visit private orthopaedic surgeons for
earlier surgery. Despite the presence of robust joint
replacement options in the Hong Kong orthopaedic
community, there remain differences between
public and private hospital settings in terms of the
environment, perioperative medical care, and service
availability. To our knowledge, no studies have been
published regarding the effects of ERAS practices
on LOS after lower limb total joint arthroplasty, or
whether ERAS practices could be implemented as a
standardised protocol by private hospitals in Hong
Kong.
Therefore, this study investigated whether
the promising results of ERAS practices could be
reproduced in private hospitals by comparison of
LOS among patients who underwent unilateral
primary THA or TKA by a single surgeon at Hong
Kong Sanatorium & Hospital, a private hospital in
Hong Kong, before and after the implementation of
ERAS.
Methods
Patients
Patients who had undergone unilateral primary THA or TKA by the senior author (KYC) at Hong
Kong Sanatorium & Hospital, Hong Kong, were
included in the study cohort. Patients with revision
arthroplasty, one-stage bilateral arthroplasty, and
unicompartmental knee arthroplasty were excluded.
Because ERAS practices were progressively
implemented from 2015 to 2016, we allocated
patients who were treated from 2012 to 2014 into the
conventional group and patients who were treated
from 2017 to 2018 into the ERAS group.
Similarities between enhanced recovery after
surgery and conventional practices
Our ERAS practices were generally similar to
conventional practices. Most patients underwent
surgery on the morning after an evening admission.
Most patients received spinal anaesthesia unless
contra-indicated (eg, ankylosing spondylitis, severe
spinal deformity, coagulopathy, or fixed cardiac
output state); routine sedation (using intravenous
midazolam and propofol) was also conducted
to improve patient comfort. Cementless THA
systems, either a Pinnacle acetabular cup with a
Summit femoral stem (DePuy, Warsaw [IN], US) or
an R3 acetabular cup with a Synergy femoral stem
(Smith & Nephew, Auckland, New Zealand), were
implemented by means of a posterolateral approach.
Total knee arthroplasty was performed using a
medial parapatellar approach with thigh tourniquet
and conventional instruments. Cemented rotating
platform TKA systems were used: either a Legacy
Posterior Stabilised Flex Mobile prosthesis (Zimmer,
Warsaw [IN], US) or an Attune prosthesis (DePuy).
A Foley urinary catheter was inserted only on
urinary retention with bladder volume of >800 mL.21
Prophylactic antibiotics were administered on
the induction of anaesthesia, then continued for
2 days after surgery. Prophylaxis against venous
thromboembolism, both pharmacological (with
subcutaneous enoxaparin) and mechanical (with
a sequential compression device), was routinely
implemented. Patients were discharged home when
they could safely exit their beds without assistance
and stably walk using an assistive device without any
sign of complications.
Differences between enhanced recovery after
surgery and conventional practices
Steroid administration
When using ERAS practices, a higher dose of
intravenous steroid is administered on the
induction of anaesthesia for both THA and TKA. In
the conventional group, 4 to 8 mg of dexamethasone
was administered; in the ERAS group, 125 mg
of methylprednisolone (equivalent to 25 mg of
dexamethasone) was administered instead.22 Notably,
high-dose glucocorticoids before arthroplasty are reportedly safe and recommended for routine use.23
Management of pain, nausea, and vomiting
In the conventional group, no standard pain control
regimen was established. Pain medications were
prescribed at the discretion of anaesthetists or
surgeons, including the use of femoral nerve block
and postoperative patient-controlled analgesia pump.
Pain management was standardised and optimised in
the ERAS group, particularly for patients undergoing
TKA. Pre-emptive analgesia was implemented, such
that patients routinely began oral pregabalin and
transdermal buprenorphine patch treatments before
surgery. Preventive analgesia was also employed
both intra- and post-operatively. A periarticular
“cocktail” injection of local infiltrative analgesia24—consisting of ropivacaine, ketorolac, and 1:1000
adrenaline—was injected into the posterior joint
capsule before implantation of the prosthesis; it was
also injected into the subcutaneous layer anteriorly
and intra-articularly during wound closure. After surgery, patients received multimodal
oral analgesia including regular cyclooxygenase-2
inhibitors or non-steroidal anti-inflammatory drugs,
pregabalin, and paracetamol. Buprenorphine patch
treatment was maintained for 5 to 7 days. Patient-controlled
analgesia was omitted when using ERAS
practices. In contrast, the pain control requirement
was lower for patients undergoing THA. In both
conventional and ERAS groups, local anaesthetic
(bupivacaine) was injected into the subcutaneous
plane before skin closure, while oral paracetamol
was prescribed after surgery. After discharge from the hospital,
patients who underwent TKA were administered
non-steroidal anti-inflammatory drugs, pregabalin,
and paracetamol for up to 5 weeks after surgery;
most patients undergoing THA were prescribed
paracetamol alone.
Prophylactic intravenous palonosetron was
routinely administered to prevent postoperative
nausea and vomiting; intravenous metoclopramide
was used to manage breakthrough symptoms.
Blood management
Tranexamic acid was routinely used in the ERAS
group to minimise bleeding and the need for
transfusion. For patients undergoing TKA, 1 g of
tranexamic acid was injected intra-articularly after
deep layer closure. No routine use of tranexamic acid
was adopted in conventional practices. A deep drain
was used when adhering to conventional practices
but not when adhering to ERAS practices. For
patients undergoing THA, intravenous tranexamic
acid was administered at the same time as induction of
anaesthesia; a deep drain was also used and removed
the next morning.
Sleep management
While hypnotics were only administered on
request when in the conventional group, patients
in the ERAS group were routinely prescribed
hypnotics the night before surgery and the first 2 to 3 days after surgery. This helped patients in the ERAS
group to comply with the rehabilitation programme
after surgery.
Same-day rehabilitation
Same-day or day-zero rehabilitation was
implemented in the ERAS group. Patients in the
conventional group had bed rest on the day of
surgery, then began mobilisation on postoperative
day 1. Conversely, patients in the ERAS group who
underwent morning surgery were encouraged to
mobilise in the afternoon or evening on the same
day, under physiotherapist supervision.
Outcomes
The outcome was postoperative LOS, which was
denoted by the number of days after surgery when the patient was discharged from the hospital. The day of surgery was regarded as
postoperative day 0. Discharge criteria remained
consistent throughout the study period (ie, safe
exit from bed without assistance and stable walking
using an assistive device), as described above. The
proportion of patients discharged on or before
postoperative day 3 in each group was compared.
We also investigated the effects of age, sex, nature of
surgery (THA versus TKA), and class of hospital bed
(general versus private ward) on LOS.
Statistical analysis
Patient data were anonymously entered into an
encrypted file to ensure privacy. Data analysis
was performed using SPSS (Window version 26.0;
IBM Corp, Armonk [NY], US). The Chi squared
test, independent samples t test with two-tailed
significance, and one-way analysis of variance
were used for comparisons. A P value of <0.05 was
considered statistically significant.
Results
Baseline parameters
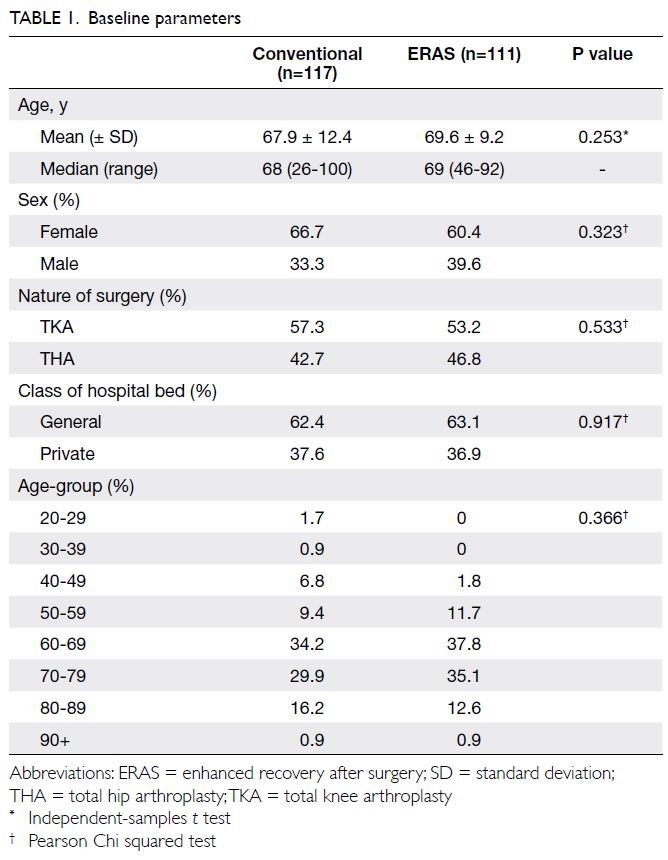
In total, 228 patients were included: 117 in the
conventional group and 111 in the ERAS group.
The mean and median ages did not significantly
differ between the conventional and ERAS groups
(Table 1). Most patients were aged between 50 and
89 years (89.7% in the conventional group and 97.2%
in the ERAS group); however, the distribution of
ages did not significantly differ between groups. The
distributions of sex, nature of surgery, and class of
hospital bed also did not significantly differ between
the conventional and ERAS groups (Table 1).
Outcome
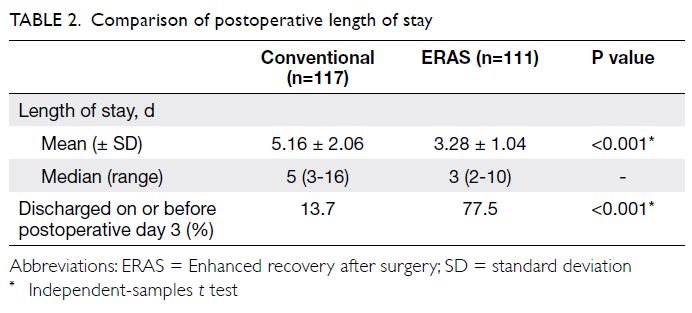
The mean LOS significantly improved from
5.16 ± 2.06 days to 3.28 ± 1.04 days (P<0.001) after
ERAS implementation (Table 2). Patients discharged
on or before postoperative day 3 comprised 13.7%
of the conventional group and 77.5% of the ERAS
group (P<0.001).
Factors affecting postoperative length of stay
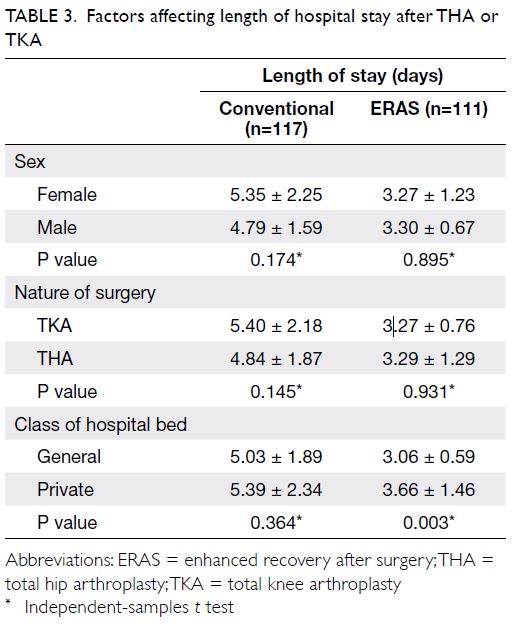
Subgroup analysis was performed to examine the
effects of sex, nature of surgery, class of hospital bed
(Table 3), and age-group (Fig) on LOS.
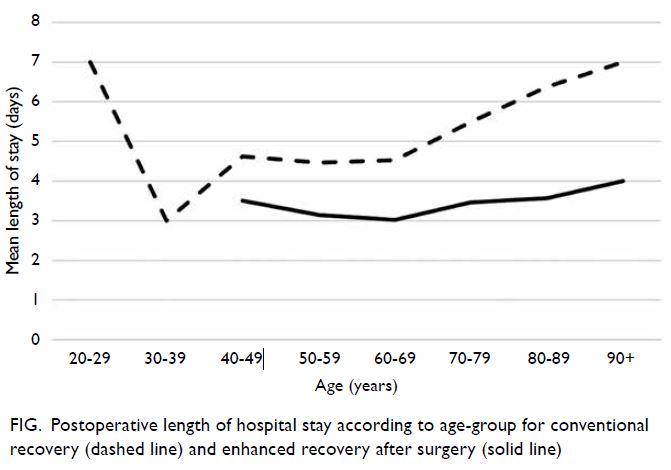
Figure. Postoperative length of hospital stay according to age-group for conventional recovery (dashed line) and enhanced recovery after surgery (solid line)
In the conventional group, there were no
significant differences in mean LOS between female
and male patients, patients receiving TKA and
patients receiving THA, or general ward and private
ward patients (Table 3). One-way analysis of variance
showed a significant difference in mean LOS among
age-groups (F [7, 109]=2.58, P=0.017) [Fig]. The
mean LOS generally increased as age increased
from the third decade (3 days) to the ninth decade
(7 days); however, two patients in the 20-29 age-group
had exceptionally long hospital stays.
In the ERAS group, there were no significant
differences in mean LOS between female and male
patients or between patients receiving TKA and
patients receiving THA (Table 3). One-way analysis
of variance showed that age did not have a significant
effect on the mean LOS (F [5, 105]=1.13, P=0.348)
[Fig]. However, the mean LOS significantly differed
between general ward and private ward patients
(3.06 ± 0.59 vs 3.66 ± 1.46 days, P=0.003) [Table 3].
Complication and re-admission
No postoperative complications or instances
of 30-day re-admission were observed among
patients who underwent TKA. Among patients
who underwent THA, three (two from the
conventional group, one from the ERAS group)
had complications. In the conventional group, one patient with spondyloepiphyseal dysplasia
experienced dislocation during in-patient stay,
which required closed reduction; one patient
experienced dislocation during postoperative week 3,
which required re-admission and revision to offset
the liner and a longer neck hip ball to improve soft
tissue tension. In the ERAS group, one patient had
periprosthetic femoral fracture after an accidental
fall on postoperative day 13, which required re-admission
with revision to the long cementless stem,
as well as cable fixation. No patients in either group
experienced postoperative wounds or periprosthetic
infections.
Discussion
Despite more efficient service provision,
postoperative LOS in private hospitals might be
limited by confounders that surgeons cannot control
(eg, patient preference and financial factors).25
Nevertheless, it was unsurprising that our results
were consistent with previous literature: ERAS
practices are effective for reducing the LOS after
unilateral primary arthroplasty.
Regarding factors that affect postoperative
LOS, a significant difference in the mean LOS was
observed between general ward and private ward
patients in the ERAS group. In public hospitals, the
LOS among patients with worse socio-economic
backgrounds is often limited by inadequate social
support from family after discharge26 or a suboptimal
home environment (eg, non-lift landing flats in
older urban buildings).27 While placement issues are
rarely problematic for patients in private hospitals,28
a possible explanation for the difference in LOS
between general ward and private ward patients,
where the cost difference is on average 5 times
higher, is that patients with better socio-economic
backgrounds may have higher expectations for
surgical outcomes29; thus, they may tolerate
longer hospital stays for rehabilitation, despite the
higher costs of such stays. Private insurance is also
reportedly an independent predictor of discharge
delay despite objective readiness for discharge30;
however, we presumed that the effect of insurance
was not applicable in the present study because fewer
than 10% of patients in our cohort had no insurance
coverage. Furthermore, no significant differences in
the mean LOS were noted with regard to the nature
of surgery, sex, or age in the ERAS group. These
findings may be related to the use of standardised
ERAS practices and perioperative protocols, which
have minimised variation in patient management.31
The implementation of ERAS practices in
private hospitals is potentially beneficial to all
stakeholders (including hospital administrators)
because it facilitates hospital bed availability, while
reducing costs via shorter convalescence duration
and reduced morbidity.32 However, there are some important challenges for surgeons who wish to
initiate ERAS practices in private centres. These
challenges include occasional requirements for
minor alterations in ward environments, changes
in anaesthesia technique, rapid turnover of in-house
surgical staff, and noncompliance with ERAS
practices.33 Furthermore, a large caseload might be
necessary to attract a dedicated multidisciplinary
team for the sustainable development of ERAS
practices in private centres. While it may be
challenging to achieve full ERAS implementation
in a short period of time, the stepwise addition of
ERAS components might improve patient outcomes
in private hospitals.34
There were some limitations in this study.
First, this study used a retrospective design without
randomisation, which may have led to imbalance and
bias in the results. Second, this study only involved
patients from a single surgeon; thus, the sample
size was small. Third, differences in functional
status and co-morbidities were not considered in
the analysis, as the electronic health record sharing
system between public and private hospitals was
only established in 2016 so complete acquisition of
patient’s parameters was not possible. Finally, other
clinical outcome parameters and patient satisfaction
were not investigated; these will be examined in a
future study, where a thorough documentation in
patient reported outcome measure and clinician-based
outcome measure will improve the validity of
results.
In conclusion, ERAS practices produced
significant improvement in mean postoperative LOS,
compared to conventional practices, for patients
who underwent unilateral primary THA or TKA in
a private hospital. Specifically, a significantly greater
proportion of patients in the ERAS group were able to return home on or before postoperative day 3. The
findings indicate that the good outcomes of ERAS
practices in public joint replacement centres can
be reproduced in private hospitals with sufficient
caseloads and consistent implementation of ERAS
practices.
Author contributions
Concept or design: KY Chiu.
Acquisition of data: MMT Chung.
Analysis or interpretation of data: MMT Chung.
Drafting of the manuscript: MMT Chung, JKF Ng, FY Ng, PK Chan.
Critical revision of the manuscript for important intellectual content: KY Chiu.
Acquisition of data: MMT Chung.
Analysis or interpretation of data: MMT Chung.
Drafting of the manuscript: MMT Chung, JKF Ng, FY Ng, PK Chan.
Critical revision of the manuscript for important intellectual content: KY Chiu.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Declaration
The results of this study were presented in the Hong Kong Orthopaedic Association 40th Annual Congress in Hong
Kong (31 October to 1 November 2020).
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was approved by the Hong Kong Sanatorium & Hospital Medical Group Research Committee (Ref RC-2019-
25). The requirement for patient consent was waived for this
retrospective study.
References
1. Kehlet H. Multimodal approach to postoperative recovery. Curr Opin Crit Care 2009;15:355-8. Crossref
2. Kehlet H, Dahl JB. Anaesthesia, surgery, and challenges in postoperative recovery. Lancet 2003;362:1921-8. Crossref
3. Kehlet H. Fast-track hip and knee arthroplasty. Lancet 2013;381:1600-2. Crossref
4. Rogers LJ, Bleetman D, Messenger DE, et al. The impact of enhanced recovery after surgery (ERAS) protocol
compliance on morbidity from resection for primary lung
cancer. J Thoracic Cardiovasc Surg 2018;155:1843-52. Crossref
5. Geltzeiler CB, Rotramel A, Wilson C, Deng L, Whiteford MH, Frankhouse J. Prospective study of colorectal enhanced
recovery after surgery in a community hospital. JAMA
Surg 2014;149:955-61. Crossref
6. Melnyk M, Casey RG, Black P, Koupparis AJ. Enhanced
recovery after surgery (ERAS) protocols: time to change
practice? Can Urol Assoc J 2011;5:342-8. Crossref
7. Scheib SA, Thomassee M, Kenner JL. Enhanced recovery after surgery in gynecology: a review of the literature. J
Minim Invasive Gynecol 2019;26:327-43. Crossref
8. Andersen LØ, Gaarn-Larsen L, Kristensen BB, Husted H, Otte KS, Kehlet H. Subacute pain and function after fast-track
hip and knee arthroplasty. Anaesthesia 2009;64:508-13. Crossref
9. Wu CL, Raja SN. Treatment of acute postoperative pain. Lancet 2011;377:2215-25. Crossref
10. Auyong DB, Allen CJ, Pahang JA, Clabeaux JJ, MacDonald KM, Hanson NA. Reduced length of
hospitalization in primary total knee arthroplasty patients
using an updated enhanced recovery after surgery (ERAS)
pathway. J Arthroplasty 2015;30:1705-9. Crossref
11. Pua YH, Ong PH. Association of early ambulation
with length of stay and costs in total knee arthroplasty:
retrospective cohort study. Am J Phys Med Rehabil
2014;93:962-70. Crossref
12. Pearse EO, Caldwell BF, Lockwood RJ, Hollard J. Early
mobilisation after conventional knee replacement may
reduce the risk of postoperative venous thromboembolism.
J Bone Joint Surg Br 2007;89:316-22. Crossref
13. Zhu S, Qian W, Jiang C, Ye C, Chen X. Enhanced recovery
after surgery for hip mand knee arthroplasty: a systematic
review and meta-analysis. Postgrad Med J 2017;93:736-42. Crossref
14. Duncan CM, Hall Long K, Warner DO, Hebl JR. The
economic implications of a multimodal analgesic regimen
for patients undergoing major orthopaedic surgery: a
comparative study of direct costs. Reg Anesth Pain Med
2009;34:301-7. Crossref
15. Duggal S, Flics S, Cornell CN. Introduction of clinical
pathways in orthopedic surgical care: the experience of
the hospital for special surgery. In: Ronald MacKenzie C,
Cornell CN, Memtsoudis SG, editors. Perioperative Care
of the Orthopedic Patient. New York: Springer; 2014:
365-71. Crossref
16. Husted H. Fast-track hip and knee arthroplasty: clinical
and organizational aspects. Acta Orthop Suppl 2012;83:1-39. Crossref
17. Christelis N, Wallace S, Sage CE, et al. An enhanced
recovery after surgery program for hip and knee
arthroplasty. Med J Aust 2015;202:363-8. Crossref
18. Soffin EM, YaDeau JT. Enhanced recovery after surgery
for primary hip and knee arthroplasty: a review of the
evidence. Br J Anaesth 2016;117(Suppl 3):iii62-72. Crossref
19. Yan CH, Chiu KY, Ng FY. Total knee arthroplasty for
primary knee osteoarthritis: changing pattern over the past
10 years. Hong Kong Med J 2011;17:20-5.
20. Hospital Authority, Hong Kong SAR Government.
Elective total joint replacement surgery. 2019.
Available from: https://www.ha.org.hk/visitor/ha_visitor_index.asp?Content_ID=221223&Lang=EN%20G&Dimension=100&Parent_ID=214172&Ver=HTML. Accessed 25 Feb 2020. Crossref
21. Bjerregaard LS, Hornum U, Troldborg C, Bogoe S, Bagi P,
Kehlet H. Postoperative urinary catheterization thresholds
of 500 versus 800 ml after fast-track total hip and knee
arthroplasty: a randomized, open-label, controlled trial.
Anesthesiology 2016;124:1256-64. Crossref
22. Lunn TH, Kristensen BB, Andersen LØ, et al. Effect of
high-dose preoperative methylprednisolone on pain and
recovery after total knee arthroplasty: a randomized,
placebo-controlled trial. Br J Anaesth 2011;106:230-8. Crossref
23. Kehlet H, Lindberg-Larsen V. High-dose glucocorticoid
before hip and knee arthroplasty: to use or not to use-that's
the question. Acta Orthop 2018;89:477-9. Crossref
24. Ng FY, Ng JK, Chiu KY, Yan CH, Chan CW. Multimodal
periarticular injection vs continuous femoral nerve block
after total knee arthroplasty: a prospective, crossover,
randomized clinical trial. J Arthroplasty 2012;27:1234-8. Crossref
25. Badham J, Brandrup J. Length of stay comparisons for
private and public hospitals. Aust Health Rev 2000;23:162-70. Crossref
26. Freitas A, Silva-Costa T, Lopes F, et al. Factors influencing hospital high length of stay outliers. BMC Health Serv Res 2012;12:265. Crossref
27. Waring J, Marshall F, Bishop S, et al. An ethnographic study
of knowledge sharing across the boundaries between care
processes, services and organisations: the contributions
to ‘safe’ hospital discharge. Southampton (UK): NIHR
Journals Library; Sep 2014. Crossref
28. Perelman J, Closon MC. Impact of socioeconomic factors on in-patient length of stay and their consequences in per case hospital payment systems. J Health Serv Res Policy
2011;16:197-202. Crossref
29. Li X, Galvin JW, Li C, Agrawal R, Curry EJ. The impact of socioeconomic status on outcomes in orthopaedic surgery.
J Bone Joint Surg Am 2020;102:428-44. Crossref
30. Celio DA, Poggi R, Schmalzbauer M, Rosso R, Majno P,
Christoforidis D. ERAS, length of stay and private
insurance: a retrospective study. Int J Colorectal Dis
2019;34:1865-70. Crossref
31. Barbieri A, Vanhaecht K, Van Herck P, et al. Effects of
clinical pathways in the joint replacement: a meta-analysis.
BMC Med 2009;7:32. Crossref
32. Stowers MD, Lemanu DP, Hill AG. Health economics in
enhanced recovery after surgery programs. Can J Anaesth
2015;62:219-30. Crossref
33. Kahokehr A, Sammour T, Zargar-Shoshtari K, Thompson L,
Hill AG. Implementation of ERAS and how to overcome
the barriers. Int J Surg 2009;7:16-9. Crossref
34. Tan NL, Hunt JL, Gwini SM. Does implementation of
an enhanced recovery after surgery program for hip
replacement improve quality of recovery in an Australian
private hospital: a quality improvement study. BMC
Anesthesiol 2018;18:64. Crossref