Hong Kong Med J 2021 Dec;27(6):413–20 | Epub 17 Dec 2021
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Intermediate- to long-term outcomes of transvaginal mesh for treatment of Asian women with pelvic organ prolapse
Symphorosa SC Chan, MD, FRCOG; Osanna YK Wan, FHKAM (Obstetrics and Gynaecology), FHKCOG; KW Choy, MSc (Med), PhD; Rachel YK Cheung, FRCOG, FHKAM (Obstetrics and Gynaecology)
Department of Obstetrics and Gynaecology, The Chinese University of Hong Kong, Hong Kong
Corresponding author: Dr Symphorosa SC Chan (symphorosa@cuhk.edu.hk)
Abstract
Introduction: Short-term follow-up analyses
suggest that transvaginal mesh has limited
application for pelvic organ prolapse (POP)
treatment. This study evaluated the intermediate- and
long-term outcomes of transvaginal mesh
surgery.
Methods: This retrospective study included all
women who underwent transvaginal mesh surgery
in one urogynaecology centre. Inclusion criteria
were women with stage III/IV POP, age ≥65 years,
and (preferably) sexual inactivity. Concomitant
sacrospinous fixation and mid-urethral slings were
offered for stage III/IV apical POP and urodynamic
stress incontinence, respectively. Women were
followed up for 5 years. Subjective recurrence was
defined as reported prolapse symptoms. Objective
recurrence was defined as stage II prolapse or above.
Mesh complications and patient satisfaction were
reviewed.
Results: Of 183 women who underwent transvaginal
mesh surgery, 156 had ≥1 year of follow-up (mean,
50 ± 22 months). Subjective and objective recurrence
rates were 5.1% and 10.9%, respectively. The mesh
erosion rate was 9.6%; all affected women received
local oestrogen treatment or bedside surgical
excision. Three women received transobturator tension-free transvaginal tape for de novo (n=1)
or preoperative urodynamic stress incontinence
who did not undergo concomitant surgery (n=2);
14% of the women had de novo urgency urinary
incontinence. No women reported chronic pain.
Overall, 98% were ‘satisfied’ or ‘very satisfied’ with
the operation.
Conclusion: During 50 months of follow-up,
transvaginal mesh surgery for stage III/IV POP
had low subjective and objective recurrence rates.
The total re-operation rate was 9.6%. Most women
were satisfied with the operation. Based on the risk-benefit
profile, transvaginal mesh surgery may be
suitable for women who have advanced POP.
New knowledge added by this study
- In women with stage III or IV pelvic organ prolapse, transvaginal mesh surgery (with concomitant sacrospinous fixation for stage III or IV apical compartment prolapse) had low subjective (5.1%) and objective (10.9%) rates of recurrence, along with a high satisfaction rate (98%), during approximately 50 months of follow-up.
- In sexually inactive women, the transvaginal mesh erosion rate is low.
- Although some women required re-operations because of factors such as pelvic organ prolapse recurrence, stress urinary incontinence, and mesh erosion, the overall re-operation rate was 9.6%.
- In contrast to previous recommendations, transvaginal mesh surgery may be suitable for women who are sexually inactive, particularly women who have a higher risk of prolapse recurrence related to conditions such as advanced pelvic organ prolapse and levator ani muscle avulsion.
Introduction
Pelvic organ prolapse (POP) leads to considerable
symptomatic distress and reduced quality of life
among women.1 2 Large-scale studies of women in the
United States and Europe have shown that the risks
of undergoing POP or stress urinary incontinence
(SUI) surgery by 80 years of age range from 12.6% to 18.7%.3 4 5 Advanced POP stage and worse quality
of life are factors that increase the likelihood of
surgical treatment.2 Symptom resolution is the
most important goal among women who seek
consultations for POP.6 Importantly, quality of life
improves in women who undergo surgical treatment.7
However, there is a high mean recurrence rate after POP surgery: 36% after a follow-up interval of 0.1
to 10 years. Reoperation is also common (29.2%)
and the between-procedure interval decreases with
successive repairs.3 8
A systematic review and meta-analysis of
25 randomised controlled trials revealed that,
compared with native tissue repair, transvaginal
mesh surgery for anterior compartment prolapse
has reduced risks of awareness of prolapse (risk
ratio=0.66, 95% confidence interval=0.54-0.81),
recurrent prolapse (risk ratio=0.4, 95% confidence
interval=0.3-0.53), and repeat surgery for prolapse
(risk ratio=0.53, 95% confidence interval=0.31-0.88)
over 1 to 3 years of follow-up.9 However, transvaginal
mesh surgery carried an increased risk of repeat
surgery for a composite outcome of prolapse, SUI,
and mesh erosion (risk ratio=2.4, 95% confidence
interval=1.51-3.81). Considering this risk-benefit
profile, the authors concluded that transvaginal mesh
has limited utility in primary surgery; however, the
quality of analysed evidence only ranged from very
low to moderate. Among the randomised controlled
trials considered in that systematic review, only one
was conducted in Asia. Moreover, high objective
and subjective cure rates of transvaginal mesh and a
low mesh erosion rate have been reported over 5 to
7 years of follow-up, although some studies have had
a high rate of loss to follow-up.10 11 12
The present study was performed to evaluate
the long-term outcome of transvaginal mesh surgery
for advanced anterior compartment prolapse in a
tertiary centre. It also investigated the recurrence
rate and the types of postoperative complications
among women who underwent transvaginal mesh
surgery.
Methods
Patients
This was a retrospective analysis of prospectively
collected data concerning transvaginal mesh
reconstructive surgeries performed for POP
treatment from January 2008 to June 2019 in a
urogynaecology training centre. Ethics approval was
obtained (CREC 2015.125); the ethics committee
waived the requirement for informed consent. All
women who underwent transvaginal mesh surgery
in the study centre were recruited. Demographic
data, including age, parity, mode of delivery,
urinary symptoms (eg, SUI and/or urgency urinary
incontinence [UUI]), and symptoms of prolapse were
collected during the first consultation; the Pelvic
Organ Prolapse Quantification assessment was also
performed.13 Management options of vaginal ring
pessary and surgery were offered. For women who
chose surgery, a urodynamic study was arranged.
Transvaginal mesh surgery (ie, anterior
vaginal mesh or total vaginal mesh) was available
to women with stage III or IV anterior and apical
and posterior compartment prolapse, age ≥65 years,
and (preferably) sexual inactivity, or with recurrent
POP. Beginning in January 2013, vaginal mesh
insertion in the posterior compartment was
not performed because of published evidence
indicating no improvement from posterior vaginal
mesh, compared with native tissue repair alone.14
Transvaginal mesh was performed with concomitant
vaginal hysterectomy or a uterine-preserving
operation depending on each woman’s choice and
medical condition. In women with stage III or IV
apical compartment prolapse, concomitant bilateral
sacrospinous fixation was performed. Because
of variations in commercial product availability,
Prolift®, Perigee®, and Restorelle® were used from
2008 to 2012, 2013 to August 2017, and September
2017 to June 2019, respectively.
Surgical procedure
Women were admitted on the day of the operation.
One dose of prophylactic intravenous antibiotics
was administered on induction. The operation
was performed under either spinal or general
anaesthesia depending on each woman’s choice and
the attending anaesthetist’s assessment. For women
who chose hysterectomy, the operation began with
vaginal hysterectomy, followed by hydrodissection with adrenaline solution and midline incision over
the anterior vaginal wall. Subsequent dissection
of the bladder from the anterior vaginal wall
was performed; the sacrospinous ligament was
reached without opening the posterior vaginal wall.
Sacrospinous ligament fixation was conducted using
a Mayo-hook from 2008 to 2017; it was conducted
using a Capio device® from 2018 to 2019. Depending
on the mesh design, anterior mesh was introduced
and all arms either passed through the obturator
membranes (Prolift® and Perigee®) or were fixed to
the ipsilateral pelvic wall and sacrospinous ligament
using stitches (Restorelle®). Anterior mesh was then
attached to the bladder fascia and anterior vaginal
wall using absorbable stitches. If total vaginal
mesh was performed, the posterior vaginal wall
was opened at the midline and the sacrospinous
ligament was identified; the arms of posterior mesh
were introduced to the sacrospinous ligaments.
Cystoscopy was performed to exclude bladder injury
and confirm ureteric jets. Per rectal examination
was performed to exclude rectal perforation. Only
the edge of the vaginal epithelium was trimmed; the
anterior vaginal wall was closed by three interrupted
stitches at the distal region, followed by continuous
sutures. In the event of symptomatic posterior
compartment prolapse, posterior colporrhaphy was
performed. Concomitant continence surgery (ie,
mid-urethral sling) was performed for women with
urodynamic stress incontinence (USI). At the end
of the operation, one piece of vaginal gauze soaked
with chlorhexidine solution was packed into the
vagina and a transurethral Foley catheter was placed.
Most vaginal hysterectomies were performed by
gynaecology trainees; all procedures involving
mesh were performed by urogynaecologists or
urogynaecology subspecialty trainees under direct
supervision by urogynaecologists. Operative details
including anaesthesia type, operative time, blood
loss, and any organ injuries were collected from
electronic operative notes that were completed by
surgeons immediately after the operation.
Postoperative care and follow-up
Oral intake was resumed on the day of the operation.
Standard oral paracetamol were administered. One
course of antibiotics was administered to women
with a high risk of infection (eg, patients with diabetes
mellitus and/or a prolonged operation) and women
with postoperative fever that persisted for more than
24 hours. The vaginal gauze and Foley catheter were
removed on the day after the operation. Women
were discharged from day 1 onwards if they resumed
a normal diet, voided well, and remained afebrile.
Women were followed up once at 2 to
4 months, then annually until 5 years after surgery.
Subsequently, if they had no active pelvic floor
symptoms, they were discharged from the clinic. Earlier follow-up was offered on request.
During follow-up examinations, the attending
gynaecologist specifically asked women about
symptoms of prolapse, SUI, UUI, vaginal bleeding,
pain, and dyspareunia, as well as the severity of such
symptoms. Vaginal examinations were performed
to assess any recurrence of prolapse or mesh
erosion, in accordance with recommendations of
the International Urogynecological Association and
International Continence Society.15 16 Satisfaction
(ie, very unsatisfied, unsatisfied, satisfied, or very
satisfied) was recorded during each postoperative
visit. Subjective recurrence was defined as reported
symptoms of prolapse, vaginal bulge, or dragging
sensation. Objective recurrence was defined by the
Pelvic Organ Prolapse Quantification assessment
with any compartment reaching ≥1 cm above the
hymen (stage ≥II). In the event of mesh erosion,
the location, size, and area of mesh erosion were
recorded. Vaginal oestrogen cream was offered. The
options of conservative management or surgical
excision of exposed mesh were discussed with
women who experienced mesh erosion, depending
on the erosion severity, accompanying symptoms,
and their personal preferences.
If women reported symptoms of SUI or UUI, a
urodynamic study was offered. If USI was diagnosed,
tension-free vaginal tape surgery was offered
to women for whom pelvic floor exercises were
ineffective. Medical treatment was offered to women
with overactive bladder or detrusor overactivity.
Statistical analysis
SPSS software (Windows version 21.0; IBM Corp,
Armonk [NY], United States) was used to analyse
the collected data. Categorical data are shown
using descriptive statistics. Normally distributed
data are shown as means (standard deviations),
whereas non-normally distributed data are shown
as medians (ranges). The times to subjective and
objective recurrences were depicted using Kaplan–Meier curves. A P value of <0.05 was considered
statistically significant.
Results
Demographic characteristics, operative
data, and postoperative outcomes among all patients
In total, 183 women (mean age, 71.8 ± 8.4 years)
underwent transvaginal mesh surgery. Nearly all
were Hong Kong Chinese women, with the exception
of two who were non-Chinese Asian women. The
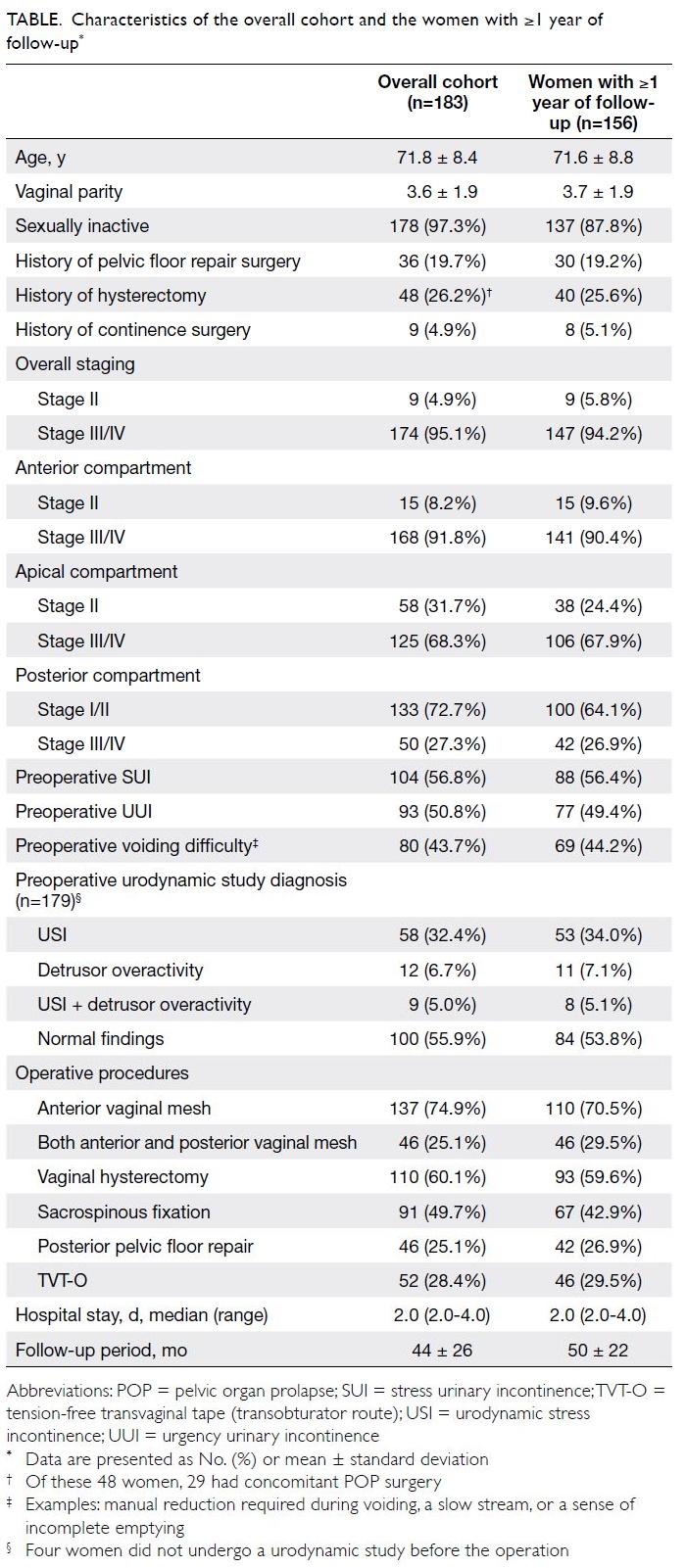
characteristics of the overall cohort are shown in the Table.
The operative procedures and hospital stay are
summarised in the Table. Forty-six (25.1%) women
had spinal anaesthesia. The mean operative time was 122.9 ± 40.7 minutes and the mean blood loss
was 193 ± 155 mL. Three (1.6%) women required
blood transfusion. One woman had bladder injury
during the trocar insertion of the anterior vaginal
mesh; the involved trocar was immediately removed
and reinserted in the correct surgical plane.
Cystoscopy showed a small perforation site at the
lateral bladder wall, but no repair was required. The
woman recovered uneventfully. One woman had a
mesh infection with abscess formation in the vulva,
requiring removal of the anterior mesh on day 18.
The infection subsided with antibiotics and drainage,
but the woman died 7 weeks after surgery because
of other medical morbidities.17
Overall, one woman was lost to follow-up
and three women, including the woman mentioned
above, died of medical diseases within 1 year; thus,
179 (97.8%) women were eligible for the postoperative
outcome analysis. Of these 179 women, 23 (12.8%)
underwent operation within 1 year prior to this
report, while 156 (87%), 113 (63%), and 77 (43%) had
completed 1, 3, and 5 years of follow-up, respectively.
The mean duration of follow-up was 50 ± 22 months.
There were no differences in demographics,
preoperative symptoms, stage and compartment of
prolapse, or operative data between the 23 women
with <1 year of follow-up and the 156 women with
≥1 year of follow-up, except for the vaginal mesh
brand (because of variations in commercial product
availability) and the duration of follow-up (Table).
Postoperative outcomes among women with
≥1 year of follow-up
Among the 156 women with ≥1 year of follow-up,
eight reported symptoms of prolapse recurrence
(subjective recurrence rate of 5.1%). Five women
had stage II POP, while three women had stage III
POP. Four women experienced recurrence in the
first year of follow-up; two, one, and one additional
women experienced recurrence in the second,
third, and fourth year of follow-up, respectively.
While five women with recurrence had conservative
treatment for POP, one woman had vaginal pessary
and two (1.3%) women had surgery to manage
prolapse recurrence. In addition, nine other women
had asymptomatic stage II POP: two had anterior
compartment prolapse and seven had posterior
compartment prolapse. The objective recurrence rate
was 10.9% (n=17). The mesh erosion rate was 9.6%
(n=15). In all, 40% of the erosions (n=6) occurred at
the posterior wall; the remaining erosions occurred
at other sites in the vagina (four anterior wall, four
vaginal vault, and one lateral wall). Most instances of
mesh erosion (n=8, 53.3%) occurred in the first year.
Ten of the 15 affected women underwent surgical
excision under local anaesthesia at the bedside;
seven, one, and two women required one, two, and
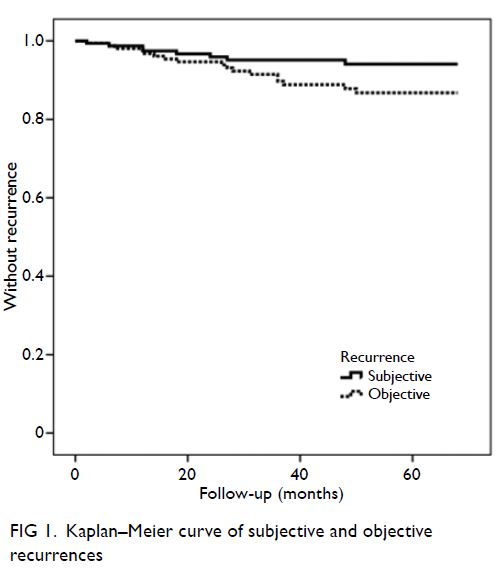
three surgical excisions, respectively. The times to subjective and objective recurrences are depicted
using Kaplan–Meier curves (Fig 1).
The preoperative and postoperative
symptoms of SUI are listed in Figure 2. Occult
USI was observed in 11 (16.2%) of 68 women who
reported no SUI before the operation. Among four
women who had occult USI and did not undergo
continence surgery, two had postoperative SUI;
they did not require surgical treatment. De novo
SUI occurred in 12 (7.7%) women. Only one (1/53,
1.9%) woman received tension-free transvaginal
tape (transobturator route) [TVT-O] for treatment
of SUI; the remaining 11 women had mild symptoms
or achieved improvement with pelvic floor exercise.
Among the 31 women who had preoperative SUI
but normal urodynamic study findings and did not
undergo continence surgery, 19 (61.2%) women
had postoperative SUI. Among them, two received
TVT-O afterwards. Overall, 22 (14%) women had de
novo UUI: seven received anticholinergics and the
remaining 15 had conservative treatment. No women
reported vaginal pain, pelvic pain, or dyspareunia.
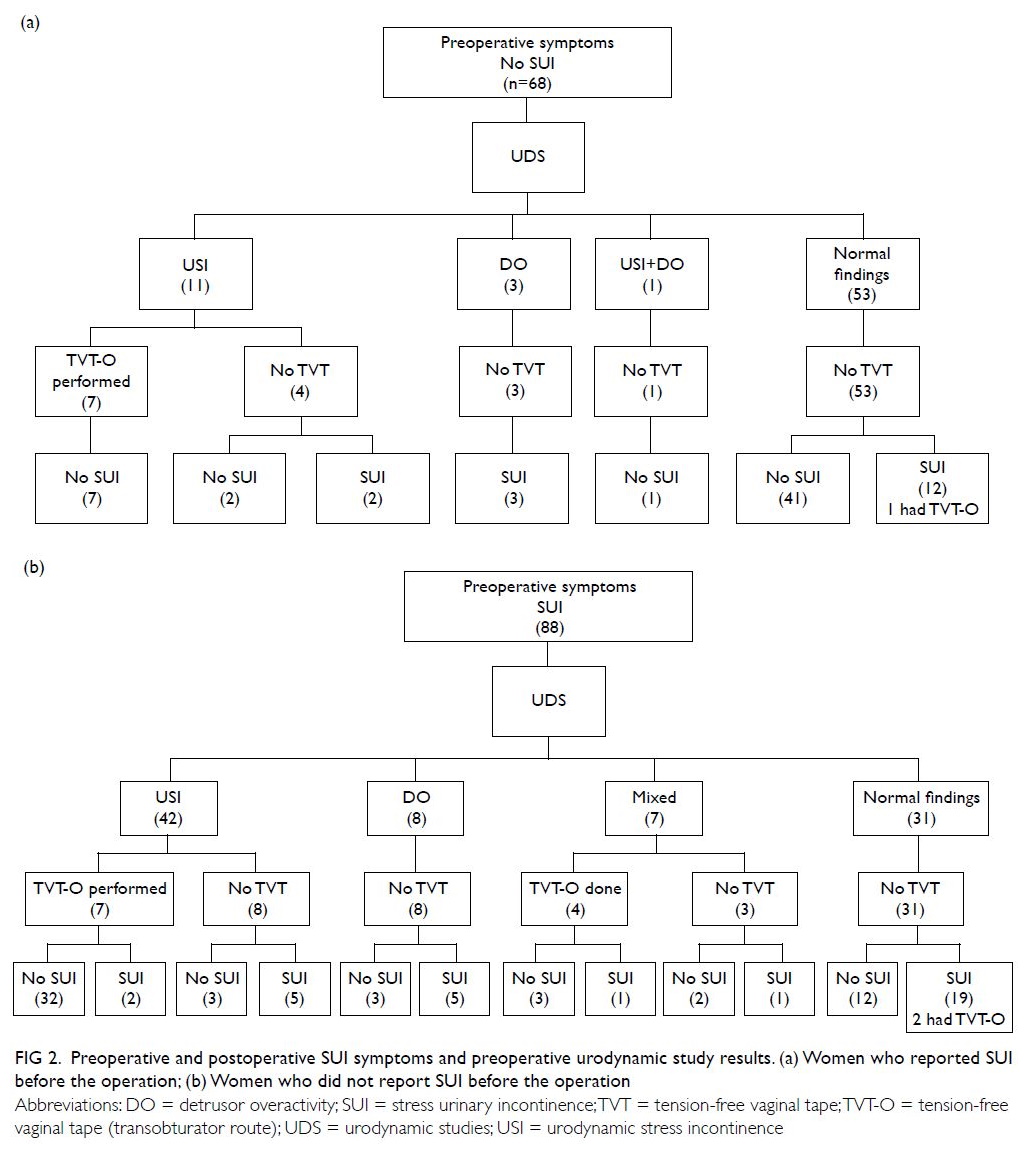
Figure 2. Preoperative and postoperative SUI symptoms and preoperative urodynamic study results. (a) Women who reported SUI before the operation; (b) Women who did not report SUI before the operation
In summary, the total re-operation rate was
9.6%: two women for recurrent POP, 10 women for
mesh erosion, three women for TVT-O, and one
woman for de novo SUI. In all, 103 (66%) women
and 50 (32.1%) women were ‘satisfied’ and ‘very
satisfied’, respectively, with the operation at their
latest follow-up examination. Three women who
ever had recurrence did not report being ‘satisfied’
or ‘very satisfied’.
Discussion
This study provided a comprehensive evaluation
of the intermediate- to long-term (ie, 3 to 5 years)
outcomes of transvaginal mesh surgery in women
with advanced POP. Risk factors for POP recurrence
reportedly include levator ani muscle avulsion
(odds ratio=2.8), preoperative stage III-IV POP
(odds ratio=2.1), family history (odds ratio=1.8),
and large hiatal area (odds ratio=1.06 per 1 cm2).8
The prevalence of levator ani muscle avulsion is
higher in women with more advanced POP: we
previously reported that 54.5% and 66.7% of women
with stage III and IV POP had levator ani muscle
avulsion, respectively.18 Although this factor was
not evaluated in the present study, we presume
that a similar proportion of our cohort would have
this condition, placing them at high risk of POP
recurrence. Indeed, transvaginal mesh repair leads
to a lower rate of anterior compartment prolapse
recurrence, compared with native tissue repair in
women with levator ani muscle avulsion.19 20
Transvaginal mesh was not recommended
in a systematic review and meta-analysis of 25
randomised controlled trials, based on its risk-benefit
profile. The risk of awareness of prolapse
was 13%; the risks of repeat surgery for prolapse and SUI were 1.8% and 2.9%, respectively.9 However, if
the transvaginal mesh treatment efficacy remains
high over a longer follow-up period and the risk of
morbidity is low, the above recommendation may not
apply to all women. In our cohort, these risks were
5.1%, 1.3%, and 1.9% for a mean follow-up period of
50 months. This indicates a tendency towards lower
POP recurrence risks in our cohort. The objective
recurrence rate of 10.6% also tended to be lower,
compared with previous studies that recruited
women who had stage II POP8, although 95% of our
women had stage III or IV POP. Our subjective and
objective recurrence rates are similar to the rates in
other Asian centres in the past decade.10 11
Apical compartment prolapse is more
prevalent among women in Hong Kong, compared
with Caucasian women.18 21 Furthermore, apical
support is important in the management of
anterior compartment prolapse, which comprises
impairment of the pubovisceral muscle and the
uterosacral and cardinal ligaments.10 22 23 Thus, we
performed concomitant sacrospinous fixation to
suspend the vaginal vault among women in this
study; this additional procedure did not increase
perioperative morbidity. This may explain why the
vaginal vault was not commonly involved in women
who had subjective or objective recurrence of POP
in the present study. Most women with objective
recurrence had stage II posterior compartment
prolapse, but they were asymptomatic.
The mesh erosion rate was 9.6%; 40% of
erosions were caused by posterior vaginal mesh.
The erosion rate for anterior vaginal mesh alone was 5.8%; this was comparable with previously
reported rates of 2.7% to 20%, with a mean of
11.1%.10 11 24 25 26 Furthermore, our rate was similar to
other Asian centres where a low mesh erosion rate
was reported.10 11 Most instances of erosion in our
study occurred within the first or second year of
follow-up; approximately two-thirds of the affected
women underwent excision of the exposed part
of the mesh and repair of the vaginal epithelium
under local anaesthesia at the bedside.17 Among
the various types of possible mesh complications,
Warembourg et al24 reported that mesh erosion was the most common complication that required
re-operation; however, it was also treated most
effectively. However, more serious complications
could occur, such as erosion into the urinary tract or
bowel.24 No instances of vaginal pain or dyspareunia
were reported in our cohort, in contrast to previous
findings26; this was presumably because we mainly
offered transvaginal mesh surgery to women who
were sexually inactive. The proportion of women
with POP who report sexual inactivity is generally
high (64%) in Hong Kong.27 Further research is
needed to determine whether ethnicity contributes to vaginal pain or dyspareunia after transvaginal mesh surgery.
Preoperative urodynamic studies showed that,
of 68 women who did not report SUI, 16% and 6% had
occult USI and other diagnoses, respectively; thus,
only 53 (78%) women had no abnormal findings. De
novo SUI occurred in 12 of these 53 women (7.7%
of all 156 women with ≥1 year of follow-up); only
one woman requested continence surgery. Although
some women reported symptoms of SUI, our
policy was not to offer continence surgery if no USI
was evident during the urodynamic study. Of the
remaining 31 of 53 women with no abnormal findings,
only two subsequently required continence surgery.
Overall, repeat surgery for SUI only occurred in
three (1.9%) women; we regarded this as a low risk of
repeat surgery. Preoperative urodynamic studies and
our more conservative approach (ie, not frequently
offering continence surgery) might have reduced the
risk of long-term complications. However, treatment
was offered to women with preoperative clinically
bothersome USI. Women who received concomitant
TVT-O were satisfied with this management.
This study had some limitations. First, this
was a single-centre study with a moderate sample
size. However, the data were collected prospectively
using a standardised form. Second, a health-related
quality of life questionnaire was not used because
validated questionnaires were unavailable when
transvaginal mesh surgery first began in our centre;
thus, no data were available for some women.1 We
plan to investigate these data in a future study.
Finally, the effects of sexual function on the surgical
outcomes were not explored because most women
in this cohort were sexually inactive. We did not
recommend transvaginal mesh surgery to women
who were sexually active because there were
increased risks of mesh erosion and dyspareunia.
Conclusion
Women with stage III or IV POP experienced a
benefit from transvaginal anterior mesh surgery (and
concomitant sacrospinous fixation if concomitant
stage III/IV apical compartment prolapse) with
low risks of subjective recurrence of POP (5.1%),
objective recurrence of POP (10.9%), and re-operation
for POP recurrence (1.3%) at a mean
follow-up interval of 50 months. Although some
women required re-operations because of various
factors (eg, POP recurrence, SUI, and mesh erosion),
the overall re-operation rate was 9.6%. Most
women were satisfied or highly satisfied with the
transvaginal mesh surgery. This type of surgery may
be suitable for women with POP who are sexually
inactive, particularly women who have a higher risk
of recurrence related to conditions such as advanced
POP and levator ani muscle avulsion.
Author contributions
Concept or design: All authors.
Acquisition of data: SSC Chan, OYK Wan, RYK Chung.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: SSC Chan.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: SSC Chan, OYK Wan, RYK Chung.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: SSC Chan.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors would like to thank Miss Loreta Lee for data
collection and data entry for this research.
Declaration
Portions of the results were presented in the 26th Asia and Oceania Federation of Obstetrics and Gynecology (AOFOG)
Congress in the Philippines in 2019, during a talk that received
the “Best Oral Presentation” award in the Urogynaecology
session.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Ethics approval was obtained from The Joint Chinese
University of Hong Kong–New Territories East Cluster
Clinical Research Ethics Committee (Ref: CREC 2015.125).
The requirement for written informed consent was waived by
the ethics board.
References
1. Chan SS, Cheung RY, Yiu AK, et al. Chinese validation of pelvic floor distress inventory and pelvic floor impact
questionnaire. Int Urogynecol J 2011;22:1305-12. Crossref
2. Chan SS, Cheung RY, Yiu KW, Lee LL, Pang AW, Chung TK.
Symptoms, quality of life, and factors affecting women’s
treatment decisions regarding pelvic organ prolapse. Int
Urogynecol J 2012;23:1027-33. Crossref
3. Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse
and urinary incontinence. Obstet Gynecol 1997;89:501-6. Crossref
4. Wu JM, Matthews CA, Conover MM, Pate V, Funk MJ. Lifetime risk of stress urinary incontinence or pelvic organ
prolapse surgery. Obstet Gynecol 2014;123:1201-6. Crossref
5. Løwenstein E, Ottesen B, Gimbel H. Incidence and lifetime risk of pelvic organ prolapse surgery in Denmark from
1977 to 2009. Int Urogynecol J 2015;26:49-55. Crossref
6. Lowenstein L, FitzGerald MP, Kenton K, et al. Patient-selected goals: the fourth dimension in assessment of pelvic
floor disorders. Int Urogynecol J Pelvic Floor Dysfunct
2008;19:81-4. Crossref
7. Chan SS, Cheung RY, Lai BP, Lee LL, Choy KW, Chung TK. Responsiveness of the Pelvic Floor Distress Inventory and Pelvic Floor Impact Questionnaire in women undergoing
treatment for pelvic floor disorders. Int Urogynecol J
2013;24:213-21. Crossref
8. Friedman T, Eslick GD, Dietz HP. Risk factors for prolapse recurrence: systematic review and meta-analysis. Int
Urogynecol J 2018;29:13-21. Crossref
9. Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Marjoribanks J. Transvaginal mesh or grafts
compared with native tissue repair for vaginal prolapse.
Cochrane Database Syst Rev 2016;(2):CD012079. Crossref
10. Lo TS, Pue LB, Tan YL, Wu PY. Long-term outcomes of synthetic transobturator nonabsorbable anterior
mesh versus anterior colporrhaphy in symptomatic,
advanced pelvic organ prolapse surgery. Int Urogynecol J
2014;25:257-64. Crossref
11. Dong S, Zhong Y, Chu L, Li H, Tong X, Wang J. Agestratified
analysis of long-term outcomes of transvaginal
mesh repair for treatment of pelvic organ prolapse. Int J
Gynecol Obstet 2016;135:112-6. Crossref
12. Meyer I, McGwin G, Swain TA, Alvarez MD, Ellington DR,
Richter HE. Synthetic graft augmentation in vaginal
prolapse surgery: long-term objective and subjective
outcomes. J Minim Invasive Gynecol 2016;23:614-21. Crossref
13. Bump RC, Mattiasson A, Bø K, et al. The standardization
of terminology of female pelvic organ prolapse and pelvic
floor dysfunction. Am J Obstet Gynecol 1996;175:10-7. Crossref
14. Maher C, Feiner B, Baessler K, Schmid C. Surgical
management of pelvic organ prolapse in women. Cochrane
Database Syst Rev 2013;(4):CD004014. Crossref
15. Haylen BT, Freeman RM, Swift SE, et al. An International
Urogynecological Association (IUGA)/International
Continence Society (ICS) joint terminology and
classification of the complications related directly to the
insertion of prostheses (meshes, implants, tapes) & grafts
in female pelvic floor surgery. Int Urogynecol J 2011;22:3-15. Crossref
16. Toozs-Hobson P, Freeman R, Barber M, et al. An
International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the
terminology for reporting outcomes of surgical procedures
for pelvic organ prolapse. Int Urogynecol J 2012;23:527-35. Crossref
17. Wan OY, Chan SS, Cheung RY, Chung TK. Mesh-related complications from reconstructive surgery for pelvic organ
prolapse in Chinese patients in Hong Kong. Hong Kong
Med J 2018;24:369-77. Crossref
18. Yu CH, Chan SS, Cheung RY, Chung TK. Prevalence of
levator ani muscle avulsion and effect on quality of life
in women with pelvic organ prolapse. Int Urogynecol J
2018;29:729-33. Crossref
19. Wong V, Shek KL, Goh J, Krause H, Martin A, Dietz HP.
Cystocele recurrence after anterior colporrhaphy with
and without mesh use. Eur J Obstet Gynecol Reprod Biol
2014;172:131-5. Crossref
20. Rodrigo N, Wong V, Shek KL, Martin A, Dietz HP. The use
of 3-dimensional ultrasound of the pelvic floor to predict
recurrence risk after pelvic reconstructive surgery. Aust N
Z J Obstet Gynaecol 2014;54:206-11. Crossref
21. Cheung RY, Chan SS, Shek KL, Chung TK, Dietz HP.
Pelvic organ prolapse in Caucasian and Asian women:
a comparative study. Ultrasound Obstet Gynecol
2019;53:541-5. Crossref
22. Chen L, Ashton-Miller JA, Hsu Y, DeLancey JO. Interaction
among apical support, levator ani impairment, and anterior
vaginal wall prolapse. Obstet Gynecol 2006;108:324-32. Crossref
23. Stanford EJ, Cassidenti A, Moen MD. Traditional native
tissue versus mesh-augmented pelvic organ prolapse
repairs: providing an accurate interpretation of current
literature. Int Urogynecol J 2012;23:19-28. Crossref
24. Warembourg S, Labaki M, de Tayrac R, Costa P, Fatton B.
Reoperations for mesh-related complications after pelvic
organ prolapse repair: 8-year experience at a tertiary
referral center. Int Urogynecol J 2017;28:1139-51. Crossref
25. Deffieux X, de Tayrac R, Huel C, et al. Vaginal mesh erosion
after transvaginal repair of cystocele using Gynemesh or
Gynemesh-Soft in 138 women: a comparative study. Int
Urogynecol J Pelvic Floor Dysfunct 2007;18:73-9. Crossref
26. Hüsch T, Mager R, Ober E, Bentler R, Ulm K, Haferkamp A.
Quality of life in women of non-reproductive age with
transvaginal mesh repair for pelvic organ prolapse: a
cohort study. Int J Surg 2016;33:36-41. Crossref
27. Cheung RY, Lee JH, Lee LL, Chung TK, Chan SS. Vaginal
pessary in women with symptomatic pelvic organ prolapse:
a randomized controlled trial. Obstet Gynecol 2016;128:73-80. Crossref